Local Report ~ January 2007
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -

Accident and Emergency: Performance Update
Accident and Emergency Performance update Prepared by Audit Scotland May 2014 Auditor General for Scotland The Auditor General’s role is to: • appoint auditors to Scotland’s central government and NHS bodies • examine how public bodies spend public money • help them to manage their finances to the highest standards • check whether they achieve value for money. The Auditor General is independent and reports to the Scottish Parliament on the performance of: • directorates of the Scottish Government • government agencies, eg the Scottish Prison Service, Historic Scotland • NHS bodies • further education colleges • Scottish Water • NDPBs and others, eg Scottish Police Authority, Scottish Fire and Rescue Service. You can find out more about the work of the Auditor General on our website: www.audit-scotland.gov.uk/about/ags Audit Scotland is a statutory body set up in April 2000 under the Public Finance and Accountability (Scotland) Act 2000. We help the Auditor General for Scotland and the Accounts Commission check that organisations spending public money use it properly, efficiently and effectively. Accident and Emergency | 3 Contents Summary 4 Key messages 7 Part 1. A&E waiting times 9 Part 2. Reasons for delays in A&E 20 Part 3. Action by the Scottish Government 37 Endnotes 41 Appendix 1. NHS Scotland A&E departments and minor injury units 43 Appendix 2. National context for A&E and unscheduled care, 2004 to 2014 45 Exhibit data When viewing this report online, you can access background data by clicking on the graph icon. The data file will -

4.11 Chief Executive and Directors Report
NHS Highland Board 24 July 2018 Item 4.11 CHIEF EXECUTIVE AND DIRECTORS REPORT – EMERGING ISSUES AND UPDATES Report by Elaine Mead, Chief Executive The Board is asked to: • Note the updates provided in the report. Chief Officer Argyll and Bute Health and Social Care Partnership It is with much regret to report that Christina West has resigned from the post of Chief Officer for Argyll and Bute Health and Social Care Partnership with a leaving date of 30th September 2018. Integration of health and social care has been one of the most significant changes in the public sector for decades. Under Christina’s Leadership she leaves Argyll and Bute’s Health and Social Care Partnership in a positive position to move forward, with plans in place to redesign services not least to meet the demographic challenges. Christina takes with her our grateful thanks, for her hard work, determination and commitment to developing health and social care services for the people of Argyll and Bute. She embraced the Highland Quality Approach and has been an invaluable member of NHS Highland’s Senior Leadership team. The recruitment process is underway to secure a new Chief Officer. Dr Grays Temporary Service Model for Women and Children’s services A new temporary service model for Women and Children’s services at Dr Gray’s Hospital is to be put in place to allow maternity and paediatric service to continue in Elgin. The change comes after NHS Education for Scotland said initial indications were that only two trainee doctors had elected to work at Dr Gray’s at the next intake in August – six less than the number required. -

Emergency Departments
ED Site List 220711 v2.xls NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care File NHS Board Site Type Location Name Location Address Comments Type Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG -

11 0 CHP Estate Condition Survey Ver 3 151107
Argyll and Bute CHP Committee 29 November 2007 Item: 11.0 ARGYLL AND BUTE CHP Estate Condition Survey 2007/08 Report by the Head of Planning, Contracting and Performance The CHP Committee is asked to: Note the findings of the estate condition survey conducted on its properties ‹ Note and endorse the action plan drawn up ‹ Note that the CHP Capital planning group has been remitted to performance manage and monitor progress against the action plan 1 INTRODUCTION Each NHS Board has to approve a 5-Year Capital Investment Programme and a key element within this is ensuring that the Boards estate is fit for purpose in terms of statutory compliance, function and effectiveness to inform its property strategy and requirements. The CHP commissioned consultants to undertake an Estate condition survey on all the NHS Board owned premises. This appraisal of condition and performance of the estate follows well established guidance described in NHS Estatecode. These appraisals are a high level assessment of condition and performance aimed at providing a baseline from which property strategies can be developed. This Estate condition report is based on a detailed survey of the property condition & the other facets listed below. Full technical details are retained within a property database, which will be regularly updated. Information is gathered from both physical surveys and historic information gathered & retained by Estate Officers. Copies of the Estate Condition Database are retained by the operational Estate Officers and additional detailed information which is summarised in the main reports can be extracted for each individual building or site owned by Argyll & Bute CHP. -

Emergency Departments
ED-site-list NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care NHS Board Site Type Location Name Location Address File Type Comments Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG A Forth Valley -

Aviemore and Broadford Preferred for New Hospitals
Highlights MONTHLY March 2014 MEET THE BOARD: GRAHAM CRERAR A fund of experience AVIEMORE AND BROADFORD Dr Boyd Peters at Ian Charles PREFERRED FOR Hospital in Grantown-on-Spey NEW HOSPITALS St Vincents Hospital, Kingussie BROADFORD and Aviemore community hospital and resource have emerged as the pre- centre in Aviemore, starting a ferred locations for new hos- wider redesign of health and so- pitals in Highland. cial care services and closing Ian On 11th March, the steering Charles Hospital in Grantown-on- group looking into the redesign of Spey and St Vincent Hospital in health and adult social care ser- Kingussie. vices in Skye, Lochalsh and Work will now take place to South West Ross chose Broad- identify possible sites in ford as its preferred location for a Aviemore for the new hospital and resource centre, and this will new hospital in the area. Mackinnon Memorial Hospital, form part of the formal consulta- A week earlier, a special meet- Broadford ing of the NHS Highland board tion. decided to go to formal three- In Skye, Lochalsh and South month consultation in Badenoch West Ross, an extensive engage- & Strathspey, where there has ment exercise resulted in a pre- already been extensive commu- ferred option being chosen for the nity engagement on service re- future shape of service provision. design. The result of this is the This was to modernise local ser- emergence of a preferred option vices, including those provided by for change – developing a new Continued on page 2 Portree Hospital - - Preferred locations for new hospitals Continued from front page of the NHS Highland board to at pains to point out at its special pave the way for a formal, three- meeting this month that much the area’s two hospitals, Portree month consultation on the full had still to be done before any and Mackinnon Memorial in service model and possible site construction work starts. -

Board Approves Safe Transition to Midwife-Led Unit
THE NHS HIGHLAND STAFF NEWSPAPER May 2017 HighNOVEMBERlights 2015 CAITHNESS MATERNITY Board approves safe transition to midwife-led unit NHS HIGHLAND board members unani- mously approved a report updating them on the safe transition to a midwife-led Commu- nity Maternity Unit (CMU) at Caithness Gen- eral Hospital. At the meeting on Tuesday 30th May 2017, Dr Roderick Harvey, the board’s medical director re- ported that, as planned, more expectant mothers were travelling to Inverness to give birth and that the changes have resulted in “very significantly lower” emergency maternal and neonatal transfers. The decision to reconfigure the maternity unit at CGH from a consultant-led obstetric unit was made on the grounds of safety in November 2016. The move was made after investigations found that the deaths of two babies born at the Caithness General were "potentially avoidable". Six months on from the decision, Dr Rod Harvey said: “The ‘very significantly lower’ maternal and The Medical High Dependency Unit (MHDU) at Raig- neonatal transfer figures are key indicators that the more Hospital in Inverness had something astonishing to CMU and new arrangements are working as celebrate this month. Turn to page 15 to find out more... Continued on page 2 - - Board approve CMU other by voice, speak regularly, and Continued from front feel comfortable discussing concerns planned.” and enjoying working with each Figures show that eleven women team. The experience and sharing of gave birth at Caithness General be- a wealth of expertise has obviously Contents tween December 2016 to the end of been of great benefit to the overall April – as opposed to 73 women development of the CMU. -

NHS Highland CONSULTANT ANAESTHETIST
NHS Highland CONSULTANT ANAESTHETIST Lorn & Islands Hospital VACANCY Consultant in Anaesthesia Lorn & Islands Hospital 40 hours per week £80,653 (GBP) to £107,170 (GBP) per annum Tenure: Permanent Applications are invited to join our Anaesthetics team at Lorn & Islands Hospital, Oban on the beautiful West Coast of Scotland. This vacancy is offered on the basis of 10 Programmed Activities per week. The department of Anaesthetics is based at Lorn & Islands Hospital, Oban. The Hospital is located on the southern outskirts of Oban and forms a hub for both acute and community services within the area. Purpose built in 1995, the Hospital houses a full range of facilities expected in a rural general hospital including a full 24 hour medical, surgical and anaesthetic service. Duties are based at Lorn and the Islands Hospital with some sessions at the Argyll and Bute Mental Health Hospital in Lochgilphead. There is the possibility of further clinic sessions at community hospitals throughout Argyll. The area is of one of outstanding natural beauty, the town of Oban is a tourist and commercial centre for the West of Scotland and the Isles. The port town has ferry links to the islands of Mull, Iona, Islay, Coll, Tiree, Colonsay and Lismore. There is plenty of opportunity for enjoying leisure pursuits including yachting, canoeing, walking, climbing, cycling and fishing. It’s a great place to bring up a family with good local schools and reasonable property prices. Oban provides the advantage of a high quality of life in a rural setting with access to the main centres of Glasgow, Stirling and Perth all within 2½ hours travel time. -

MND Scotland Integrated Care Pathway – Mobility
MND Scotland Integrated Care Pathway The Scottish MND Clinical Specialist Team Helen Lennox Dumfries & Galloway North, South & East Ayrshire Laura Cunningham Glasgow City (North, East, West) Cumbernauld North Lanarkshire (ML Postcodes) South Lanarkshire (ML Postcodes) Ann Silver Western Isles Glasgow City (South) North Lanarkshire (G Postcodes) South Lanarkshire (G Postcodes) Renfrewshire Janice Hatrick East Dunbartonshire West Dunbartonshire Inverclyde East Renfrewshire Renfrewshire Dianne Fraser Aberdeen City Susan Stewart Aberdeenshire Moray Moira Flett Orkney Dorothy Storey Shetland Andrew Bethell Highland Jacqui McMillan Argyll & Bute Carolyn Webber Dundee City Dee McAleer Angus Gill Craig Perth & Kinross North East Fife Gill Stott Edinburgh City Alison McEleney Borders East, West & Mid Lothian Laura Marshall Stirlingshire Falkirk Clackmannanshire Loch Lomond & Trossachs Dunfermline & West Fife Kirkcaldy & Levenmouth Glenrothes NATIONAL NURSING LEAD FOR MOTOR NEURONE DISEASE/ CONSULTANT NURSE Judith Newton, RGN MSc(R) University of Edinburgh, Centre of Clinical Brain Sciences, Chancellors Building, Little France, Edinburgh EH16 4SB Mobile: 07702858820 Email:[email protected] [email protected] MND CARE CENTRE - WEST MND CARE CENTRE – MND CARE CENTRE – TAYSIDE Helen Lennox ORKNEY Carolyn Webber Regional Care Specialist for MND Moira Flett Nurse Specialist - MND Room L2/70, 2nd Floor MND Care Advisor Department of Neurology Dept Neurosurgery, Institute of Balfour Hospital South Block Level 6 Neurological Sciences New Scapa -

Public Document Pack Argyll and Bute Council Comhairle Earra Ghaidheal Agus Bhoid
Public Document Pack Argyll and Bute Council Comhairle Earra Ghaidheal agus Bhoid Corporate Services Director: Nigel Stewart Kilmory, Lochgilphead, PA31 8RT Tel: 01546 602127 Fax: 01546 604444 DX 599700 LOCHGILPHEAD e.mail –[email protected] 16 June 2004 NOTICE OF MEETING A meeting of ARGYLL AND BUTE COUNCIL will be held in the COUNCIL CHAMBER, KILMORY, LOCHGILPHEAD on WEDNESDAY, 23 JUNE 2004 at 11:00 AM, which you are requested to attend. Nigel Stewart Director of Corporate Services BUSINESS 1. APOLOGIES FOR ABSENCE 2. DECLARATIONS OF INTEREST (IF ANY) 3. NHS ARGYLL AND CLYDE CLINICAL STRATEGY (a) PRESENTATION AND DISCUSSION OF CONSULTATION DOCUMENT (Pages 1 - 60) (b) NOTICE OF MOTION UNDER STANDING ORDER 13 By Councillor Macaskill, seconded by Councillor Walsh “That the Council appoint a short life Policy Development Group of five Members with at least one Member from each of the Council’s four sub- areas to formulate a draft response to the Consultation document after consultation with Area Committees and other stakeholders as appropriate – the draft response to come to the Council meeting on 15 September 2004.” (c) MATERNITY SERVICES Report by Director of Community Services (Pages 61 - 86) 4. MINUTES Argyll and Bute Council 12 May 2004 (Pages 87 - 92) 5. MINUTES OF COMMITTEES (a) Helensburgh and Lomond Area Committee 4 May 2004 (Pages 93 - 102) (b) Bute and Cowal Area Committee 4 May 2004 (Pages 103 - 106) (c) Mid Argyll, Kintyre and Islay Area Committee 5 May 2004 (Pages 107 - 112) (d) Oban, Lorn and the Isles Area -
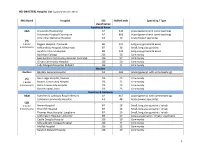
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St.