Guidelines for Assessing and Treating Anxiety Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diet Manual for Long-Term Care Residents 2014 Revision
1 Diet Manual for Long-Term Care Residents 2014 Revision The Office of Health Care Quality is pleased to release the latest revision of the Diet Manual for Long-Term Care Residents. This manual is a premier publication—serving as a resource for providers, health care facilities, caregivers and families across the nation. In long-term care facilities, meeting nutritional requirements is not as easy as it sounds. It is important to provide a wide variety of food choices that satisfy each resident’s physical, ethnic, cultural, and social needs and preferences. These considerations could last for months or even years. Effective nutritional planning, as well as service of attractive, tasty, well-prepared food can greatly enhance the quality of life for long-term care residents. The Diet Manual for Long Term Care Residents was conceived and developed to provide guidance and assistance to nursing home personnel. It has also been used successfully in community health programs, chronic rehabilitation, and assisted living programs. It serves as a guide in prescribing diets, an aid in planning regular and therapeutic diet menus, and as a reference for developing recipes and preparing diets. The publication is not intended to be a nutrition-care manual or a substitute for individualized judgment of a qualified professional. Also included, is an appendix that contains valuable information to assess residents’ nutritional status. On behalf of the entire OHCQ agency, I would like to thank the nutrition experts who volunteered countless hours to produce this valuable tool. We also appreciate Beth Bremner and Cheryl Cook for typing the manual. -

Unilever to Spread Magnum Vegan Reach As Trend Set to Mainstream In
Food and Beverage Innovation December 2018 - 2019 February Volume 17 ISSN 1570-9108 DOUBLE ISSUE Unilever to spread Magnum Vegan reach as trend set to mainstream in 2019 Unilever has introduced its Magnum suitability going forward, with plant-based Vegan ice cream to Australian markets milks and meat substitutes already rapidly with more European markets to follow this moving into the mainstream. year, as the trend towards reformulating The rise of veganism is indicative classic items in vegan forms accelerates. of a growing theme towards mindful At launch, Unilever, described it as a consumption. “velvety plant-based product” that provides Animal welfare and environmental “a creamy experience without the need concerns form clear goals among the for dairy.” “A first for the Australian following of such a strict diet. Vegan market, the 100 percent dairy-free range products are increasingly associated to will feature two of the brand’s signature ethical packaging (50 percent), organic flavors…allowing vegans the opportunity (31 percent), gluten-free (34 percent) and to enjoy and share a moment of pure GMO-free (27 percent) (CAGR 2014-2018). pleasure,” the company said. In 2018, 60 percent of all products with Last year, two new vegan versions vegan claims were reported in Europe. of the popular Magnum ice cream bars continued on page 3 were launched in Sweden and Finland. TOP MARKETTop SUBCATEGORIES market subcategories OF FOOD & BEVERAGES of food LAUNCHES & beverages WITH A “VEGAN” launches CLAIM (GLOBAL, 2018) Magnum Vegan Classic and Magnum with a “vegan” claim (Global, 2018) Vegan Almond, which are European Vegetarian Union approved, are made 6 from a pea protein base and covered in smooth dark chocolate. -

1. Introduction
1. INTRODUCTION 1.1 Background to Unilever Sri Lanka Unilever's association with the country, Ceylon at the time, began in the early 1900s with brands such as Sunlight, Lux and Pears Rose being available for sale in the local market. In 1927 imports and distribution was organised with the appointment of a sole agent Sankar Aiyars. In 1938, with the sales of Sunlight reaching 2000 tons and Lux reaching 200 tons Lever Brothers Ceylon Limited was incorporated. This was followed with the establishment of a soap factory in Grandpass Colombo in April 1940. Bakery fats and Margarine manufacture commenced in 1941 and in 1958 the company established its own selling and distribution organisation (Sankalana, 2009). Over the years the organisation expanded and the business activities of Unilever were managed through Lever Brothers Ceylon Limited, Lipton, Brooke Bond, Ceytea, Lever Aqua Products and Premier Foods. The organisation was restructured in 1991 to bring all legal entities under the umbrella of Unilever Ceylon. Since then the business was managed by two divisions namely Consumer Division and Tea Division. Since 1996, the consolidated business entity is known as Unilever Sri Lanka Limited (USL) with its head office and main food and home and personal care (HPC) factory in Grandpass, Colombo. This plant manufactures a large range of fast moving consumer goods such as toilet soaps, hard soaps, washing powders, shampoos, toothpaste and margarine. This site employs around 1270 permanent employees. Non soap detergent (NSD) plant, hard soap packing plant and the distribution centre are located at the Lindel industrial site in Sapugaskanda, about 15 km away from the Grandpass office. -

Brexit Fallout Spreads to Britain's Famous Marmite
Business38 FRIDAY, OCTOBER 14, 2016 Amazon adding 120,000 workers to meet holiday demand NEW YORK: Amazon.com will add 120,000 seasonal work- ers in an effort to meet an expected spike in demand dur- ing the holidays. The seasonal positions will be created at fulfillment centers, sorting centers and customer service sites in 27 states. The move marks a 20 percent boost from the 100,000 seasonal hires a year ago. Last year, the company said it transitioned 14,000 seasonal positions to regular, full-time jobs and it expects to boost that figure this year. The e-commerce giant saw its fourth-quarter profit in 2015 more than double on higher demand from online shoppers during the holiday season. — AP Delta beats 3Q profit forecasts LONDON: Jars of savoury spread ‘Marmite’ which is owned by the Anglo-Dutch multinational Unilever, on sale in a ATLANTA: Delta Air Lines Inc. (DAL) yesterday reported third- branch of Tesco yesterday. — AP quarter profit of $1.26 billion. On a per-share basis, the Atlanta-based company said it had profit of $1.69. Earnings, adjusted for non-recurring costs, came to $1.70 per share. Brexit fallout spreads to The results surpassed Wall Street expectations. The aver- age estimate of nine analysts surveyed by Zacks Investment Research was for earnings of $1.65 per share. The airline post- Britain’s famous Marmite ed revenue of $10.48 billion in the period, falling short of Street forecasts. Four analysts surveyed by Zacks expected $10.59 billion. Delta shares have declined 23 percent since the A squeeze in revenues beginning of the year, while the Standard & Poor’s 500 index has risen roughly 5 percent. -
Kosher Nosh Guide Summer 2020
k Kosher Nosh Guide Summer 2020 For the latest information check www.isitkosher.uk CONTENTS 5 USING THE PRODUCT LISTINGS 5 EXPLANATION OF KASHRUT SYMBOLS 5 PROBLEMATIC E NUMBERS 6 BISCUITS 6 BREAD 7 CHOCOLATE & SWEET SPREADS 7 CONFECTIONERY 18 CRACKERS, RICE & CORN CAKES 18 CRISPS & SNACKS 20 DESSERTS 21 ENERGY & PROTEIN SNACKS 22 ENERGY DRINKS 23 FRUIT SNACKS 24 HOT CHOCOLATE & MALTED DRINKS 24 ICE CREAM CONES & WAFERS 25 ICE CREAMS, LOLLIES & SORBET 29 MILK SHAKES & MIXES 30 NUTS & SEEDS 31 PEANUT BUTTER & MARMITE 31 POPCORN 31 SNACK BARS 34 SOFT DRINKS 42 SUGAR FREE CONFECTIONERY 43 SYRUPS & TOPPINGS 43 YOGHURT DRINKS 44 YOGHURTS & DAIRY DESSERTS The information in this guide is only applicable to products made for the UK market. All details are correct at the time of going to press but are subject to change. For the latest information check www.isitkosher.uk. Sign up for email alerts and updates on www.kosher.org.uk or join Facebook KLBD Kosher Direct. No assumptions should be made about the kosher status of products not listed, even if others in the range are approved or certified. It is preferable, whenever possible, to buy products made under Rabbinical supervision. WARNING: The designation ‘Parev’ does not guarantee that a product is suitable for those with dairy or lactose intolerance. WARNING: The ‘Nut Free’ symbol is displayed next to a product based on information from manufacturers. The KLBD takes no responsibility for this designation. You are advised to check the allergen information on each product. k GUESS WHAT'S IN YOUR FOOD k USING THE PRODUCT LISTINGS Hi Noshers! PRODUCTS WHICH ARE KLBD CERTIFIED Even in these difficult times, and perhaps now more than ever, Like many kashrut authorities around the world, the KLBD uses the American we need our Nosh! kosher logo system. -

YVS STOCK LIST 1St JULY 20
FLAT NUMBER: Type Name Price How Many BAKERY Hovis - Wholemeal £1.60 BAKERY Hovis - Soft White £1.50 BAKERY Pita Bread - white (6) £1.10 BAKERY Granary Bread £1.70 BAKERY Hovis small wholemeal loaf £1.10 BAKERY Pita Bread - wholemeal (6) £1.10 BAKERY DTC - Oven Baked White Baguettes (2) £0.85 BATHROOM & CLEANING Anti-bacterial Handwash (500ml) £1.00 BATHROOM & CLEANING Carex - Anti-bacterial Handwash £1.50 BATHROOM & CLEANING Comfort - Fabric Conditioner (Sunshiny) £1.99 BATHROOM & CLEANING Cushelle - Original (9 roll) £5.49 BATHROOM & CLEANING Toilet DucK Marine 750ml £1.29 BATHROOM & CLEANING Fairy Non Bio Washing Pods x15 £4.49 BATHROOM & CLEANING Domestos - Regular Blue Bleach £1.00 BATHROOM & CLEANING Happy Shopper - Family Tissues £1.00 BATHROOM & CLEANING Imperial Leather - Talcum Powder £1.49 BATHROOM & CLEANING Fairy Washing Up Liquid Orginal 433ml £1.29 BATHROOM & CLEANING Spontex - 2 Washups sponges £0.95 BATHROOM & CLEANING Cif - Lemon (250ml) £1.49 BATHROOM & CLEANING Raid - Fly & Wasp Killer £2.99 BATHROOM & CLEANING Flash Multi Surface Ultra Power Concentrate 400ml £1.49 BATHROOM & CLEANING Flash Spray with bleach £1.91 BATHROOM & CLEANING Bold - 2in1 Washing Powder £2.99 BATHROOM & CLEANING Comfort - Fabric Conditioner (Blue SKies) £1.99 BATHROOM & CLEANING Sponges - Tough Scourers £1.00 BATHROOM & CLEANING Best-one - 3 Sponges £0.59 BATHROOM & CLEANING Dettol surface wipes £6.50 BATHROOM & CLEANING Daz washing liquid £2.99 BATHROOM & CLEANING Persil Washing Powder - Non-Bio £2.99 BATHROOM & CLEANING Andrex - Supreme Quilt -

EXAMPLES of MEAL PLANS 3 MEALS Breaksfast
EXAMPLES OF MEAL PLANS 3 MEALS Breaksfast - Smoothie - Strawberry shake with 150g mixed berries Lunch - 2 crackerbread with Bovril & an apple Dinner - 90g Roast with 90g onion, mushrooms, peppers, carrots and potato (only if it’s the 5 th meal) and Beef Cup a soup 3 MEALS Breakfast – 1 whole egg + 2 egg whites & 90g mushrooms (scrambled eggs) Lunch – 3 Provitas with Bovril & fruit salad (an apple + 150g pawpaw & strawberries) Dinner – 90g extra lean mince with a gem squash (add mince to one half and cinnamon + sweetener to other half) 4 MEALS Breakfast – A nectarine with 1 crackerbread/2 small melba toast with marmite Lunch – 175ml Fabulite fatfree Strawberry yoghurt + 90g carrot sticks / cherry tomatoes Snack – Cup a Soup with 1 crackerbread/2 small melba toast + half a medium grapefruit Dinner – 90g extra lean Mince with mash (only if it’s the 5 th meal) 4 MEALS Breakfast – 150g water melon Lunch - 2 crackerbread with 70g smoked chicken/pastrami (only 70g since it’s not raw weight), mustard and tomato Snack – Cup a Soup & an apple Dinner – 90g Steak with 90g salad (baby spinach leaves, rocket, cherry tomatoes, peppers, cucumber) 4 MEALS Breakfast – An orange and 1 provita with marmite Lunch – 175ml Fabulite fatfree Black Cherry yoghurt with 90g carrot / cucumber strips Snack – An apple and 1 crackerbread with marmite Dinner – 90g fresh Hake fillet (bake in oven with some Thyme & garlic flakes + lemon juice for great flavour) & 90g mixed veg or a potato (if 5 th meal) 4 MEALS Breakfast – Half a medium grapefruit & 2 small melba toast -

Salicylate Food and Product Shopping Lists Last Updated: January 31 2021
p. 1 Salicylate Food and Product Shopping Lists Last Updated: January 31 2021 Formatted for shopping convenience from The Low-Sal Life Go to the website at https://low-sal-life.com/food-product-lists#products for more data on each item, the year and sources for that data, and their complete and awesome list of citations, studies and research: “There have been five major studies testing salicylates in food over the last forty years. I will categorize food by the highest study's levels which includes Free + Bound Salicylic Acid levels, but also include all the historical results. Please take caution while trying new foods. Also note, that the food industry has changed and scientific methods improved in 40 years which may be a few reasons why salicylate levels have changed. Malakar et al. reports all levels with free plus bound salicylic acid, not just free like Swain et al. 1985. This may explain why levels are higher than before. Kęszycka also reports both free and bound, but provides the levels separately. This is why white rice is no longer in the negligible list - it has a low level when including bound salicylic acid. While it's not known how the body metabolizes bound salicylates, it's good to know what the full potential is. The best way to use this list is to search for the food item with your browser search - look for ALL the mentions. For example, figs are listed in three categories depending on how they are preserved. Also, some foods were not included in the five research articles, so I've included items like the St. -
Britain Panics Over Brexit-Sparked Marmite Shortage
WORLD UNITED KINGDOM Britain Panics Over Brexit-Sparked Marmite Shortage Tesco pulled a range of products from its website following a pricing row with Unilever News that a major British supermarket will no longer be stocking Marmite following Brexit has sparked outrage across the U.K., leading the hashtag #MarmiteGate to trend on Twitter. Tesco pulled a range of products, including Marmite, PG Tips tea bags, Ben & Jerry’s ice cream, Persil washing powder and Lynx body spray, from its website after a row over pricing with the major food and household goods supplier Unilever. According to The Guardian, Unilever is trying to charge Tesco an extra 10% for its goods due to the pound’s fall against the euro and the dollar following the vote for Brexit in June. Graeme Pitkethly, Unilever’s chief financial officer, described these price increases as a “normal” part of business. “We are taking price increases in the UK. That is a normal devaluation-led cycle,” he told analysts. Promoted Recommended by Nick Sutton 12 Oct @suttonnick Down to the last three jars of Marmite at a local Tesco pic.twitter.com/DJVm6lhGhC Nick Sutton Follow @suttonnick Only two jars of Marmite left this morning. #marmitewatch pic.twitter.com/T8NIHpKpda 6:20 AM - 13 Oct 2016 44 47 Marmite fans have not taken the news well, packing social media full of photos of shelves being emptied of the “love it or hate it” yeast spread. Tubs of Marmite have even gone on sale on eBay for up to £4million ($4.78 million)—although no bids have been placed so far. -

Carb Counter
HOW TO USE THE ATKINS® CARB COUNTER HE CARB COUNTER has one purpose only—to tell you the Atkins net carb CARB COUNTER count of as many foods as humanly possible. It is not a calorie counter, nor is it a T comprehensive encyclopedia of food counts. You won’t learn how much calcium 3 How to Use the 27 Fruit a food has, how many grams of omega-6 fat, how much protein or how much vitamin Atkins Carb Counter C. All of that information is available elsewhere. What is not widely available—until 30 Grains, Noodles & Pasta now—is a way of answering the all-important question, “How many net carbs does 5 Atkins & Other this portion of food that I’m about to eat contain?” Low-Carb Specialty Foods 32 Legumes Knowing that number is going to make it possible for you to do Atkins the right way, 8 Baking Ingredients 33 Nuts & Seeds the effective way, and the way that works for you, no matter what Atkins DietTM plan 9 Beef, Lamb, Pork 35 Oils, Fats, Vinegar (Atkins 20® or Atkins 40®) you’re on. & Other Meats & Salad Dressings What’s more, we based our net carb counts on realistic amounts of food—the amount 37 Poultry 11 Beverages & of a food you’re actually likely to eat! Remember, manufacturers are famous for making Alcoholic Beverages 38 Sauces & Marinades “serving sizes” ridiculously unrealistic in order to make their numbers look less bad. 14 Breads, Crackers, We’ve all seen examples of this: A single cookie you’d eat in two bites is labeled 41 Tortillas & Wraps Snacks “2 servings” with “1/2 cookie” constituting one “serving”; or a small 8 ounce bottle of juice at the convenience store with a label claiming it’s “2 servings”. -
12/15/2019 4:22 PM Page 1 of 120
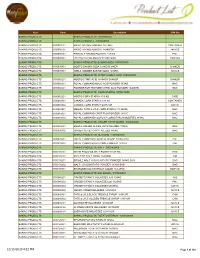
Item Code Description U/M Set BAKING PRODUCTS BAKING PRODUCTS - 0300000000 BAKING PRODUCTS BAKING POWDER - 0300080000 BAKING PRODUCTS 0300080101 MAGIC BAKING POWDER 1X2.5KG CONTAINER BAKING PRODUCTS 0300080102 MAGIC BAKING POWDER 24X450GR 24X1CS BAKING PRODUCTS 0300080201 PINNACLE BAKING POWDER 1X5 KG PAIL BAKING PRODUCTS 0300080301 LIEVITO BAKING POWDER 100X16GR 100X1CS BAKING PRODUCTS BAKING PRODUCTS: BAKING SODA -0300030000 BAKING PRODUCTS 0300030401 MOSTO BAKING SODA 1X1KG SHAKER SHAKER BAKING PRODUCTS 0300030501 ARM & HAMMER BAKING SODA 12X2KG 12X1CS BAKING PRODUCTS BAKING PRODUCTS: CITRIC & MALIC ACID -0300060000 BAKING PRODUCTS 0300060201 MOSTO CITRIC ACID 1X454GR SHAKER SHAKER BAKING PRODUCTS 0300060301 ROYAL COMMAND MALIC ACID POWDER 1X1KG BAG BAKING PRODUCTS 0300060401 POWDER FOR TEXTURE CITRIC ACID POWDER 1X400GR BAG BAKING PRODUCTS BAKING PRODUCTS: CORN STARCH -0300010000 BAKING PRODUCTS 0300010201 MOSTO CORN STARCH 1X5 KG CASE BAKING PRODUCTS 0300010301 CANADA CORN STARCH 1X1 KG CONTAINER BAKING PRODUCTS 0300010302 CANADA CORN STARCH 6X454GR 6X1CS BAKING PRODUCTS 0300010501 MEOJEL TATE & LYLE CORN STARCH 1X 50LBS BAG BAKING PRODUCTS 0300010601 ROYAL COMMAND CRISP FILM POWDER 1X1KG BAG BAKING PRODUCTS 0300010602 ROYAL COMMAND COLFO 67 CORNSTARCH MODIFIED 1X1KG BAG BAKING PRODUCTS BAKING PRODUCTS: GINGER CRYSTALIZED - 0300050000 BAKING PRODUCTS 0300050301 MOSTO GINGER SLICES CRYSTALLIZED 1X1KG BAG BAKING PRODUCTS 0300050302 GINGER SLICES CRYSTALLIZED 1X5KG BAG BAKING PRODUCTS BAKING PRODUCTS: GLUCOSE - 0300020000 BAKING PRODUCTS -

The Holmes Report 2017 Book After Awards and Events Around the +1 914 450 3462 Was Designed by 05Creative* World
THE AGENCY HOLMES RANKINGS REPORT IN2 SABRE AWARDS THE 2017 THE SABRE HOLMES AWARDS REPORT EMEA 2017 The Best Agencies, Campaigns, Influencers and Stories of the Year AGENCY OF THE YEAR IN2 INNOVATION SUMMIT 2017 THE THE INFLUENCE INNOVATOR 100 25 2017 2017 THE GLOBAL EDITION GLOBAL PR SUMMIT 2017 THE “Proving and improving the value of HOLMES public relations” REPORT Paul Holmes The Holmes Group is dedicated to Paul Holmes North America proving and improving the value of Founder & Chair The Holmes Group public relations, by providing [email protected] 271 West 47th Street insight, knowledge and recognition Suite 23-A Arun Sudhaman to public relations professionals. New York, NY 10036 CEO & Editor-in-Chief +1 212 333 2300 The Holmes Group was founded in +852 96187774 2000 by Paul Holmes, publisher and [email protected] Europe CEO, who has more than two decades The Holmes Group Aarti Shah of experience writing about and 6 Sussex Mews West Head of Strategic Partnerships evaluating the public relations W2 2SE & Operations United Kingdom Holmes Report’s delivers — not only +1 510 808 5855 +44 (0)203 238 2048 the most sophisticated reporting and [email protected] analysis on PR trends and issues — Diana Marszalek but also the industry’s most sought- Senior Reporter (New York) The Holmes Report 2017 book after awards and events around the +1 914 450 3462 was designed by 05creative* world. [email protected] Celeste Picco Administrative +1 212 333 2300 [email protected] Patrick Drury Event Manager +1 732 299 1847 [email protected]