Phosphorus Metabolism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Phosphate Solubilizing Bacteria to Leach Rare Earth Elements from Monazite-Bearing Ore
Minerals 2015, 5, 189-202; doi:10.3390/min5020189 OPEN ACCESS minerals ISSN 2075-163X www.mdpi.com/journal/minerals Article Use of Phosphate Solubilizing Bacteria to Leach Rare Earth Elements from Monazite-Bearing Ore Doyun Shin 1,2,*, Jiwoong Kim 1, Byung-su Kim 1,2, Jinki Jeong 1,2 and Jae-chun Lee 1,2 1 Mineral Resources Resource Division, Korea Institute of Geoscience and Mineral Resources (KIGAM), Gwahangno 124, Yuseong-gu, Daejeon 305-350, Korea; E-Mails: [email protected] (J.K.); [email protected] (B.K.); [email protected] (J.J.); [email protected] (J.L.) 2 Department of Resource Recycling Engineering, Korea University of Science and Technology, Gajeongno 217, Yuseong-gu, Daejeon 305-350, Korea * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +82-42-868-3616. Academic Editor: Anna H. Kaksonen Received: 8 January 2015 / Accepted: 27 March 2015 / Published: 2 April 2015 Abstract: In the present study, the feasibility to use phosphate solubilizing bacteria (PSB) to develop a biological leaching process of rare earth elements (REE) from monazite-bearing ore was determined. To predict the REE leaching capacity of bacteria, the phosphate solubilizing abilities of 10 species of PSB were determined by halo zone formation on Reyes minimal agar media supplemented with bromo cresol green together with a phosphate solubilization test in Reyes minimal liquid media as the screening studies. Calcium phosphate was used as a model mineral phosphate. Among the test PSB strains, Pseudomonas fluorescens, P. putida, P. rhizosphaerae, Mesorhizobium ciceri, Bacillus megaterium, and Acetobacter aceti formed halo zones, with the zone of A. -

Prebiological Evolution and the Metabolic Origins of Life
Prebiological Evolution and the Andrew J. Pratt* Metabolic Origins of Life University of Canterbury Keywords Abiogenesis, origin of life, metabolism, hydrothermal, iron Abstract The chemoton model of cells posits three subsystems: metabolism, compartmentalization, and information. A specific model for the prebiological evolution of a reproducing system with rudimentary versions of these three interdependent subsystems is presented. This is based on the initial emergence and reproduction of autocatalytic networks in hydrothermal microcompartments containing iron sulfide. The driving force for life was catalysis of the dissipation of the intrinsic redox gradient of the planet. The codependence of life on iron and phosphate provides chemical constraints on the ordering of prebiological evolution. The initial protometabolism was based on positive feedback loops associated with in situ carbon fixation in which the initial protometabolites modified the catalytic capacity and mobility of metal-based catalysts, especially iron-sulfur centers. A number of selection mechanisms, including catalytic efficiency and specificity, hydrolytic stability, and selective solubilization, are proposed as key determinants for autocatalytic reproduction exploited in protometabolic evolution. This evolutionary process led from autocatalytic networks within preexisting compartments to discrete, reproducing, mobile vesicular protocells with the capacity to use soluble sugar phosphates and hence the opportunity to develop nucleic acids. Fidelity of information transfer in the reproduction of these increasingly complex autocatalytic networks is a key selection pressure in prebiological evolution that eventually leads to the selection of nucleic acids as a digital information subsystem and hence the emergence of fully functional chemotons capable of Darwinian evolution. 1 Introduction: Chemoton Subsystems and Evolutionary Pathways Living cells are autocatalytic entities that harness redox energy via the selective catalysis of biochemical transformations. -
Discovery, Metabolism and Functions of NAD and NADP
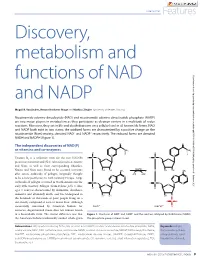
Coenzymes Features Discovery, metabolism and functions of NAD Downloaded from http://portlandpress.com/biochemist/article-pdf/37/1/9/3189/bio037010009.pdf by guest on 01 October 2021 and NADP Magali R. VanLinden, Renate Hvidsten Skoge and Mathias Ziegler (University of Bergen, Norway) Nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP) are two major players in metabolism as they participate as electron carriers in a multitude of redox reactions. Moreover, they act in life and death decisions on a cellular level in all known life forms. NAD and NADP both exist in two states; the oxidized forms are characterized by a positive charge on the nicotinamide (Nam) moiety, denoted NAD+ and NADP+ respectively. The reduced forms are denoted NADH and NADPH (Figure 1). The independent discoveries of NAD(P) as vitamins and co-enzymes Vitamin B3 is a collective term for the two NAD(P) precursors nicotinic acid (NA) (also referred to as niacin) and Nam, as well as their corresponding ribosides. Niacin and Nam were found to be essential nutrients after severe outbreaks of pellagra (originally thought to be a new pestilence) in 18th Century Europe. Large outbreaks of pellagra occurred in North America in the early 20th Century. Pellagra (from Italian: pelle = skin; agra = sour) is characterized by dermatitis, diarrhoea, dementia and ultimately death, and was widespread in the hundreds of thousands of poor people living on a diet mostly composed of corn or maize flour. Although successfully consumed by American Indians for centuries, degerminated maize does not contain niacin in a bioavailable form. The crucial difference was that Figure 1. -

Download Download
Dorjnamjaa et al. Mongolian Geoscientist 49 (2019) 41-49 https://doi.org/10.5564/mgs.v0i49.1226 Mongolian Geoscientist Review paper New scientific direction of the bacterial paleontology in Mongolia: an essence of investigation * Dorj Dorjnamjaa , Gundsambuu Altanshagai, Batkhuyag Enkhbaatar Department of Paleontology, Institute of Paleontology, Mongolian Academy of Sciences, Ulaanbaatar 15160, Mongolia *Corresponding author. Email: [email protected] ARTICLE INFO ABSTRACT Article history: We review the initial development of Bacterial Paleontology in Mongolia and Received 10 September 2019 present some electron microscopic images of fossil bacteria in different stages of Accepted 9 October 2019 preservation in sedimentary rocks. Indeed bacterial paleontology is one the youngest branches of paleontology. It has began in the end of 20th century and has developed rapidly in recent years. The main tasks of bacterial paleontology are detailed investigation of fossil microorganisms, in particular their morphology and sizes, conditions of burial and products of habitation that are reflected in lithological and geochemical features of rocks. Bacterial paleontology deals with fossil materials and is useful in analysis of the genesis of sedimentary rocks, and sedimentary mineral resources including oil and gas. The traditional paleontology is especially significant for evolution theory, biostratigraphy, biogeography and paleoecology; however bacterial paleontology is an essential first of all for sedimentology and for theories sedimentary ore genesis or biometallogeny Keywords: microfossils, phosphorite, sedimentary rocks, lagerstatten, biometallogeny INTRODUCTION all the microorganisms had lived and propagated Bacteria or microbes preserved well as fossils in without breakdowns. Bacterial paleontological various rocks, especially in sedimentary rocks data accompanied by the data on the first origin alike natural substances. -

Adenosine Triphosphate Turnover in Humans. Decreased Degradation During Relative Hyperphosphatemia
Adenosine triphosphate turnover in humans. Decreased degradation during relative hyperphosphatemia. M A Johnson, … , S P Schmaltz, I H Fox J Clin Invest. 1989;84(3):990-995. https://doi.org/10.1172/JCI114263. Research Article The regulation of ATP metabolism by inorganic phosphate (Pi) was examined in five normal volunteers through measurements of ATP degradation during relative Pi depletion and repletion states. Relative Pi depletion was achieved through dietary restriction and phosphate binders, whereas a Pi-repleted state was produced by oral Pi supplementation. ATP was radioactively labeled by the infusion of [8(14)C]adenine. Fructose infusion was used to produce rapid ATP degradation during Pi depletion and repletion states. Baseline measurements indicated a significant decrease of Pi levels during phosphate depletion and no change in serum or urinary purines. Serum values of Pi declined 20 to 26% within 15 min after fructose infusion in all states. Urine measurements of ATP degradation products showed an eightfold increase within 15 min after fructose infusion in both Pi-depleted and -supplemented states. Urinary radioactive ATP degradation products were fourfold higher and urinary purine specific activity was more than threefold higher during Pi depletion as compared with Pi repletion. Our data indicate that there is decreased ATP degradation to purine end products during a relative phosphate repletion state as compared to a relative phosphate depletion state. These data show that ATP metabolism can be altered through manipulation of the relative Pi state in humans. Find the latest version: https://jci.me/114263/pdf Adenosine Triphosphate Turnover in Humans Decreased Degradation during Relative Hyperphosphatemia Marcia A. -

The Road of Sustainable Development for Phosphate Fertilizer Industry in China
The Road of Sustainable Development for Phosphate Fertilizer Industry in China China Phosphate Industry Association Wu Xiyan 2013.9.Beijing Remarkable Achievements Phosphate fertilizer industry in China has kept rapidly developing since 2000; Ranked first in the world,it's production over US in 2005 ,achieved banlance between production and marketing in 2006,a surplus after 2007and became large exporter for Ammonium phosphate& coarse whiting ; The P fertilizer output reached 1693 t P2O5 in 2012, about 40 percent of the world; yr during 2000-2012 increased 8.1 percent; The growth in the first year of 2013 was slow, upto 8.372 million t from Jan.to June P2O5,Slightly increased 0.9%。 Product Structure of Phosphate fertilizer in China 2012, High concentration of phosphate &compound fertilizer took up 86% in 2012 from 35% in 2005 Total yield of 16.93 million t P2O5 in 2012 High concentration of phosphate &compound fertilizer took up 86.4% with 14.62 million t P2O5 ; AP output 12.60 million t P2O5 ,took up 74.4%; DAPphysical quantity14.6million t; MAP physical quantity 1328million t TSPphysical quantity1.07 million t; Phosphate group NPK physical quantity8.47million t Industrial Distribution of Phosphate fertilizer in China Two transfer basically realized:Basic fertilizer to Resources origin; Special fertilizer to end market Soil testing formula fertilization by Ministry of Agri.led enterprises produce accordingly output in Yunnan,Guizhou,Sichuan ,Hubei took up 71% overhall ; Hubei,Yunnan,Guizhou,C hongqing,Anhui ranked first -

China Fertilizer Industry Outlook
China Fertilizer Industry Outlook CONTENTS 1. Introduction 4 2. Chinese agriculture 6 3. Development of fertilizer demand 8 4. China’s fertilizer supply and international impact 9 5. Recent developments and outlook 12 6. Implications for GPCA members 14 1. Introduction China is the most important and most to support domestic crop production. It influential country in the fertilizer business. has now grown to such a scale that it is the Its development has been dramatic. In the largest producer, consumer and exporter mid-1990s, fertilizer demand was on the of urea and ammoniated phosphates in the scale of a medium sized country, albeit world, and one of the leading producers and growing at a rapid rate. Production was consumers of potash. relatively modest and the country was an importer of most fertilizer products. In this report we provide an overview of the Chinese fertilizer industry, tracking the development of For a period it ranked among the largest agriculture and demand, together with the supply side importers of urea. However, as the Chinese and its increasing international influence. We also economy has seen massive transformation, describe our expectations for its development in the so too has its agriculture sector, and the future and the impact it has on the GCC region and its fertilizer business whose target is primarily fertilizer producing companies. 4 | China - Fertilizer Industry Outlook China - Fertilizer Industry Outlook | 5 2. Chinese agriculture To understand the development of the growth in harvested area, therefore, has been the result Chinese fertilizer industry it is important to of increased multiple cropping. -

Origins of Life in the Universe Zackary Johnson
11/4/2007 Origins of Life in the Universe Zackary Johnson OCN201 Fall 2007 [email protected] Zackary Johnson http://www.soest.hawaii.edu/oceanography/zij/education.html Uniiiversity of Hawaii Department of Oceanography Class Schedule Nov‐2Originsof Life and the Universe Nov‐5 Classification of Life Nov‐7 Primary Production Nov‐9Consumers Nov‐14 Evolution: Processes (Steward) Nov‐16 Evolution: Adaptation() (Steward) Nov‐19 Marine Microbiology Nov‐21 Benthic Communities Nov‐26 Whale Falls (Smith) Nov‐28 The Marine Food Web Nov‐30 Community Ecology Dec‐3 Fisheries Dec‐5Global Ecology Dec‐12 Final Major Concepts TIMETABLE Big Bang! • Life started early, but not at the beginning, of Earth’s Milky Way (and other galaxies formed) history • Abiogenesis is the leading hypothesis to explain the beginning of life on Earth • There are many competing theories as to how this happened • Some of the details have been worked out, but most Formation of Earth have not • Abiogenesis almost certainly occurred in the ocean 20‐15 15‐94.5Today Billions of Years Before Present 1 11/4/2007 Building Blocks TIMETABLE Big Bang! • Universe is mostly hydrogen (H) and helium (He); for Milky Way (and other galaxies formed) example –the sun is 70% H, 28% He and 2% all else! Abundance) e • Most elements of interest to biology (C, N, P, O, etc.) were (Relativ 10 produced via nuclear fusion Formation of Earth Log at very high temperature reactions in large stars after Big Bang 20‐13 13‐94.7Today Atomic Number Billions of Years Before Present ORIGIN OF LIFE ON EARTH Abiogenesis: 3 stages Divine Creation 1. -

ATP Structure and Function
ATP: Universal Currency of Cellular Energy All living things including plants, animals, birds, insects, humans need energy for the proper functioning of cells, tissues and other organ systems. As we are aware that green plants, obtain their energy from the sunlight, and animals get their energy by feeding on these plants. Energy acts as a source of fuel. We, humans, gain energy from the food we eat, but how are the energy produced and stored in our body. A living cell cannot store significant amounts of free energy. Excess free energy would result in an increase of heat in the cell, which would result in excessive thermal motion that could damage and then destroy the cell. Rather, a cell must be able to handle that energy in a way that enables the cell to store energy safely and release it for use only as needed. Living cells accomplish this by using the compound adenosine triphosphate (ATP). ATP is often called the “energy currency” of the cell, and, like currency, this versatile compound can be used to fill any energy need of the cell. How? It functions similarly to a rechargeable battery. When ATP is broken down, usually by the removal of its terminal phosphate group, energy is released. The energy is used to do work by the cell, usually by the released phosphate binding to another molecule, activating it. For example, in the mechanical work of muscle contraction, ATP supplies the energy to move the contractile muscle proteins. Recall the active transport work of the sodium-potassium pump in cell membranes. -

Aluminum Phosphate
Right to Know Hazardous Substance Fact Sheet Common Name: ALUMINUM PHOSPHATE Synonyms: Aluminum Monophosphate CAS Number: 7784-30-7 Chemical Name: Phosphoric Acid, Aluminum Salt (1:1) RTK Substance Number: 0062 Date: June 1998 Revision: July 2007 DOT Number: UN 1760 Description and Use EMERGENCY RESPONDERS >>>> SEE BACK PAGE Aluminum Phosphate is an odorless, white crystalline solid Hazard Summary which is often used in liquid or gel form. It is used in ceramics, Hazard Rating NJDOH NFPA dental cements, cosmetics, paints, paper and pharmaceuticals. HEALTH 2 - FLAMMABILITY 0 - REACTIVITY 0 - CORROSIVE POISONOUS GASES ARE PRODUCED IN FIRE CONTAINERS MAY EXPLODE IN FIRE DOES NOT BURN Reason for Citation Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; f Aluminum Phosphate is on the Right to Know Hazardous 4=severe Substance List because it is cited by OSHA, ACGIH, DOT f Aluminum Phosphate can affect you when inhaled. and NIOSH. f Contact can irritate and burn the skin and eyes. f This chemical is on the Special Health Hazard Substance f Inhaling Aluminum Phosphate can irritate the nose, throat List. and lungs. SEE GLOSSARY ON PAGE 5. FIRST AID Eye Contact Workplace Exposure Limits f Immediately flush with large amounts of cool water. The following exposure limits are for inorganic Aluminum Continue for at least 15 minutes, occasionally lifting upper compounds (measured as Aluminum): and lower lids. Remove contact lenses, if worn, while rinsing. Immediate medical attention is necessary. OSHA: The legal airborne permissible exposure limit (PEL) is 15 mg/m3 (as total dust), and 5 mg/m3 (as respirable Skin Contact dust) averaged over an 8-hour workshift. -

Phosphorus in the Kidney Disease Diet: Become a Phosphorus Detective
Phosphorus in the Kidney Disease Diet: Become a Phosphorus Detective Carolyn Feibig, MS, RD, LD Transplant Dietitian The George Washington University Hospital Thanks to our speaker! Carolyn Feibig, MS, RD, LD • Kidney Transplant Dietitian at the George Washington University Hospital • Passionate about educating the general public about the importance of early detection of kidney disease and the importance of a healthy diet for kidney health Objectives Managing your phosphorus can be overwhelming! Today we will look at: – what is phosphorus, why it is important – how you can manage your phosphorus with kidney disease/ on dialysis – what can happen if your phosphorus is out of range (high or low) After today you will be a Master Phosphorus Detective – with the skills to find all sources of phosphorus and how to keep your phos in range. Phosphorus • Phosphorus is vital to the production and storage of energy in the human body. It is a main component in ATP (Adenosine Triphosphate). It is widely available in food, and is a important to bone building and health. • About 85% to 90% of total body phosphorus is found in bones and teeth. • Phosphorus is also a component of fats, proteins, and cell membranes. Phosphorus • High levels of phosphorus in your blood are not IMMEDIATELY harmful but can cause SEVERE long term problems. • The recommended range for dialysis patients is 3.0 to 5.5 mg/dL. • The following slides discuss what happens when your phosphorus is high BUT low phos can be cause for immediate concern: – Although rare, a severe drop in serum phosphorus 1.5 mg/dL or below, can cause neuromuscular disturbances, coma and death due to impaired cellular metabolism. -

New RNA Research Demonstrates Prebiotic Possibility
Cleveland State University EngagedScholarship@CSU Chemistry Faculty Publications Chemistry Department 1-2020 New RNA Research Demonstrates Prebiotic Possibility David W. Ball Cleveland State University, [email protected] Follow this and additional works at: https://engagedscholarship.csuohio.edu/scichem_facpub Part of the Chemistry Commons How does access to this work benefit ou?y Let us know! Publisher's Statement Link to publisher version: https://skepticalinquirer.org/2020/01/new-rna-research-demonstrates- prebiotic-possibility/ Recommended Citation Ball, David W., "New RNA Research Demonstrates Prebiotic Possibility" (2020). Chemistry Faculty Publications. 522. https://engagedscholarship.csuohio.edu/scichem_facpub/522 This Article is brought to you for free and open access by the Chemistry Department at EngagedScholarship@CSU. It has been accepted for inclusion in Chemistry Faculty Publications by an authorized administrator of EngagedScholarship@CSU. For more information, please contact [email protected]. New RNA Research Demonstrates Prebiotic Possibility David W. Ball Creationists and other religious fundamentalists commonly (and erroneously) bring up the issue of abiogenesis as an argument against evolution, claiming that life is too complex to have arisen naturally from simple (non-living) chemicals. Abiogenesis is the development of chemical life from non-living chemicals, and is an active area of research for scientists studying the “Origin Of Life” question. The issue is largely irrelevant as an argument against evolution because evolution deals with what happens after life is formed. It is widely accepted that modern abiogenesis research traces back to the Miller-Urey experiment, performed by Stanley Miller at the University of Chicago (with assistance from Harold Urey) and published in 1953.