Defences: the Integumentary System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CHAPTER 4 the Integumentary System
CHAPTER 4 The Integumentary System LEARNING OBJECTIVES Upon completion of this chapter, you should be able to: • Name the two layers of the skin. • Name the accessory structures of the integumentary system. • Build and pronounce medical terms of the integumentary system. • Name the disorders and treatments relating to the integumentary system. • Name the major classifi cations of pharmacologic agents used to treat skin disorders. • Analyze and defi ne the new terms introduced in this chapter. • Interpret abbreviations associated with the integumentary system. 53 54 PART TWO • BODY SYSTEMS Introduction The largest organ of the body is the skin. The skin covers the entire body—more than 20 square feet on average—and weighs about 24 pounds. It is part of the integumentary system, which also includes the accessory structures: hair, nails, and sebaceous (oil) and sudoriferous (sweat) glands. Integumentum is Latin for “covering” or “shelter.” The physician who specializes in the diag- nosis and treatment of skin disorders is called a dermatologist (dermat/o being one of the com- bining forms for skin). Coupling the root dermat/o with the previously learned suffi x -logy gives us the term dermatology , which is the term for the specialty practice that deals with the skin. Word Elements The major word elements that relate to the integumentary system consist of various anatomical components, accessory structures, colors of the skin, and abnormal conditions. The Word Ele- ments table lists many of the roots, their meanings, and examples associated -

Ch7 Basic Body Structure and Function Test&A
Chapter 7- Test Name: Basic Body Structure & Fuction Date: 1. Physiology is the study of A) what body parts look like and where they are located. B) the structure and function of the human body. C) how the various body parts work. D) how organisms are created. 2. The basic unit of life is A) a cell. B) a tissue. C) an organ. D) an organ system. 3. Which one of the following is like the cell's brain? A) The cytoplasm B) The cell nucleus C) The cell organelles D) The cell membrane 4. Which cell transports oxygen throughout the body? A) Red blood B) Epithelial C) Muscle D) Nerve 5. Which one of the following is considered connective tissue? A) Mucous membrane B) Blood C) Skin D) Glands 6. Which one of the following organs is included in the integumentary system? A) The fingernails B) The gallbladder C) The pancreas D) The ureters 7. What does epithelial tissue do? A) It connects tissues together. B) It produces movement. C) It conducts information. D) It protects the body. Page 1 8. Which statement correctly describes homeostasis? A) It causes problems by invading otherwise healthy tissues. B) It reduces the immune system's ability to fight off infection. C) It is a state of balance achieved by all of the organ systems working together. D) It occurs when the structure or function of an organ or organ system is abnormal. 9. The purpose of melanin is to A) keep the skin lubricated. B) aid in temperature regulation. C) give our skin, hair, and eyes color. -
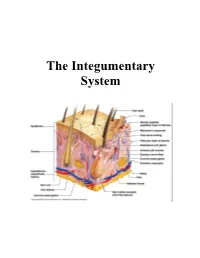
The Integumentary System
The Integumentary System THE INTEGUMENTARY SYSTEM Skin is the system of the body that makes an individual beautiful! Skin/fur coloration allows animals to be camouflaged. *The skin is the largest organ of the body. The skin and its derivatives (hair, nails, sweat and oil glands) make up the integumentary system. The total surface area of the skin is about 1.8 m² and its total weight is about 11 kg. The skin gives us our appearance and shape. Anatomy of the Skin • Skin is made up of two layers that cover a third fatty layer. The outer layer is called the epidermis; it is a tough protective layer. The second layer (located under the epidermis) is called the dermis; it contains nerve endings, sweat glands, oil glands, and hair follicles. Under these two skin layers is a fatty layer called the subcutaneous tissue, or hypodermis. 1 • The dermis is home to the oil glands. These are also called sebaceous glands, and they are always producing sebum. Sebum is your skin's own natural oil. It rises to the surface of your epidermis to keep your skin lubricated and protected. It also makes your skin waterproof. • Skin is alive! It's made of many thin sheets of flat, stacked cells. Older cells are constantly being pushed to the surface by new cells, which grow from below. When the old ones reach the top, they become wider and flatter as they get rubbed and worn by all your activity. And, sooner or later, they end up popping off like tiles blown from a roof in a strong wind. -
The Integumentary System (In Teg Yoo MEN Tuh Ree) Skin, Tissues, and You � the Integumentary System Is the Body’S Outer Covering
The Integumentary System (In teg yoo MEN tuh ree) Skin, Tissues, and You ! " The Integumentary system is the body’s outer covering. It has the task of physically separating the body from the external environment. This is the first key to homeostasis. ! " Homeostasis: The internal stability or “steady state” maintained by your body. We maintain a body temperature of 98.6ºF (37ºC) ! " The Integumentary system isn’t perfect. Cuts and other injuries break the barrier of the system and allow microorganisms to enter the body. Also, extensive exposure to the sun can cause damage to the tissue. Other harmful agents can damage the system as well. http://academic.kellogg.edu/herbrandsonc/bio201_mckinley/f5-1_layers_of_the_inte_c.jpg The Skin and Tissue Tissues ! " Your body contains 250 different types of cells. ! " Groups of similar cells with common function are called tissues. ! " Tissues protect the body, connect body parts together, some lift and move the body, some transmit http://asweknowit.net/images_edu/dwa5%20tissues.jpg information. Epithelial Tissue ! " Epithelial tissue: sheets of closely packed cells that cover the entire surface of your body and form the lining of your internal organs, many different types all serve the general function of protecting the tissues and organs they cover ! " In your respiratory system, ! " 1st type; line your windpipe and its major branches, cells secrete mucus which traps dust, pollen. etc. cilia sweep them up to throat to be swallowed, ! " 2nd type; lines narrower airways cells have smooth surface allows -

Body Systems Work Together by Cindy Grigg
Body Systems Work Together By Cindy Grigg 1 You know that your body is made of cells. When groups of cells do the same kind of work, they are called tissues. The word tissue comes from a Latin word meaning to "weave." Cells that make up tissues are sometimes "woven" together. 2 You have four main types of tissues: epithelial, nervous, muscle, and connective tissue. Epithelial tissue covers the outside of the body. It also lines organs and cavities. Nervous tissue sends electrical signals. Muscle tissue helps you move. Connective tissue joins bones and cushions organs. 3 When groups of tissues work together, they are called organs. Some examples of organs are the heart, lungs, skin, and stomach. When organs work together, they are called systems. For example, your heart, lungs, blood, and blood vessels work together. They make up the circulatory system. 4 There are eleven systems in the human body: muscular system, respiratory system, digestive system, integumentary system (skin), skeletal system, circulatory (or cardiovascular) system, excretory (or urinary) system, reproductive system, nervous system, lymphatic system, and endocrine system. Each system has a special job. 5 All of your body systems have to work together to keep you healthy. Your bones and muscles work together to support and move your body. Your respiratory system takes in oxygen from the air. It also gets rid of carbon dioxide. 6 Your digestive system absorbs water and nutrients from the food you eat. 7 Your circulatory system carries oxygen, water, and nutrients to cells throughout your body. Wastes from the cells are eliminated by your respiratory system, your excretory system, and your skin. -

Medical Literacy Bridge
Written by Jack McGrath Layout and computer assistance by Kathy Yeomans Edited by Jack McGrath and Kathy Yeomans DVD by Terry Weiser, VACE Technology Development Center Supervision by Steve Thompson Special thanks to the Workforce Investment Board of Ventura County Printed by Ventura Unified School District The Workforce Investment Board of Ventura County sponsored the creation of this curriculum based on a contract awarded to Ventura Adult and Continuing Education. The curriculum is the result of VACE’s observations regarding student success rate for English Language Learners and basic literacy English speakers who enroll in Allied Health training programs. Introduction: Medical Literacy Bridge ............................................................................................................................. 1 A Bridge to Medical Terminology ...................................................................................................................................................... 2 DVD instructions ....................................................................................................................................................................................... 2 Memory Techniques ................................................................................................................................................................................ 2 English Word Study and Medical Text Books .............................................................................................................................. -

Human Body Systems
INTEREST GRABBER – NOTEBOOK #1 AN IMPORTANT PROCESS While walking along a dusty path, you begin to cough. As you continue your walk, a small insect comes flying toward you. You blink and then duck so that it misses you. These actions are just a few examples of homeostasis. Homeostasis is the process by which organisms keep internal conditions relatively constant despite changes in their external environments. 1. List three other examples of homeostasis that occur in organisms. 2. Why is homeostasis important to an organism? INTEREST GRABBER 1. List three other examples of homeostasis that occur in organisms. Accept all reasonable student examples that show an understanding of homeostasis. 2. Why is homeostasis important to an organism? Homeostasis allows an organism to remain in balance with its environment. If homeostasis is not maintained, it can harm the organism or result in the death of the organism. LEVELS OF ORGANIZATION IN A MULTICELLULAR ORGANISM Cell Tissue Organ Organ system Complete organism NERVOUS SYSTEM - controls and coordinates functions throughout the body and responds to internal and external stimuli Nervous System Integumentary System Skeletal System Muscular System Circulatory System NERVOUS SYSTEM Structures: Brain, spinal cord, peripheral nerves Function: Recognizes and coordinates the body’s response to changes in the internal and external environments NERVOUS SYSTEM - THE SYNAPSE Direction of Impulse Dendrite of -chemical messages adjacent neuron Axon Receptor (neurotransmitters) Vesicle are sent to the Axon synapse -
The Integumentary System the Integumentary System
Essentials of Anatomy & Physiology, 4th Edition Martini / Bartholomew The Integumentary System PowerPoint® Lecture Outlines prepared by Alan Magid, Duke University Slides 1 to 51 Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Integumentary System Components • Cutaneous membrane • Epidermis • Dermis • Accessory structures • Subcutaneous layer (hypodermis) Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Main Functions of the Integument • Protection • Temperature maintenance • Synthesis and storage of nutrients • Sensory reception • Excretion and secretion Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Components of the Integumentary System Figure 5-1 Integumentary Structure/Function The Epidermis • Stratified squamous epithelium • Several distinct cell layers • Thick skin—five layers • On palms and soles • Thin skin—four layers • On rest of body Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Cell Layers of The Epidermis • Stratum germinativum • Stratum spinosum • Stratum granulosum • Stratum lucidum (in thick skin) • Stratum corneum • Dying superficial layer • Keratin accumulation Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function The Structure of the Epidermis Figure 5-2 Integumentary Structure/Function Cell Layers of The Epidermis • Stratum germinativum -
Tissues and Integumentary System Biol 105 Chapter 4
Into to A&P: Tissues and Integumentary System Biol 105 Chapter 4 Outline I. Tissues A. Epithelial B. Connective C. Muscle D. Nervous tissues II. Cell to Cell Contact III. Body Cavities IV. Membranes V. Homeostasis VI. Integumentary System (includes: skin, hair, nails) Copyright © 2009 Pearson Education, Inc. Copyright © 2009 Pearson Education, Inc. Organization of the Human Body § Multicellular organisms require specialized cells to perform specific tasks. § These cells then organize into tissues, tissues organize into organs and organs organize into organ systems. Copyright © 2009 Pearson Education, Inc. Tissues § A tissue is a group of cells that work together to accomplish a common function. Copyright © 2009 Pearson Education, Inc. Tissues § There are four primary tissue types: 1. Epithelial tissue 2. Connective tissue 3. Muscle tissue 4. Nervous tissue Copyright © 2009 Pearson Education, Inc. Tissues - Epithelial § Epithelial Tissue covers the body surfaces, lines cavities and organs, and forms glands. Copyright © 2009 Pearson Education, Inc. Tissues - Connective § Connective Tissue binds and supports the body, provides protection for our organs, serves as a storage site for fat, and participates in our immunity. Copyright © 2009 Pearson Education, Inc. Tissues – Muscle and Nervous § Muscle tissue is responsible for movement. § Nervous tissue receives stimuli and conducts nerve impulses. Copyright © 2009 Pearson Education, Inc. Epithelial Tissue § Epithelial tissues - cover surfaces (epithelium) outside of the body (our skin), and lines internal cavities and tubes, including the inside surface of the stomach and the lungs (endothelium). § Functions are protection, secretion, and absorption, may contain glands. § Cells are tightly packed together. Copyright © 2009 Pearson Education, Inc. Glands § Many glands are composed of epithelial tissue. -

Medical Terminology
MEDICAL TERMINOLOGY THE INTEGUMENTARY SYSTEM MATCHING EXERCISES ANATOMICAL TERMS 1. keratin a. sweat glands 2. epidermis b. protein `gluey' substance in skin and tissue 3. collagen c. hard protein substance in epidermis, skin, 4.stratum corneum nails 5. sudoriferous glands d. outer layer of skin 6. melanocyte e. flat scale-like cells of outer epidermis 7. epithelium f. dense fibrous layer of skin (dermis) 8. sebum g. cell in basal layer that gives color to 9. corium skin 10. melanin h. cells covering external and internal surfaces i. oily substance from glands in skin j. dark pigment in melanocytes SYMPTOMATIC AND DIAGNOSTIC TERMS 1. macula a. small blister 2. nodule b. solid mass extending into epidermis 3. vesicle c. a wart 4. verruca d. small flat discolored spot on skin 5. keloid e. irregular overgrowth of scar tissue 6. urticaria f. spider angioma 7. comedo g. hives 8. telangiectasia h. eruptions 9. lupus i. blackhead 10. exanthemata j. chronic autoimmune disease 1. a `mangy fox' condition a. decubitus ulcer 2. a 'lying down' sore b. xanthoderma 3. dry skin c. tinea 4. moth-eaten skin condition d. alopecia 5. jaundice e. xeroderma 1. albinism a. localized thickening of skin caused by 2. onychia exposure to sun 3. pediculosis b. inflammation of nailfold 4. actinic keratosis c. congenital lack of melanin pigment 5. herpes zoster d. skin condition with inflamed vesicles that 6. psoriasis burst and scale 7. paronychia e. lice infestation 8. eczema f. inflammation of a nail 9. furuncle g. a boil 10. impetigo h. bacterial skin inflammation with rupturing pustules around mouth i. -
Integumentary System What Is Integument ?
Integumentary System What is integument ? The integument as an organ, and is an alternative name for skin. The integumentary system includes the skin and the skin derivatives hair, nails, and glands. The integument can also be thought of as a cutaneous membrane that covers the outer surface of the body. We lose almost a kg Introduction of skin epithelium a year that becomes a The Integument major part of household o Is the largest system of the body “dust”. o 16% of body weight o The integument is made up of two parts: 1. Cutaneous membrane a. Epidermis– Superficial epithelium b. Dermis – underlying CT with blood supply c. Hypodermis 2. Accessory structures a. Hair b. Nails c. Exocrine Glands Functions Protection o First line of defense against • Bacteria • Viruses o Protects underlying structures from • Ultraviolet (UV) radiation • Dehydration Vitamin D production o Needed for calcium absorption Sensation o Sensory receptors Funcitons Body temperature regulation o If too hot • Dermal blood vessels dilate • Vessels carry more blood to surface so heat can escape o If too cold • Dermal blood vessels constrict • Prevents heat from escaping Excretion o Small amounts of waste products are lost through perspiration Structure Understanding how the skin can function in these many ways starts with understanding the structure of the 3 layers of skin The Epidermis o Epithelial tissue Dermis o Dense connective tissue proper – irregular Hypodermis o Subcutaneous tissue- loose connective tissue proper and adipose tissue Structure /subcutaneous layer Structure/Epidermis The Epidermis is •A stratified squamous epithelia, composed of four to five layers (depending on body region) of epithelial cells. -

INTEGUMENTARY SYSTEM Abbreviations: @ at Lab Laboratory
INTEGUMENTARY SYSTEM Abbreviations: @ at Lab laboratory aa of each p after Bx, bx biopsy spec specimen C & S culture and sensitivity subQ subcutaneous s without c with drsg dressing Common Fundamental Terms: Edema = Puffy or swollen tissue from excess interstitial fluid Can be pitting or weeping Herpes simplex, virus (ex, simplex 1= fever-blisters) Diaphoresis = excessive perspiration due to distress not the same as hyperhydrosis! Melanin=brownish-black pigment Carotene = Yellowish-red pigment Albino = Absence of color pigments Erythema: Reddish color skin Jaundice: Yellow discoloration to the skin Pale/pallor: white in color Dermis: Called the true skin Subcutaneous tissue / fascia / hypodermis: Innermost layer of skin. Sudoriferous glands = sweat glands Sebaceous glands = oil glands sebum = oil Alopecia = baldness hypodermis = layer below the dermis papule = circumscribed, solid elevation of skin with no visible fluid, varying in size from a pinhead to 1 cm (red bump w/o a head) Lesion = any abnormality in the tissue of an organism purulent = pus induration = hard center Prefixes- Definitions Medical Terms Example Definitions of Terms Auto- self autopsy to view self postmortem autologous transfusion receiving your own blood bio- life biopsy to view a small piece of tissue biology study/science of life cutane/o-,cut- subcutaneous below dermis, under the skin dermat/o- dermatologist Dr. who studies skin diseases derm/a- pertaining to skin dermatitis inflammation of the skin inter- between intercellular between the cells intra- inside,