Integumentary System What Is Integument ?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diapositiva 1
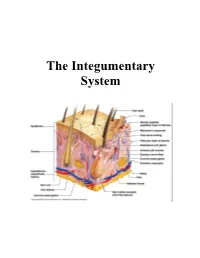
Ingegneria delle tecnologie per la salute Fondamenti di anatomia e istologia Apparato tegumentario aa. 2017-18 INTEGUMENTARY SYSTEM integumentary system = refers to skin and its accessory structures responsible for much more than simply human outward appearance: about 16% of body weight, covering an area of 1.5 to 2 m2 (= largest organ system in human body). • skin protects inner organs INTEGUMENTARY SYSTEM • skin = even not typical, but an organ, made of tissues that work together as a single structure to perform unique and critical functions • integumentary system = skin + its accessory structures, providing body with overall protection. • made of multiple layers of cells and tissues, which are held to underlying structures by connective tissue: deeper layer of skin is well vascularized (has numerous blood vessels) and also has numerous sensory, and autonomic and sympathetic nerve fibers ensuring communication to and from brain. INTEGUMENTARY SYSTEM Overview • Largest organ (15% of body weight) • Epidermis – keratinized stratified squamous epithelium • Dermis – connective tissue layer • Hypodermis • Thickness variable, normally 1-2 mm – dermis may thicken, up to 6 mm – stratum corneum layer increased • calluses on hands and feet Structure of the Skin 2 layers: epidermis + dermis SKIN: histology SKIN: histology SKIN: histology Cells of the Epidermis • Stem cells – undifferentiated cells in deepest layers • Keratinocytes – most of the skin cells • Melanocytes – synthesize pigment that shield UV • Tactile (merkel) cells – receptor cells associated with nerve fibers • Dendritic (langerhans) cells – macrophages guard against pathogens Cell and Layers of the Epidermis Epidermis: histology = composed of keratinized, stratified squamous epithelium, made of 4 or 5 layers of epithelial cells, depending on its location in body. -

CHAPTER 4 the Integumentary System
CHAPTER 4 The Integumentary System LEARNING OBJECTIVES Upon completion of this chapter, you should be able to: • Name the two layers of the skin. • Name the accessory structures of the integumentary system. • Build and pronounce medical terms of the integumentary system. • Name the disorders and treatments relating to the integumentary system. • Name the major classifi cations of pharmacologic agents used to treat skin disorders. • Analyze and defi ne the new terms introduced in this chapter. • Interpret abbreviations associated with the integumentary system. 53 54 PART TWO • BODY SYSTEMS Introduction The largest organ of the body is the skin. The skin covers the entire body—more than 20 square feet on average—and weighs about 24 pounds. It is part of the integumentary system, which also includes the accessory structures: hair, nails, and sebaceous (oil) and sudoriferous (sweat) glands. Integumentum is Latin for “covering” or “shelter.” The physician who specializes in the diag- nosis and treatment of skin disorders is called a dermatologist (dermat/o being one of the com- bining forms for skin). Coupling the root dermat/o with the previously learned suffi x -logy gives us the term dermatology , which is the term for the specialty practice that deals with the skin. Word Elements The major word elements that relate to the integumentary system consist of various anatomical components, accessory structures, colors of the skin, and abnormal conditions. The Word Ele- ments table lists many of the roots, their meanings, and examples associated -

Ch7 Basic Body Structure and Function Test&A
Chapter 7- Test Name: Basic Body Structure & Fuction Date: 1. Physiology is the study of A) what body parts look like and where they are located. B) the structure and function of the human body. C) how the various body parts work. D) how organisms are created. 2. The basic unit of life is A) a cell. B) a tissue. C) an organ. D) an organ system. 3. Which one of the following is like the cell's brain? A) The cytoplasm B) The cell nucleus C) The cell organelles D) The cell membrane 4. Which cell transports oxygen throughout the body? A) Red blood B) Epithelial C) Muscle D) Nerve 5. Which one of the following is considered connective tissue? A) Mucous membrane B) Blood C) Skin D) Glands 6. Which one of the following organs is included in the integumentary system? A) The fingernails B) The gallbladder C) The pancreas D) The ureters 7. What does epithelial tissue do? A) It connects tissues together. B) It produces movement. C) It conducts information. D) It protects the body. Page 1 8. Which statement correctly describes homeostasis? A) It causes problems by invading otherwise healthy tissues. B) It reduces the immune system's ability to fight off infection. C) It is a state of balance achieved by all of the organ systems working together. D) It occurs when the structure or function of an organ or organ system is abnormal. 9. The purpose of melanin is to A) keep the skin lubricated. B) aid in temperature regulation. C) give our skin, hair, and eyes color. -
The Integumentary System
The Integumentary System THE INTEGUMENTARY SYSTEM Skin is the system of the body that makes an individual beautiful! Skin/fur coloration allows animals to be camouflaged. *The skin is the largest organ of the body. The skin and its derivatives (hair, nails, sweat and oil glands) make up the integumentary system. The total surface area of the skin is about 1.8 m² and its total weight is about 11 kg. The skin gives us our appearance and shape. Anatomy of the Skin • Skin is made up of two layers that cover a third fatty layer. The outer layer is called the epidermis; it is a tough protective layer. The second layer (located under the epidermis) is called the dermis; it contains nerve endings, sweat glands, oil glands, and hair follicles. Under these two skin layers is a fatty layer called the subcutaneous tissue, or hypodermis. 1 • The dermis is home to the oil glands. These are also called sebaceous glands, and they are always producing sebum. Sebum is your skin's own natural oil. It rises to the surface of your epidermis to keep your skin lubricated and protected. It also makes your skin waterproof. • Skin is alive! It's made of many thin sheets of flat, stacked cells. Older cells are constantly being pushed to the surface by new cells, which grow from below. When the old ones reach the top, they become wider and flatter as they get rubbed and worn by all your activity. And, sooner or later, they end up popping off like tiles blown from a roof in a strong wind. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
The Integumentary System (In Teg Yoo MEN Tuh Ree) Skin, Tissues, and You � the Integumentary System Is the Body’S Outer Covering
The Integumentary System (In teg yoo MEN tuh ree) Skin, Tissues, and You ! " The Integumentary system is the body’s outer covering. It has the task of physically separating the body from the external environment. This is the first key to homeostasis. ! " Homeostasis: The internal stability or “steady state” maintained by your body. We maintain a body temperature of 98.6ºF (37ºC) ! " The Integumentary system isn’t perfect. Cuts and other injuries break the barrier of the system and allow microorganisms to enter the body. Also, extensive exposure to the sun can cause damage to the tissue. Other harmful agents can damage the system as well. http://academic.kellogg.edu/herbrandsonc/bio201_mckinley/f5-1_layers_of_the_inte_c.jpg The Skin and Tissue Tissues ! " Your body contains 250 different types of cells. ! " Groups of similar cells with common function are called tissues. ! " Tissues protect the body, connect body parts together, some lift and move the body, some transmit http://asweknowit.net/images_edu/dwa5%20tissues.jpg information. Epithelial Tissue ! " Epithelial tissue: sheets of closely packed cells that cover the entire surface of your body and form the lining of your internal organs, many different types all serve the general function of protecting the tissues and organs they cover ! " In your respiratory system, ! " 1st type; line your windpipe and its major branches, cells secrete mucus which traps dust, pollen. etc. cilia sweep them up to throat to be swallowed, ! " 2nd type; lines narrower airways cells have smooth surface allows -

Body Systems Work Together by Cindy Grigg
Body Systems Work Together By Cindy Grigg 1 You know that your body is made of cells. When groups of cells do the same kind of work, they are called tissues. The word tissue comes from a Latin word meaning to "weave." Cells that make up tissues are sometimes "woven" together. 2 You have four main types of tissues: epithelial, nervous, muscle, and connective tissue. Epithelial tissue covers the outside of the body. It also lines organs and cavities. Nervous tissue sends electrical signals. Muscle tissue helps you move. Connective tissue joins bones and cushions organs. 3 When groups of tissues work together, they are called organs. Some examples of organs are the heart, lungs, skin, and stomach. When organs work together, they are called systems. For example, your heart, lungs, blood, and blood vessels work together. They make up the circulatory system. 4 There are eleven systems in the human body: muscular system, respiratory system, digestive system, integumentary system (skin), skeletal system, circulatory (or cardiovascular) system, excretory (or urinary) system, reproductive system, nervous system, lymphatic system, and endocrine system. Each system has a special job. 5 All of your body systems have to work together to keep you healthy. Your bones and muscles work together to support and move your body. Your respiratory system takes in oxygen from the air. It also gets rid of carbon dioxide. 6 Your digestive system absorbs water and nutrients from the food you eat. 7 Your circulatory system carries oxygen, water, and nutrients to cells throughout your body. Wastes from the cells are eliminated by your respiratory system, your excretory system, and your skin. -

Medical Literacy Bridge
Written by Jack McGrath Layout and computer assistance by Kathy Yeomans Edited by Jack McGrath and Kathy Yeomans DVD by Terry Weiser, VACE Technology Development Center Supervision by Steve Thompson Special thanks to the Workforce Investment Board of Ventura County Printed by Ventura Unified School District The Workforce Investment Board of Ventura County sponsored the creation of this curriculum based on a contract awarded to Ventura Adult and Continuing Education. The curriculum is the result of VACE’s observations regarding student success rate for English Language Learners and basic literacy English speakers who enroll in Allied Health training programs. Introduction: Medical Literacy Bridge ............................................................................................................................. 1 A Bridge to Medical Terminology ...................................................................................................................................................... 2 DVD instructions ....................................................................................................................................................................................... 2 Memory Techniques ................................................................................................................................................................................ 2 English Word Study and Medical Text Books .............................................................................................................................. -

Basic Biology of the Skin 3
© Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION CHAPTER Basic Biology of the Skin 3 The skin is often underestimated for its impor- Layers of the skin: tance in health and disease. As a consequence, it’s frequently understudied by chiropractic students 1. Epidermis—the outer most layer of the skin (and perhaps, under-taught by chiropractic that is divided into the following fi ve layers school faculty). It is not our intention to present a from top to bottom. These layers can be mi- comprehensive review of anatomy and physiol- croscopically identifi ed: ogy of the skin, but rather a review of the basic Stratum corneum—also known as the biology of the skin as a prerequisite to the study horny cell layer, consisting mainly of kera- of pathophysiology of skin disease and the study tinocytes (fl at squamous cells) containing of diagnosis and treatment of skin disorders and a protein known as keratin. The thick layer diseases. The following material is presented in prevents water loss and prevents the entry an easy-to-read point format, which, though brief of bacteria. The thickness can vary region- in content, is suffi cient to provide a refresher ally. For example, the stratum corneum of course to mid-level or upper-level chiropractic the hands and feet are thick as they are students and chiropractors. more prone to injury. This layer is continu- Please refer to Figure 3-1, a cross-sectional ously shed but is replaced by new cells from drawing of the skin. This represents a typical the stratum basale (basal cell layer). -

Human Body Systems
INTEREST GRABBER – NOTEBOOK #1 AN IMPORTANT PROCESS While walking along a dusty path, you begin to cough. As you continue your walk, a small insect comes flying toward you. You blink and then duck so that it misses you. These actions are just a few examples of homeostasis. Homeostasis is the process by which organisms keep internal conditions relatively constant despite changes in their external environments. 1. List three other examples of homeostasis that occur in organisms. 2. Why is homeostasis important to an organism? INTEREST GRABBER 1. List three other examples of homeostasis that occur in organisms. Accept all reasonable student examples that show an understanding of homeostasis. 2. Why is homeostasis important to an organism? Homeostasis allows an organism to remain in balance with its environment. If homeostasis is not maintained, it can harm the organism or result in the death of the organism. LEVELS OF ORGANIZATION IN A MULTICELLULAR ORGANISM Cell Tissue Organ Organ system Complete organism NERVOUS SYSTEM - controls and coordinates functions throughout the body and responds to internal and external stimuli Nervous System Integumentary System Skeletal System Muscular System Circulatory System NERVOUS SYSTEM Structures: Brain, spinal cord, peripheral nerves Function: Recognizes and coordinates the body’s response to changes in the internal and external environments NERVOUS SYSTEM - THE SYNAPSE Direction of Impulse Dendrite of -chemical messages adjacent neuron Axon Receptor (neurotransmitters) Vesicle are sent to the Axon synapse -
The Integumentary System the Integumentary System
Essentials of Anatomy & Physiology, 4th Edition Martini / Bartholomew The Integumentary System PowerPoint® Lecture Outlines prepared by Alan Magid, Duke University Slides 1 to 51 Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Integumentary System Components • Cutaneous membrane • Epidermis • Dermis • Accessory structures • Subcutaneous layer (hypodermis) Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Main Functions of the Integument • Protection • Temperature maintenance • Synthesis and storage of nutrients • Sensory reception • Excretion and secretion Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Components of the Integumentary System Figure 5-1 Integumentary Structure/Function The Epidermis • Stratified squamous epithelium • Several distinct cell layers • Thick skin—five layers • On palms and soles • Thin skin—four layers • On rest of body Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function Cell Layers of The Epidermis • Stratum germinativum • Stratum spinosum • Stratum granulosum • Stratum lucidum (in thick skin) • Stratum corneum • Dying superficial layer • Keratin accumulation Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Integumentary Structure/Function The Structure of the Epidermis Figure 5-2 Integumentary Structure/Function Cell Layers of The Epidermis • Stratum germinativum -
The Integumentary System the Integumentary System
The Integumentary System The Integumentary System Integument is skin Skin and its appendages make up the integumentary system A fatty layer (hypodermis) lies deep to it Two distinct regions Epidermis Dermis Epidermis Keratinized stratified squamous epithelium Four types of cells Keratinocytes – deepest, produce keratin (tough fibrous protein) Melanocytes - make dark skin pigment melanin Merkel cells – associated with sensory nerve endings Langerhans cells – macrophage-like dendritic cells Layers (from deep to superficial) Stratum basale or germinativum – single row of cells attached to dermis; youngest cells Stratum spinosum – spinyness is artifactual; tonofilaments (bundles of protein) resist tension Stratum granulosum – layers of flattened keratinocytes producing keratin (hair and nails made of it also) Stratum lucidum (only on palms and soles) Stratum corneum – horny layer (cells dead, many layers thick) (see figure on next slide) Epithelium: layers (on left) and cell types (on right) Dermis Strong, flexible connective tissue: your “hide” Cells: fibroblasts, macrophages, mast cells, WBCs Fiber types: collagen, elastic, reticular Rich supply of nerves and vessels Critical role in temperature regulation (the vessels) Two layers (see next slides) Papillary – areolar connective tissue; includes dermal papillae Reticular – “reticulum” (network) of collagen and reticular fibers *Dermis layers *Dermal papillae * * Epidermis and dermis of (a) thick skin and (b) thin skin (which one makes the difference?) Fingerprints,