NGS Panels 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of Kallmann Syndrome, a Genetic Disorder of Neuronal Migration Affecting the Olfactory and Genital Systems
MR Imaging of Kallmann Syndrome, a Genetic Disorder of Neuronal Migration Affecting the Olfactory and Genital Systems 1 2 2 3 4 Charles L. Truwit, ' A. James Barkovich, Melvin M. Grumbach, and John J. Martini PURPOSE: We report the MR findings in nine patients with clinical and laboratory evidence of Kallmann syndrome (KS), a genetic disorder of olfactory and gonadal development. In patients with KS, cells that normally express luteinizing hormone-releasing hormone fail to migrate from the medial olfactory placode along the terminalis nerves into the forebrain. In addition, failed neuronal migration from the lateral olfactory placode along the olfactory fila to the forebrain results in aplasia or hypoplasia of the olfactory bulbs and tracts. Patients with KS, therefore, suffer both reproductive and olfactory dysfunction. METHODS: Nine patients with KS underwent direct coronal MR of their olfactory regions in order to assess the olfactory sulci, bulbs, and tracts. A lOth patient had MR findings of KS, although the diagnosis is not yet confirmed by laboratory tests. RESULTS: Abnormalities of the olfactory system were identified in all patients. In particular, the anterior portions of the olfactory sulci were uniformly hypoplastic. The olfactory bulbs and tracts appeared hypoplastic or aplastic in all patients in whom the bulb/ tract region was satisfactorily imaged. In two (possibly three) patients, prominent soft tissue in the region of the bulbs suggests radiographic evidence of neurons that have been arrested before migration. CONCLUSIONS: Previous investigators of patients with KS used axial MR images to demonstrate hypoplasia of the olfactory sulci but offered no assessment of the olfactory bulbs. -

Marble Bone Disease: a Rare Bone Disorder
Open Access Case Report DOI: 10.7759/cureus.339 Marble Bone Disease: A Rare Bone Disorder Eswaran Arumugam 1 , Maheswari Harinathbabu 2 , Ranjani Thillaigovindan 1 , Geetha Prabhu 1 1. Prosthodontics, Thai Moogambigai Dental College and Hospital 2. Oral Medicine and Radiology, Siva Multi Speciality Dental Clinic Corresponding author: Eswaran Arumugam, [email protected] Abstract Osteopetrosis, or marble bone disease, is a rare skeletal disorder due to a defective function of the osteoclasts. This defect renders bones more susceptible to osteomyelitis due to decreased vascularity. This disorder is inherited as autosomal dominant and autosomal recessive. Healthcare professionals should urge these patients to maintain their oral health as well as general health, as this condition makes these patients more susceptible to frequent infections and fractures. This case report emphasizes the signs and symptoms of marble bone disease and presents clinical and radiographic findings. Categories: Physical Medicine & Rehabilitation, Miscellaneous Keywords: osteopetrosis, marble bone disease, autosomal recessive, dense sclerotic bone Introduction Osteopetrosis (literally "stone bone," also known as marble bone disease or Albers-Schonberg disease) is an extremely rare inherited disorder where the bones harden and become denser. The disorder can cause osteosclerosis. The estimated prevalence of osteopetrosis is 1 in 100,000 to 500,000. It presents in two major clinical forms-a benign autosomal dominant form and a malignant autosomal recessive form. The autosomal dominant adult (benign) form is associated with few, if any, symptoms, and the autosomal recessive infantile (malignant) form is typically fatal during infancy or early childhood if untreated [1]. A rarer autosomal recessive (intermediate) form presents during childhood with some signs and symptoms of malignant osteopetrosis. -
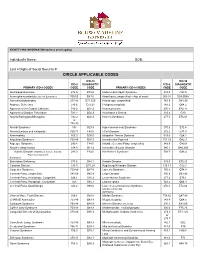
Circle Applicable Codes
IDENTIFYING INFORMATION (please print legibly) Individual’s Name: DOB: Last 4 Digits of Social Security #: CIRCLE APPLICABLE CODES ICD-10 ICD-10 ICD-9 DIAGNOSTIC ICD-9 DIAGNOSTIC PRIMARY ICD-9 CODES CODE CODE PRIMARY ICD-9 CODES CODE CODE Abetalipoproteinemia 272.5 E78.6 Hallervorden-Spatz Syndrome 333.0 G23.0 Acrocephalosyndactyly (Apert’s Syndrome) 755.55 Q87.0 Head Injury, unspecified – Age of onset: 959.01 S09.90XA Adrenaleukodystrophy 277.86 E71.529 Hemiplegia, unspecified 342.9 G81.90 Arginase Deficiency 270.6 E72.21 Holoprosencephaly 742.2 Q04.2 Agenesis of the Corpus Callosum 742.2 Q04.3 Homocystinuria 270.4 E72.11 Agenesis of Septum Pellucidum 742.2 Q04.3 Huntington’s Chorea 333.4 G10 Argyria/Pachygyria/Microgyria 742.2 Q04.3 Hurler’s Syndrome 277.5 E76.01 or 758.33 Aicardi Syndrome 333 G23.8 Hyperammonemia Syndrome 270.6 E72.4 Alcohol Embryo and Fetopathy 760.71 F84.5 I-Cell Disease 272.2 E77.0 Anencephaly 655.0 Q00.0 Idiopathic Torsion Dystonia 333.6 G24.1 Angelman Syndrome 759.89 Q93.5 Incontinentia Pigmenti 757.33 Q82.3 Asperger Syndrome 299.8 F84.5 Infantile Cerebral Palsy, unspecified 343.9 G80.9 Ataxia-Telangiectasia 334.8 G11.3 Intractable Seizure Disorder 345.1 G40.309 Autistic Disorder (Childhood Autism, Infantile 299.0 F84.0 Klinefelter’s Syndrome 758.7 Q98.4 Psychosis, Kanner’s Syndrome) Biotinidase Deficiency 277.6 D84.1 Krabbe Disease 333.0 E75.23 Canavan Disease 330.0 E75.29 Kugelberg-Welander Disease 335.11 G12.1 Carpenter Syndrome 759.89 Q87.0 Larsen’s Syndrome 755.8 Q74.8 Cerebral Palsy, unspecified 343.69 G80.9 -
Restoration of Epithelial Sodium Channel Function by Synthetic Peptides in Pseudohypoaldosteronism Type 1B Mutants
ORIGINAL RESEARCH published: 24 February 2017 doi: 10.3389/fphar.2017.00085 Restoration of Epithelial Sodium Channel Function by Synthetic Peptides in Pseudohypoaldosteronism Type 1B Mutants Anita Willam 1*, Mohammed Aufy 1, Susan Tzotzos 2, Heinrich Evanzin 1, Sabine Chytracek 1, Sabrina Geppert 1, Bernhard Fischer 2, Hendrik Fischer 2, Helmut Pietschmann 2, Istvan Czikora 3, Rudolf Lucas 3, Rosa Lemmens-Gruber 1 and Waheed Shabbir 1, 2 1 Department of Pharmacology and Toxicology, University of Vienna, Vienna, Austria, 2 APEPTICO GmbH, Vienna, Austria, 3 Vascular Biology Center, Medical College of Georgia, Augusta University, Augusta, GA, USA Edited by: The synthetically produced cyclic peptides solnatide (a.k.a. TIP or AP301) and its Gildas Loussouarn, congener AP318, whose molecular structures mimic the lectin-like domain of human University of Nantes, France tumor necrosis factor (TNF), have been shown to activate the epithelial sodium Reviewed by: channel (ENaC) in various cell- and animal-based studies. Loss-of-ENaC-function Stephan Kellenberger, University of Lausanne, Switzerland leads to a rare, life-threatening, salt-wasting syndrome, pseudohypoaldosteronism type Yoshinori Marunaka, 1B (PHA1B), which presents with failure to thrive, dehydration, low blood pressure, Kyoto Prefectural University of Medicine, Japan anorexia and vomiting; hyperkalemia, hyponatremia and metabolic acidosis suggest *Correspondence: hypoaldosteronism, but plasma aldosterone and renin activity are high. The aim of Anita Willam the present study was to investigate whether the ENaC-activating effect of solnatide [email protected] and AP318 could rescue loss-of-function phenotype of ENaC carrying mutations at + Specialty section: conserved amino acid positions observed to cause PHA1B. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Loss-Of-Function Mutation in the Prokineticin 2 Gene Causes
Loss-of-function mutation in the prokineticin 2 gene SEE COMMENTARY causes Kallmann syndrome and normosmic idiopathic hypogonadotropic hypogonadism Nelly Pitteloud*†, Chengkang Zhang‡, Duarte Pignatelli§, Jia-Da Li‡, Taneli Raivio*, Lindsay W. Cole*, Lacey Plummer*, Elka E. Jacobson-Dickman*, Pamela L. Mellon¶, Qun-Yong Zhou‡, and William F. Crowley, Jr.* *Reproductive Endocrine Unit, Department of Medicine and Harvard Reproductive Endocrine Science Centers, Massachusetts General Hospital, Boston, MA 02114; ‡Department of Pharmacology, University of California, Irvine, CA 92697; §Department of Endocrinology, Laboratory of Cellular and Molecular Biology, Institute of Molecular Pathology and Immunology, University of Porto, San Joa˜o Hospital, 4200-465 Porto, Portugal; and ¶Departments of Reproductive Medicine and Neurosciences, University of California at San Diego, La Jolla, CA 92093 Communicated by Patricia K. Donahoe, Massachusetts General Hospital, Boston, MA, August 14, 2007 (received for review May 8, 2007) Gonadotropin-releasing hormone (GnRH) deficiency in the human associated with KS, although no functional data on the mutant presents either as normosmic idiopathic hypogonadotropic hypo- proteins were provided (17). Herein, we demonstrate that homozy- gonadism (nIHH) or with anosmia [Kallmann syndrome (KS)]. To gous loss-of-function mutations in the PROK2 gene cause IHH in date, several loci have been identified to cause these disorders, but mice and humans. only 30% of cases exhibit mutations in known genes. Recently, murine studies have demonstrated a critical role of the prokineticin Results pathway in olfactory bulb morphogenesis and GnRH secretion. Molecular Analysis of PROK2 Gene. A homozygous single base pair Therefore, we hypothesize that mutations in prokineticin 2 deletion in exon 2 of the PROK2 gene (c.[163delA]ϩ [163delA]) (PROK2) underlie some cases of KS in humans and that animals was identified in the proband, in his brother with KS, and in his deficient in Prok2 would be hypogonadotropic. -

Kallmann Syndrome
Kallmann syndrome Author: DoctorJean-Pierre Hardelin1 Creation date: July 1997 Updates: May 2002 December 2003 February 2005 Scientific editor: Professor Philippe Bouchard 1 Unité de Génétique des Déficits Sensoriels (INSERM U587), Institut Pasteur, 25 rue du Dr Roux, 75724 Paris cedex 15, France. [email protected] Abstract Keywords Disease name and synonyms Excluded diseases Diagnostic criteria / Definition Differential diagnosis Incidence Clinical description Management including treatment Etiology Diagnostic methods Genetic counseling Prenatal diagnosis Unresolved questions and comments References Abstract Kallmann syndrome combines hypogonadotropic hypogonadism due to GnRH deficiency, with anosmia or hyposmia. Magnetic resonance imaging (MRI) shows hypoplasia or aplasia of the olfactory bulbs. The incidence is estimated at 1 case in 10,000 males and 1 case in 50,000 females. The main clinical features consist of the association of micropenis and cryptorchidism in young boys, the absence of spontaneous puberty, a partial or total loss of the sense of smell (anosmia). Other possible signs include mirror movements of the upper limbs (synkinesis), unilateral or bilateral renal aplasia, cleft lip/palate, dental agenesis, arched feet, deafness. Diagnostic methods consist of hormones evaluation (GnRH stimulation test) as well as qualitative and quantitative olfactometric evaluation. Hormonal replacement is used to induce puberty, and later, fertility. Kallmann syndrome is due to an impaired embryonic development of the olfactory system and the GnRH-synthesizing neurons. Sporadic cases have been predominantly reported. Three modes of inheritance have been described in familial forms: X-linked recessive, autosomal dominant, or more rarely autosomal recessive. To date, only two of the genes responsible for this genetically heterogeneous disease have been identified: KAL-1, responsible for the X-linked form and FGFR1, involved in the autosomal dominant form (KAL-2). -

Inherited Renal Tubulopathies—Challenges and Controversies
G C A T T A C G G C A T genes Review Inherited Renal Tubulopathies—Challenges and Controversies Daniela Iancu 1,* and Emma Ashton 2 1 UCL-Centre for Nephrology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF, UK 2 Rare & Inherited Disease Laboratory, London North Genomic Laboratory Hub, Great Ormond Street Hospital for Children National Health Service Foundation Trust, Levels 4-6 Barclay House 37, Queen Square, London WC1N 3BH, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-2381204172; Fax: +44-020-74726476 Received: 11 February 2020; Accepted: 29 February 2020; Published: 5 March 2020 Abstract: Electrolyte homeostasis is maintained by the kidney through a complex transport function mostly performed by specialized proteins distributed along the renal tubules. Pathogenic variants in the genes encoding these proteins impair this function and have consequences on the whole organism. Establishing a genetic diagnosis in patients with renal tubular dysfunction is a challenging task given the genetic and phenotypic heterogeneity, functional characteristics of the genes involved and the number of yet unknown causes. Part of these difficulties can be overcome by gathering large patient cohorts and applying high-throughput sequencing techniques combined with experimental work to prove functional impact. This approach has led to the identification of a number of genes but also generated controversies about proper interpretation of variants. In this article, we will highlight these challenges and controversies. Keywords: inherited tubulopathies; next generation sequencing; genetic heterogeneity; variant classification. 1. Introduction Mutations in genes that encode transporter proteins in the renal tubule alter kidney capacity to maintain homeostasis and cause diseases recognized under the generic name of inherited tubulopathies. -

Gonadotropin-Releasing Hormone Agonist Treatment of Girls with Constitutional Short Stature and Normal Pubertal Development
0021-972X/96/$03.00/0 Vol. 81, No. 9 Journal of Clmcal Endocrinology and Metabolism Printed in U.S.A. Copyright 0 1996 by The Endocrine Society Gonadotropin-Releasing Hormone Agonist Treatment of Girls with Constitutional Short Stature and Normal Pubertal Development JEAN-CLAUDE CAREL, FRlkDliRIQUE HAY, RliGIS COUTANT, DANIlkLE RODRIGUE, AND JEAN-LOUIS CHAUSSAIN Downloaded from https://academic.oup.com/jcem/article/81/9/3318/2651102 by guest on 23 September 2021 INSERM U-342 and Department of Pediatric Endocrinology, University of Paris V, Hbpital Saint Vincent de Paul, Paris, France ABSTRACT interruption of treatment, bone age was 14.9 2 1.3 yr (~13.5 yr in all GnRH agonists have been proposed to improve final height in patients), height was 149.1 k 4 cm, and final height prognosis was patients with constitutional short stature. We treated 31 girls, aged 150.6 2 3.6 cm. Final height prognosis was 1 2 2.3 cm greater than 11.9 i 1 yr (mean t- SD), with short stature, recent pubertal onset and pretreatment height prognosis (P < 0.02) and 1.2 k 2.2 cm below the predicted final height of 155 cm or less with depot triptorelin. During height predicted at the end of the treatment (P < 0.01). No major the 23 2 4 months of treatment, bone age progression was 0.6 ? 0.3 side-effect was observed. Height SD score decreased during treatment bone age yr/yr, and growth velocity declined from 7 k 2 to 4 2 0.8 with GnRH agonist from -2.3 ? 0.9 to -2.7 -C 0.7 SD score (P < cm/yr (P < 0.0001). -

Cardiomyopathy Precision Panel Overview Indications
Cardiomyopathy Precision Panel Overview Cardiomyopathies are a group of conditions with a strong genetic background that structurally hinder the heart to pump out blood to the rest of the body due to weakness in the heart muscles. These diseases affect individuals of all ages and can lead to heart failure and sudden cardiac death. If there is a family history of cardiomyopathy it is strongly recommended to undergo genetic testing to be aware of the family risk, personal risk, and treatment options. Most types of cardiomyopathies are inherited in a dominant manner, which means that one altered copy of the gene is enough for the disease to present in an individual. The symptoms of cardiomyopathy are variable, and these diseases can present in different ways. There are 5 types of cardiomyopathies, the most common being hypertrophic cardiomyopathy: 1. Hypertrophic cardiomyopathy (HCM) 2. Dilated cardiomyopathy (DCM) 3. Restrictive cardiomyopathy (RCM) 4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) 5. Isolated Left Ventricular Non-Compaction Cardiomyopathy (LVNC). The Igenomix Cardiomyopathy Precision Panel serves as a diagnostic and tool ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes. Indications The Igenomix Cardiomyopathy Precision Panel is indicated in those cases where there is a clinical suspicion of cardiomyopathy with or without the following manifestations: - Shortness of breath - Fatigue - Arrythmia (abnormal heart rhythm) - Family history of arrhythmia - Abnormal scans - Ventricular tachycardia - Ventricular fibrillation - Chest Pain - Dizziness - Sudden cardiac death in the family 1 Clinical Utility The clinical utility of this panel is: - The genetic and molecular diagnosis for an accurate clinical diagnosis of a patient with personal or family history of cardiomyopathy, channelopathy or sudden cardiac death. -

SKELETAL DYSPLASIA Dr Vasu Pai
SKELETAL DYSPLASIA Dr Vasu Pai Skeletal dysplasia are the result of a defective growth and development of the skeleton. Dysplastic conditions are suspected on the basis of abnormal stature, disproportion, dysmorphism, or deformity. Diagnosis requires Simple measurement of height and calculation of proportionality [<60 inches: consideration of dysplasia is appropriate] Dysmorphic features of the face, hands, feet or deformity A complete physical examination Radiographs: Extremities and spine, skull, Pelvis, Hand Genetics: the risk of the recurrence of the condition in the family; Family evaluation. Dwarf: Proportional: constitutional or endocrine or malnutrition Disproportion [Trunk: Extremity] a. Height < 42” Diastrophic Dwarfism < 48” Achondroplasia 52” Hypochondroplasia b. Trunk-extremity ratio May have a normal trunk and short limbs (achondroplasia), Short trunk and limbs of normal length (e.g., spondylo-epiphyseal dysplasia tarda) Long trunk and long limbs (e.g., Marfan’s syndrome). c. Limb-segment ratio Normal: Radius-Humerus ratio 75% Tibia-Femur 82% Rhizomelia [short proximal segments as in Achondroplastics] Mesomelia: Dynschondrosteosis] Acromelia [short hands and feet] RUBIN CLASSIFICATION 1. Hypoplastic epiphysis ACHONDROPLASTIC Autosomal Dominant: 80%; 0.5-1.5/10000 births Most common disproportionate dwarfism. Prenatal diagnosis: 18 weeks by measuring femoral and humeral lengths. Abnormal endochondral bone formation: zone of hypertrophy. Gene defect FGFR fibroblast growth factor receptor 3 . chromosome 4 Rhizomelic pattern, with the humerus and femur affected more than the distal extremities; Facies: Frontal bossing; Macrocephaly; Saddle nose Maxillary hypoplasia, Mandibular prognathism Spine: Lumbar lordosis and Thoracolumbar kyphosis Progressive genu varum and coxa valga Wedge shaped gaps between 3rd and 4th fingers (trident hands) Trident hand 50%, joint laxity Pathology Lack of columnation Bony plate from lack of growth Disorganized metaphysis Orthopaedics 1. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct.