Phosphorus in the Kidney Disease Diet: Become a Phosphorus Detective
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nutrients: Nitrogen (N), Sulfur (S), Phosphorus (P), Potassium (K)
Nutrients: Nitrogen (N), Sulfur (S), Phosphorus (P), Potassium (K) Essential for all life, their availability (or lack thereof) controls the distribution of flora and fauna Look into their: Sources Pools (sinks) Fluxes root uptake + microbial uptake leaching solid solution Nutrients must be in a specific form – specie - for use by organisms Nutrient Cycling: N, S, P, K Soil Organic Matter (CHONPS) Minerals Primary Productivity (P, S, K) O Leaves & Roots A Decomposition Heterotrophic respiration B Gas loss SOM/Minerals Microbes leaching of nutrients plant nutrient uptake Nutrients: natural & anthropogenic sources (IN) and outputs (OUT) N2 fertilizers (chemical, manure, sludge) gases and particulates to atmosphere pesticides (fossil fuel combustion (coal/oil); cycles; trees) wet and dry deposition (acid rain, aerosols) harvesting plant tissue/residues root uptake IN OUT SOIL Pools (sinks) (SOM/clays/oxides) Fluxes (transformations) OUT IN ions and molecules in solution (leaching) roots (exudates, biomass) colloidal transport bedrock (1ry/2ry minerals in parent material) erosion runoff The Nitrogen Cycle + The Nitrogen Cycle Denitrification: - - NO3 is the most stable N2 (g) is prevalent in reduction of NO3 chemical form of N in the air of soil pores to reduced forms aerated soil solutions of N (N2) (energy- consuming) Atmospheric N deposition Nitrogen evolution (gases) Fertilizer additions 700 (+5) +5 Oxic - denitrification NO3 (+3) zone - NO2 (+2) (mV) NO (+1) h E N2O Suboxic (0) nitrification N state oxidation N2 236 zone immobilization -

Use of Phosphate Solubilizing Bacteria to Leach Rare Earth Elements from Monazite-Bearing Ore
Minerals 2015, 5, 189-202; doi:10.3390/min5020189 OPEN ACCESS minerals ISSN 2075-163X www.mdpi.com/journal/minerals Article Use of Phosphate Solubilizing Bacteria to Leach Rare Earth Elements from Monazite-Bearing Ore Doyun Shin 1,2,*, Jiwoong Kim 1, Byung-su Kim 1,2, Jinki Jeong 1,2 and Jae-chun Lee 1,2 1 Mineral Resources Resource Division, Korea Institute of Geoscience and Mineral Resources (KIGAM), Gwahangno 124, Yuseong-gu, Daejeon 305-350, Korea; E-Mails: [email protected] (J.K.); [email protected] (B.K.); [email protected] (J.J.); [email protected] (J.L.) 2 Department of Resource Recycling Engineering, Korea University of Science and Technology, Gajeongno 217, Yuseong-gu, Daejeon 305-350, Korea * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +82-42-868-3616. Academic Editor: Anna H. Kaksonen Received: 8 January 2015 / Accepted: 27 March 2015 / Published: 2 April 2015 Abstract: In the present study, the feasibility to use phosphate solubilizing bacteria (PSB) to develop a biological leaching process of rare earth elements (REE) from monazite-bearing ore was determined. To predict the REE leaching capacity of bacteria, the phosphate solubilizing abilities of 10 species of PSB were determined by halo zone formation on Reyes minimal agar media supplemented with bromo cresol green together with a phosphate solubilization test in Reyes minimal liquid media as the screening studies. Calcium phosphate was used as a model mineral phosphate. Among the test PSB strains, Pseudomonas fluorescens, P. putida, P. rhizosphaerae, Mesorhizobium ciceri, Bacillus megaterium, and Acetobacter aceti formed halo zones, with the zone of A. -

Prebiological Evolution and the Metabolic Origins of Life
Prebiological Evolution and the Andrew J. Pratt* Metabolic Origins of Life University of Canterbury Keywords Abiogenesis, origin of life, metabolism, hydrothermal, iron Abstract The chemoton model of cells posits three subsystems: metabolism, compartmentalization, and information. A specific model for the prebiological evolution of a reproducing system with rudimentary versions of these three interdependent subsystems is presented. This is based on the initial emergence and reproduction of autocatalytic networks in hydrothermal microcompartments containing iron sulfide. The driving force for life was catalysis of the dissipation of the intrinsic redox gradient of the planet. The codependence of life on iron and phosphate provides chemical constraints on the ordering of prebiological evolution. The initial protometabolism was based on positive feedback loops associated with in situ carbon fixation in which the initial protometabolites modified the catalytic capacity and mobility of metal-based catalysts, especially iron-sulfur centers. A number of selection mechanisms, including catalytic efficiency and specificity, hydrolytic stability, and selective solubilization, are proposed as key determinants for autocatalytic reproduction exploited in protometabolic evolution. This evolutionary process led from autocatalytic networks within preexisting compartments to discrete, reproducing, mobile vesicular protocells with the capacity to use soluble sugar phosphates and hence the opportunity to develop nucleic acids. Fidelity of information transfer in the reproduction of these increasingly complex autocatalytic networks is a key selection pressure in prebiological evolution that eventually leads to the selection of nucleic acids as a digital information subsystem and hence the emergence of fully functional chemotons capable of Darwinian evolution. 1 Introduction: Chemoton Subsystems and Evolutionary Pathways Living cells are autocatalytic entities that harness redox energy via the selective catalysis of biochemical transformations. -
Discovery, Metabolism and Functions of NAD and NADP
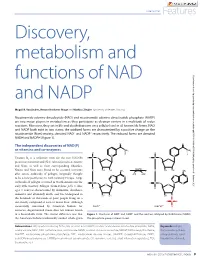
Coenzymes Features Discovery, metabolism and functions of NAD Downloaded from http://portlandpress.com/biochemist/article-pdf/37/1/9/3189/bio037010009.pdf by guest on 01 October 2021 and NADP Magali R. VanLinden, Renate Hvidsten Skoge and Mathias Ziegler (University of Bergen, Norway) Nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP) are two major players in metabolism as they participate as electron carriers in a multitude of redox reactions. Moreover, they act in life and death decisions on a cellular level in all known life forms. NAD and NADP both exist in two states; the oxidized forms are characterized by a positive charge on the nicotinamide (Nam) moiety, denoted NAD+ and NADP+ respectively. The reduced forms are denoted NADH and NADPH (Figure 1). The independent discoveries of NAD(P) as vitamins and co-enzymes Vitamin B3 is a collective term for the two NAD(P) precursors nicotinic acid (NA) (also referred to as niacin) and Nam, as well as their corresponding ribosides. Niacin and Nam were found to be essential nutrients after severe outbreaks of pellagra (originally thought to be a new pestilence) in 18th Century Europe. Large outbreaks of pellagra occurred in North America in the early 20th Century. Pellagra (from Italian: pelle = skin; agra = sour) is characterized by dermatitis, diarrhoea, dementia and ultimately death, and was widespread in the hundreds of thousands of poor people living on a diet mostly composed of corn or maize flour. Although successfully consumed by American Indians for centuries, degerminated maize does not contain niacin in a bioavailable form. The crucial difference was that Figure 1. -

Download Download
Dorjnamjaa et al. Mongolian Geoscientist 49 (2019) 41-49 https://doi.org/10.5564/mgs.v0i49.1226 Mongolian Geoscientist Review paper New scientific direction of the bacterial paleontology in Mongolia: an essence of investigation * Dorj Dorjnamjaa , Gundsambuu Altanshagai, Batkhuyag Enkhbaatar Department of Paleontology, Institute of Paleontology, Mongolian Academy of Sciences, Ulaanbaatar 15160, Mongolia *Corresponding author. Email: [email protected] ARTICLE INFO ABSTRACT Article history: We review the initial development of Bacterial Paleontology in Mongolia and Received 10 September 2019 present some electron microscopic images of fossil bacteria in different stages of Accepted 9 October 2019 preservation in sedimentary rocks. Indeed bacterial paleontology is one the youngest branches of paleontology. It has began in the end of 20th century and has developed rapidly in recent years. The main tasks of bacterial paleontology are detailed investigation of fossil microorganisms, in particular their morphology and sizes, conditions of burial and products of habitation that are reflected in lithological and geochemical features of rocks. Bacterial paleontology deals with fossil materials and is useful in analysis of the genesis of sedimentary rocks, and sedimentary mineral resources including oil and gas. The traditional paleontology is especially significant for evolution theory, biostratigraphy, biogeography and paleoecology; however bacterial paleontology is an essential first of all for sedimentology and for theories sedimentary ore genesis or biometallogeny Keywords: microfossils, phosphorite, sedimentary rocks, lagerstatten, biometallogeny INTRODUCTION all the microorganisms had lived and propagated Bacteria or microbes preserved well as fossils in without breakdowns. Bacterial paleontological various rocks, especially in sedimentary rocks data accompanied by the data on the first origin alike natural substances. -

Phosphorus Metabolism
rology & h T ep h e N r f a o p l e a u n t r i c Raina et al., J Nephrol Therapeutic 2012, S3 u s o J Journal of Nephrology & Therapeutics DOI: 10.4172/2161-0959.S3-008 ISSN: 2161-0959 Review Article Open Access Phosphorus Metabolism Rupesh Raina1*, Gaurav Garg2, Sidharth Kumar Sethi4, Martin J Schreiber3, James F Simon3 and George Thomas3 1Fellow at Rainbow Babies and Children Hospital, Case Western Reserve, Cleveland, OH, USA 2Observer at Cleveland Clinic, Department of Hospital Medicine, Cleveland, OH, USA 3Staff at Glickman Urology and Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH, USA 4Kidney and Urology Institute, Medanta, The Medicity Hospital, Gurgaon, Haryana, India Abstract Phosphorus plays a pivotal role in various biological processes. Therefore, a deeper understanding of Phosphorus Homeostasis is essential for management and treatment of conditions causing an imbalance in phosphate metabolism. The widely understood parathyroid hormone (PTH) and vitamin D axis that governs this phosphate homeostasis has been critiqued for its inability to explain a few rare genetic and acquired conditions associated with phosphate imbalance. Such conditions are characterized by normal PTH and activated vitamin D hormone. For example, Tumor Induced osteomalacia, Autosomal Dominant hypophosphatemic rickets, and X-linked hypophosphatemic rickets. Recent studies of such conditions have led to the discovery of additional factors that play an important role in phosphorus homeostasis. These phosphaturetic factors, called “Phosphatonins” include Fibroblast Growth Factor 23 (FGF-23), Fibroblast Growth Factor 7 (FGF7), Frizzled related protein 4 (FRP4), and matrix extracellular phosphoglycoprotein (MEPE).Out of these phosphatonins, FGF-23 has been extensively studied. -

Phosphorus and Sulfur Cosmochemistry: Implications for the Origins of Life
Phosphorus and Sulfur Cosmochemistry: Implications for the Origins of Life Item Type text; Electronic Dissertation Authors Pasek, Matthew Adam Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 07/10/2021 06:16:37 Link to Item http://hdl.handle.net/10150/194288 PHOSPHORUS AND SULFUR COSMOCHEMISTRY: IMPLICATIONS FOR THE ORIGINS OF LIFE by Matthew Adam Pasek ________________________ A Dissertation Submitted to the Faculty of the DEPARTMENT OF PLANETARY SCIENCE In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY In the Graduate College UNIVERSITY OF ARIZONA 2 0 0 6 2 THE UNIVERSITY OF ARIZONA GRADUATE COLLEGE As members of the Dissertation Committee, we certify that we have read the dissertation prepared by Matthew Adam Pasek entitled Phosphorus and Sulfur Cosmochemistry: Implications for the Origins of Life and recommend that it be accepted as fulfilling the dissertation requirement for the Degree of Doctor of Philosophy _______________________________________________________________________ Date: 04/11/2006 Dante Lauretta _______________________________________________________________________ Date: 04/11/2006 Timothy Swindle _______________________________________________________________________ Date: 04/11/2006 -

Adenosine Triphosphate Turnover in Humans. Decreased Degradation During Relative Hyperphosphatemia
Adenosine triphosphate turnover in humans. Decreased degradation during relative hyperphosphatemia. M A Johnson, … , S P Schmaltz, I H Fox J Clin Invest. 1989;84(3):990-995. https://doi.org/10.1172/JCI114263. Research Article The regulation of ATP metabolism by inorganic phosphate (Pi) was examined in five normal volunteers through measurements of ATP degradation during relative Pi depletion and repletion states. Relative Pi depletion was achieved through dietary restriction and phosphate binders, whereas a Pi-repleted state was produced by oral Pi supplementation. ATP was radioactively labeled by the infusion of [8(14)C]adenine. Fructose infusion was used to produce rapid ATP degradation during Pi depletion and repletion states. Baseline measurements indicated a significant decrease of Pi levels during phosphate depletion and no change in serum or urinary purines. Serum values of Pi declined 20 to 26% within 15 min after fructose infusion in all states. Urine measurements of ATP degradation products showed an eightfold increase within 15 min after fructose infusion in both Pi-depleted and -supplemented states. Urinary radioactive ATP degradation products were fourfold higher and urinary purine specific activity was more than threefold higher during Pi depletion as compared with Pi repletion. Our data indicate that there is decreased ATP degradation to purine end products during a relative phosphate repletion state as compared to a relative phosphate depletion state. These data show that ATP metabolism can be altered through manipulation of the relative Pi state in humans. Find the latest version: https://jci.me/114263/pdf Adenosine Triphosphate Turnover in Humans Decreased Degradation during Relative Hyperphosphatemia Marcia A. -

The Road of Sustainable Development for Phosphate Fertilizer Industry in China
The Road of Sustainable Development for Phosphate Fertilizer Industry in China China Phosphate Industry Association Wu Xiyan 2013.9.Beijing Remarkable Achievements Phosphate fertilizer industry in China has kept rapidly developing since 2000; Ranked first in the world,it's production over US in 2005 ,achieved banlance between production and marketing in 2006,a surplus after 2007and became large exporter for Ammonium phosphate& coarse whiting ; The P fertilizer output reached 1693 t P2O5 in 2012, about 40 percent of the world; yr during 2000-2012 increased 8.1 percent; The growth in the first year of 2013 was slow, upto 8.372 million t from Jan.to June P2O5,Slightly increased 0.9%。 Product Structure of Phosphate fertilizer in China 2012, High concentration of phosphate &compound fertilizer took up 86% in 2012 from 35% in 2005 Total yield of 16.93 million t P2O5 in 2012 High concentration of phosphate &compound fertilizer took up 86.4% with 14.62 million t P2O5 ; AP output 12.60 million t P2O5 ,took up 74.4%; DAPphysical quantity14.6million t; MAP physical quantity 1328million t TSPphysical quantity1.07 million t; Phosphate group NPK physical quantity8.47million t Industrial Distribution of Phosphate fertilizer in China Two transfer basically realized:Basic fertilizer to Resources origin; Special fertilizer to end market Soil testing formula fertilization by Ministry of Agri.led enterprises produce accordingly output in Yunnan,Guizhou,Sichuan ,Hubei took up 71% overhall ; Hubei,Yunnan,Guizhou,C hongqing,Anhui ranked first -

China Fertilizer Industry Outlook
China Fertilizer Industry Outlook CONTENTS 1. Introduction 4 2. Chinese agriculture 6 3. Development of fertilizer demand 8 4. China’s fertilizer supply and international impact 9 5. Recent developments and outlook 12 6. Implications for GPCA members 14 1. Introduction China is the most important and most to support domestic crop production. It influential country in the fertilizer business. has now grown to such a scale that it is the Its development has been dramatic. In the largest producer, consumer and exporter mid-1990s, fertilizer demand was on the of urea and ammoniated phosphates in the scale of a medium sized country, albeit world, and one of the leading producers and growing at a rapid rate. Production was consumers of potash. relatively modest and the country was an importer of most fertilizer products. In this report we provide an overview of the Chinese fertilizer industry, tracking the development of For a period it ranked among the largest agriculture and demand, together with the supply side importers of urea. However, as the Chinese and its increasing international influence. We also economy has seen massive transformation, describe our expectations for its development in the so too has its agriculture sector, and the future and the impact it has on the GCC region and its fertilizer business whose target is primarily fertilizer producing companies. 4 | China - Fertilizer Industry Outlook China - Fertilizer Industry Outlook | 5 2. Chinese agriculture To understand the development of the growth in harvested area, therefore, has been the result Chinese fertilizer industry it is important to of increased multiple cropping. -

Origins of Life in the Universe Zackary Johnson
11/4/2007 Origins of Life in the Universe Zackary Johnson OCN201 Fall 2007 [email protected] Zackary Johnson http://www.soest.hawaii.edu/oceanography/zij/education.html Uniiiversity of Hawaii Department of Oceanography Class Schedule Nov‐2Originsof Life and the Universe Nov‐5 Classification of Life Nov‐7 Primary Production Nov‐9Consumers Nov‐14 Evolution: Processes (Steward) Nov‐16 Evolution: Adaptation() (Steward) Nov‐19 Marine Microbiology Nov‐21 Benthic Communities Nov‐26 Whale Falls (Smith) Nov‐28 The Marine Food Web Nov‐30 Community Ecology Dec‐3 Fisheries Dec‐5Global Ecology Dec‐12 Final Major Concepts TIMETABLE Big Bang! • Life started early, but not at the beginning, of Earth’s Milky Way (and other galaxies formed) history • Abiogenesis is the leading hypothesis to explain the beginning of life on Earth • There are many competing theories as to how this happened • Some of the details have been worked out, but most Formation of Earth have not • Abiogenesis almost certainly occurred in the ocean 20‐15 15‐94.5Today Billions of Years Before Present 1 11/4/2007 Building Blocks TIMETABLE Big Bang! • Universe is mostly hydrogen (H) and helium (He); for Milky Way (and other galaxies formed) example –the sun is 70% H, 28% He and 2% all else! Abundance) e • Most elements of interest to biology (C, N, P, O, etc.) were (Relativ 10 produced via nuclear fusion Formation of Earth Log at very high temperature reactions in large stars after Big Bang 20‐13 13‐94.7Today Atomic Number Billions of Years Before Present ORIGIN OF LIFE ON EARTH Abiogenesis: 3 stages Divine Creation 1. -

Phosphorus: from the Stars to Land &
Phosphorus: From the Stars to Land & Sea The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Cummins, Christopher C. “Phosphorus: From the Stars to Land & Sea.” Daedalus 143, no. 4 (October 2014): 9–20. As Published http://dx.doi.org/10.1162/DAED_a_00301 Publisher MIT Press Version Final published version Citable link http://hdl.handle.net/1721.1/92509 Terms of Use Article is made available in accordance with the publisher's policy and may be subject to US copyright law. Please refer to the publisher's site for terms of use. Phosphorus: From the Stars to Land & Sea Christopher C. Cummins Abstract: The chemistry of the element phosphorus offers a window into the diverse ½eld of inorganic chemistry. Fundamental investigations into some simple molecules containing phosphorus reveal much about the rami½cations of this element’s position in the periodic table and that of its neighbors. Addition - ally, there are many phosphorus compounds of commercial importance, and the industry surrounding this element resides at a crucial nexus of natural resource stewardship, technology, and modern agriculture. Questions about our sources of phosphorus and the applications for which we deploy it raise the provocative issue of the human role in the ongoing depletion of phosphorus deposits, as well as the transfer of phos- phorus from the land into the seas. Inorganic chemistry can be de½ned as “the chem- istry of all the elements of the periodic table,”1 but as such, the ½eld is impossibly broad, encompassing everything from organic chemistry to materials sci- ence and enzymology.