Costello Syndrome: Clinical Phenotype, Genotype, and Management Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
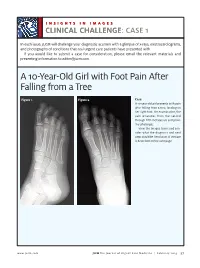
A 10-Year-Old Girl with Foot Pain After Falling from a Tree
INSIGHTS IN IMAGES CLINICAL CHALLENGECHALLENGE: CASE 1 In each issue, JUCM will challenge your diagnostic acumen with a glimpse of x-rays, electrocardiograms, and photographs of conditions that real urgent care patients have presented with. If you would like to submit a case for consideration, please email the relevant materials and presenting information to [email protected]. A 10-Year-Old Girl with Foot Pain After Falling from a Tree Figure 1. Figure 2. Case A 10-year-old girl presents with pain after falling from a tree, landing on her right foot. On examination, the pain emanates from the second through fifth metatarsals and proxi- mal phalanges. View the images taken and con- sider what the diagnosis and next steps would be. Resolution of the case is described on the next page. www.jucm.com JUCM The Journal of Urgent Care Medicine | February 2019 37 INSIGHTS IN IMAGES: CLINICAL CHALLENGE THE RESOLUTION Figure 1. Mediastinal air Figure 1. Differential Diagnosis Pearls for Urgent Care Management and Ⅲ Fracture of the distal fourth metatarsal Considerations for Transfer Ⅲ Plantar plate disruption Ⅲ Emergent transfer should be considered with associated neu- Ⅲ Sesamoiditis rologic deficit, compartment syndrome, open fracture, or vas- Ⅲ Turf toe cular compromise Ⅲ Referral to an orthopedist is warranted in the case of an in- Diagnosis tra-articular fracture, or with Lisfranc ligament injury or ten- Angulation of the distal fourth metatarsal metaphyseal cortex derness over the Lisfranc ligament and hairline lucency consistent with fracture. Acknowledgment: Images courtesy of Teleradiology Associates. Learnings/What to Look for Ⅲ Proximal metatarsal fractures are most often caused by crush- ing or direct blows Ⅲ In athletes, an axial load placed on a plantar-flexed foot should raise suspicion of a Lisfranc injury 38 JUCM The Journal of Urgent Care Medicine | February 2019 www.jucm.com INSIGHTS IN IMAGES CLINICAL CHALLENGE: CASE 2 A 55-Year-Old Man with 3 Hours of Epigastric Pain 55 years PR 249 QRSD 90 QT 471 QTc 425 AXES P 64 QRS -35 T 30 Figure 1. -

Genetic Mechanisms of Disease in Children: a New Look
Genetic Mechanisms of Disease in Children: A New Look Laurie Demmer, MD Tufts Medical Center and the Floating Hospital for Children Boston, MA Traditionally genetic disorders have been linked to the ‘one gene-one protein-one disease’ hypothesis. However recent advances in the field of molecular biology and biotechnology have afforded us the opportunity to greatly expand our knowledge of genetics, and we now know that the mechanisms of inherited disorders are often significantly more complex, and consequently, much more intriguing, than originally thought. Classical mendelian disorders with relatively simple genetic mechanisms do exist, but turn out to be far more rare than originally thought. All patients with sickle cell disease for example, carry the same A-to-T point mutation in the sixth codon of the beta globin gene. This results in a glutamate to valine substitution which changes the shape and the function of the globin molecule in a predictable way. Similarly, all patients with achondroplasia have a single base pair substitution at nucleotide #1138 of the FGFR3 gene. On the other hand, another common inherited disorder, cystic fibrosis, is known to result from changes in a specific transmembrane receptor (CFTR), but over 1000 different disease-causing mutations have been reported in this single gene. Since most commercial labs only test for between 23-100 different mutations, interpreting CFTR mutation testing is significantly complicated by the known risk of false negative results. Many examples of complex, or non-Mendelian, inheritance are now known to exist and include disorders of trinucleotide repeats, errors in imprinting, and gene dosage effects. -

Segmental Overvekst Og Vaskulærmalformasjoner V02
2/1/2021 Segmental overvekst og vaskulærmalformasjoner v02 Avdeling for medisinsk genetikk Segmental overvekst og vaskulærmalformasjoner Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* ACVRL1 175 NM_000020.3 2-10 Telangiectasia, hereditary hemorrhagic, type 2 OMIM ADAMTS3 219 NM_014243.3 1-22 Hennekam lymphangiectasia- lymphedema syndrome 3 OMIM AKT1 391 NM_005163.2 2-14 Cowden syndrome 6 OMIM Proteus syndrome, somatic OMIM AKT2 392 NM_001626.6 2-14 Diabetes mellitus, type II OMIM Hypoinsulinemic hypoglycemia with hemihypertrophy OMIM AKT3 393 NM_005465.7 2-14 Megalencephaly-polymicrogyria- polydactyly-hydrocephalus syndrome 2 OMIM file:///data/SegOv_v02-web.html 1/7 2/1/2021 Segmental overvekst og vaskulærmalformasjoner v02 Ekson Gen Gen affisert (HGNC (HGNC -

Master List of References ACADVL 1
Last Revision: 6/2017 DEPARTMENT OF PATHOLOGY AND LABORATORY MEDICINE PRECISION DIAGNOSTICS – INHERITED DISEASE Master List of References ACADVL 1. Mathur A, Sims HF, Gopalakrishnan D et al. Molecular heterogeneity in very-long-chain acyl-CoA dehydrogenase deficiency causing pediatric cardiomyopathy and sudden death. Circulation 1999;99:1337-43. [PMID: 10077518] 2. Vianey-Saban C, Divry P, Brivet M et al. Mitochondrial very-long-chain acyl-coenzyme A dehydrogenase deficiency: Clinical characteristics and diagnostic considerations in 30 patients. Clin Chim Acta 1998;269:43-62. [PMID: 9498103] AR 1. Giagulli VA, Carbone MD, De Pergola G, et al. Could androgen receptor gene CAG tract polymorphism affect spermatogenesis in men with idiopathic infertility? J Assist Reprod Genet 2014;31(6):689-97. [PMID: 24691874] 2. Gottlieb B, Beitel LK, Nadarajah A, et al. The androgen receptor gene mutations database (ARDB): 2012 update. Hum Mutat. 2012;33:887-94. [PMID: 22334387] Array CGH 1. Boone PM, Bacino CA, Shaw CA et al., Detection of clinically relevant exonic copy-number changes by array CGH. Hum Mutat 2010;31(12):1326-1342. [PMID: 20848651] CFTR 1. Collaco AM, Geibel P, Lee BS et al. Functional vacuolar ATPase (V-ATPase) proton pumps traffic to the enterocyte brush border membrane and require CFTR. Am J Physiol Cell Physiol 2013;305(9):C981-996. [PMID: 23986201] 2. Lu S, Yang X, Li X et al. Different cystic fibrosis transmembrane coductance regulator mutations in Chinese men with congenital bilateral absence of vas deferens and other acquired obtructive azoospermia. Urology 2013;82(4):824-828. [PMID: 23953609] 3. Sosnay PR, Siklosi KR, Van Goor F et al. -

Orthopedic-Conditions-Treated.Pdf
Orthopedic and Orthopedic Surgery Conditions Treated Accessory navicular bone Achondroplasia ACL injury Acromioclavicular (AC) joint Acromioclavicular (AC) joint Adamantinoma arthritis sprain Aneurysmal bone cyst Angiosarcoma Ankle arthritis Apophysitis Arthrogryposis Aseptic necrosis Askin tumor Avascular necrosis Benign bone tumor Biceps tear Biceps tendinitis Blount’s disease Bone cancer Bone metastasis Bowlegged deformity Brachial plexus injury Brittle bone disease Broken ankle/broken foot Broken arm Broken collarbone Broken leg Broken wrist/broken hand Bunions Carpal tunnel syndrome Cavovarus foot deformity Cavus foot Cerebral palsy Cervical myelopathy Cervical radiculopathy Charcot-Marie-Tooth disease Chondrosarcoma Chordoma Chronic regional multifocal osteomyelitis Clubfoot Congenital hand deformities Congenital myasthenic syndromes Congenital pseudoarthrosis Contractures Desmoid tumors Discoid meniscus Dislocated elbow Dislocated shoulder Dislocation Dislocation – hip Dislocation – knee Dupuytren's contracture Early-onset scoliosis Ehlers-Danlos syndrome Elbow fracture Elbow impingement Elbow instability Elbow loose body Eosinophilic granuloma Epiphyseal dysplasia Ewing sarcoma Extra finger/toes Failed total hip replacement Failed total knee replacement Femoral nonunion Fibrosarcoma Fibrous dysplasia Fibular hemimelia Flatfeet Foot deformities Foot injuries Ganglion cyst Genu valgum Genu varum Giant cell tumor Golfer's elbow Gorham’s disease Growth plate arrest Growth plate fractures Hammertoe and mallet toe Heel cord contracture -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Spinal Dysraphism an Orthopaedic Syndrome in Children Accompanying Occult Forms
Arch Dis Child: first published as 10.1136/adc.35.182.315 on 1 August 1960. Downloaded from SPINAL DYSRAPHISM AN ORTHOPAEDIC SYNDROME IN CHILDREN ACCOMPANYING OCCULT FORMS BY C. C. MICHAEL JAMES and L. P. LASSMAN From the Departments of Orthopaedic Surgery and Neurological Surgery, Newcastle General Hospital, Newcastle upon Tyne (RECEIVED FOR PUBLICATION OCTOBER 19, 1959) Much interest has been shown in the pathology which usually suffer. The treatment in the first of the more gross developmental anomalies of the place is principally in the field of neurosurgery since spinal cord and its coverings and in their clinical the removal of the primary cause, when it is possible, manifestations, most of which are not amenable to demands laminectomy and exploration around the treatment. It has not been appreciated that lesser spinal cord within the dura mater. Subsequent anomalies can also produce disabilities, that they orthopaedic care will be needed only to correct can be diagnosed in life and that they can frequently established deformity if the diagnosis has been be treated by surgery before the secondary effects made late. have become severe and irreversible. Clinical Spinal dysraphism is a term which has been experience over a number of years of the many applied to failure of complete development in the copyright. children sent to orthopaedic clinics with various midline of the dorsal aspect of the embryo. The types of foot or lower limb defect led us to suspect extent of this failure may be of mild, moderate or the presence in some children of a spinal cord severe degree. -

Peds Ortho: What Is Normal, What Is Not, and When to Refer
Peds Ortho: What is normal, what is not, and when to refer Future of Pedatrics June 10, 2015 Matthew E. Oetgen Benjamin D. Martin Division of Orthopaedic Surgery AGENDA • Definitions • Lower Extremity Deformity • Spinal Alignment • Back Pain LOWER EXTREMITY ALIGNMENT DEFINITIONS coxa = hip genu = knee cubitus = elbow pes = foot varus valgus “bow-legged” “knock-knee” apex away from midline apex toward midline normal varus hip (coxa vara) varus humerus valgus ankle valgus hip (coxa valga) Genu varum (bow-legged) Genu valgum (knock knee) bow legs and in toeing often together Normal Limb alignment NORMAL < 2 yo physiologic = reassurance, reevaluate @ 2 yo Bow legged 7° knock knee normal Knock knee physiologic = reassurance, reevaluate in future 4 yo abnormal 10 13 yo abnormal + pain 11 Follow-up is essential! 12 Intoeing 1. Femoral anteversion 2. Tibial torsion 3. Metatarsus adductus MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE! BRACES ARE HISTORY! Femoral Anteversion “W” sitters Internal rotation >> External rotation knee caps point in MOST LIKELY PHYSIOLOGIC AND MAY RESOLVE! Internal Tibial Torsion Thigh foot angle MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE BY SCHOOL AGE Foot is rotated inward Internal Tibial Torsion (Fuchs 1996) Metatarsus Adductus • Flexible = correctible • Observe vs. casting CURVED LATERAL BORDER toes point in NOT TO BE CONFUSED WITH… Clubfoot talipes equinovarus adductus internal varus rotation equinus CAN’T DORSIFLEX cavus Clubfoot START19 CASTING JUST AFTER BIRTH Calcaneovalgus Foot • Intrauterine positioning • Resolve -

International Symposium on New Developments in Neurofibromatoses and Rasopathies
INTERNATIONAL SYMPOSIUM ON NEW DEVELOPMENTS IN NEUROFIBROMATOSES AND RASOPATHIES Their Management, Diagnosis, Current and Future Therapeutic Targets 27th - 29th November 2017, Crowne Plaza, Kochi, Kerala, South India INTERNATIONAL SYMPOSIUM ON NEW DEVELOPMENTS IN NEUROFIBROMATOSES AND RASOPATHIES THE FIRST INTERNATIONAL SYMPOSIUM ON RASOPATHIES TO BE HELD IN ASIA RASopathies are a class of developmental disorders with overlapping clinical features as well as genetic mutations. RASopathies are associated with dysregulation of the RAS-MAPK (RAS/mitogen activated protein kinase) signalling pathway, an important pathway in humans as it is related to nine different genetic conditions and in many cancers. The meeting will bring together leading scientists, clinicians, researchers and trainee health care professionals in the field of genetics, cancer, neurology, paediatrics, cardiology, neurosurgery, craniofacial surgery, plastic surgery, dermatology, oncology and biomedical sciences from across the world. 200 25+ 20+ PLACES SPEAKERS TOPICS AIMS TO ENSURE THAT HEALTH PROFESSIONALS AND TO IDENTIFY THERAPEUTIC TARGETS FOR SCIENTISTS ARE KEPT ABREAST OF ANY NEW SEVERAL OF THESE RARE DISEASES DEVELOPMENTS IN CLINICAL PRACTICE TOPICS COVERED o RASopathies: Syndromes of Ras/ MAPK pathway o Cardio-Facio-Cutaneous Syndrome dysregulation o Capillary Malformation-Arteriovenous o Neurofibromatosis Type 1 Malformation Syndrome o Legius Syndrome o Natural history, improved diagnosis and genotype phenotype correlation for NF2 and o Noonan Syndrome Schwannomatosis -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

Flexible Flatfoot
REVIEW ORTHOPEDICS & TRAUMATOLOGY North Clin Istanbul 2014;1(1):57-64 doi: 10.14744/nci.2014.29292 Flexible flatfoot Aziz Atik1, Selahattin Ozyurek2 1Department of Orthopedics and Tarumatology, Balikesir University Faculty of Medicine, Balikesir, Turkey; 2Department of Orthopedics and Traumatology, Aksaz Military Hospital, Marmaris, Mugla, Turkey ABSTRACT While being one of the most frequent parental complained deformities, flatfoot does not have a universally ac- cepted description. The reasons of flexible flatfoot are still on debate, but they must be differentiated from rigid flatfoot which occurs secondary to other pathologies. These children are commonly brought up to a physician without any complaint. It should be kept in mind that the etiology may vary from general soft tissue laxities to intrinsic foot pathologies. Every flexible flatfoot does not require radiological examination or treatment if there is no complaint. Otherwise further investigation and conservative or surgical treatment may necessitate. Key words: Children; flatfoot; flexible; foot problem; pes planus. hough the term flatfoot (pes planus) is gener- forms again (Figure 2). When weight-bearing forces Tally defined as a condition which the longitu- on feet are relieved this arch can be observed. If the dinal arch of the foot collapses, it has not a clinically foot is not bearing any weight, still medial longitu- or radiologically accepted universal definition. Flat- dinal arch is not seen, then it is called rigid (fixed) foot which we frequently encounter in routine out- flatfoot. To differentiate between these two condi- patient practice will be more accurately seen as a re- tions easily, Jack’s test (great toe is dorisflexed as the sult of laxity of ligaments of the foot. -

Maternal Use of Opioids During Pregnancy and Congenital Malformations: a Systematic Review
Maternal Use of Opioids During Jennifer N. Lind, PharmD, MPH, a, b Julia D. Interrante, MPH, a, c Elizabeth C. Ailes, PhD, MPH, a Suzanne M. Gilboa, PhD, a PregnancySara Khan, MSPH, a, d, e Meghan T. Frey, and MA, MPH, a CongenitalApril L. Dawson, MPH, a Margaret A. Honein, PhD, MPH, a a a, b f, g a Malformations:Nicole F. Dowling, PhD, Hilda Razzaghi, PhD, MSPH, A Andreea Systematic A. Creanga, MD, PhD, Cheryl Review S. Broussard, PhD CONTEXT: abstract Opioid use and abuse have increased dramatically in recent years, particularly OBJECTIVES: among women. We conducted a systematic review to evaluate the association between prenatal DATA SOURCES: opioid use and congenital malformations. We searched Medline and Embase for studies published from 1946 to 2016 and STUDY SELECTION: reviewed reference lists to identify additional relevant studies. We included studies that were full-text journal articles and reported the results of original epidemiologic research on prenatal opioid exposure and congenital malformations. We assessed study eligibility in multiple phases using a standardized, DATA EXTRACTION: duplicate review process. Data on study characteristics, opioid exposure, timing of exposure during pregnancy, congenital malformations (collectively or as individual subtypes), length of RESULTS: follow-up, and main findings were extracted from eligible studies. Of the 68 studies that met our inclusion criteria, 46 had an unexposed comparison group; of those, 30 performed statistical tests to measure associations between maternal opioid use during pregnancy and congenital malformations. Seventeen of these (10 of 12 case-control and 7 of 18 cohort studies) documented statistically significant positive associations. Among the case-control studies, associations with oral clefts and ventricular septal defects/atrial septal defects were the most frequently reported specific malformations.