Insurance and Advance Pay Test Requisition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CADASIL Testing
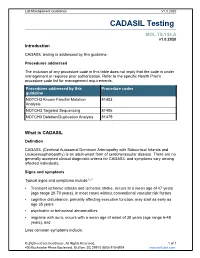
Lab Management Guidelines V1.0.2020 CADASIL Testing MOL.TS.144.A v1.0.2020 Introduction CADASIL testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline NOTCH3 Known Familial Mutation 81403 Analysis NOTCH3 Targeted Sequencing 81406 NOTCH3 Deletion/Duplication Analysis 81479 What is CADASIL Definition CADASIL (Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy) is an adult-onset form of cerebrovascular disease. There are no generally accepted clinical diagnostic criteria for CADASIL and symptoms vary among affected individuals. Signs and symptoms Typical signs and symptoms include1,2,3 Transient ischemic attacks and ischemic stroke, occurs at a mean age of 47 years (age range 20-70 years), in most cases without conventional vascular risk factors cognitive disturbance, primarily affecting executive function, may start as early as age 35 years psychiatric or behavioral abnormalities migraine with aura, occurs with a mean age of onset of 30 years (age range 6-48 years), and Less common symptoms include: © 2020 eviCore healthcare. All Rights Reserved. 1 of 7 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 recurrent seizures with onset in middle age, usually secondary to stroke acute encephalopathy, with a mean age of onset of 42 years Life expectancy for men with CADASIL is reduced by approximately five years and for women by 1 to 2 years.4 Diagnosis Brain Magnetic Resonance Imaging (MRI) findings include T2-signal-abnormalities in the white matter of the temporal pole and T2-signal-abnormalities in the external capsule and corpus callosum.1,2 CADASIL is suspected in an individual with the clinical signs and MRI findings. -

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

Genetic Mutations and Mechanisms in Dilated Cardiomyopathy
Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, … , Jessica R. Golbus, Megan J. Puckelwartz J Clin Invest. 2013;123(1):19-26. https://doi.org/10.1172/JCI62862. Review Series Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of congestive heart failure. In hypertrophic cardiomyopathy (HCM), cardiac output is limited by the thickened myocardium through impaired filling and outflow. Mutations in the genes encoding the thick filament components myosin heavy chain and myosin binding protein C (MYH7 and MYBPC3) together explain 75% of inherited HCMs, leading to the observation that HCM is a disease of the sarcomere. Many mutations are “private” or rare variants, often unique to families. In contrast, dilated cardiomyopathy (DCM) is far more genetically heterogeneous, with mutations in genes encoding cytoskeletal, nucleoskeletal, mitochondrial, and calcium-handling proteins. DCM is characterized by enlarged ventricular dimensions and impaired systolic and diastolic function. Private mutations account for most DCMs, with few hotspots or recurring mutations. More than 50 single genes are linked to inherited DCM, including many genes that also link to HCM. Relatively few clinical clues guide the diagnosis of inherited DCM, but emerging evidence supports the use of genetic testing to identify those patients at risk for faster disease progression, congestive heart failure, and arrhythmia. Find the latest version: https://jci.me/62862/pdf Review series Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, Jessica R. Golbus, and Megan J. Puckelwartz Department of Human Genetics, University of Chicago, Chicago, Illinois, USA. Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of conges- tive heart failure. -

Inherited Neuropathies
407 Inherited Neuropathies Vera Fridman, MD1 M. M. Reilly, MD, FRCP, FRCPI2 1 Department of Neurology, Neuromuscular Diagnostic Center, Address for correspondence Vera Fridman, MD, Neuromuscular Massachusetts General Hospital, Boston, Massachusetts Diagnostic Center, Massachusetts General Hospital, Boston, 2 MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology Massachusetts, 165 Cambridge St. Boston, MA 02114 and The National Hospital for Neurology and Neurosurgery, Queen (e-mail: [email protected]). Square, London, United Kingdom Semin Neurol 2015;35:407–423. Abstract Hereditary neuropathies (HNs) are among the most common inherited neurologic Keywords disorders and are diverse both clinically and genetically. Recent genetic advances have ► hereditary contributed to a rapid expansion of identifiable causes of HN and have broadened the neuropathy phenotypic spectrum associated with many of the causative mutations. The underlying ► Charcot-Marie-Tooth molecular pathways of disease have also been better delineated, leading to the promise disease for potential treatments. This chapter reviews the clinical and biological aspects of the ► hereditary sensory common causes of HN and addresses the challenges of approaching the diagnostic and motor workup of these conditions in a rapidly evolving genetic landscape. neuropathy ► hereditary sensory and autonomic neuropathy Hereditary neuropathies (HN) are among the most common Select forms of HN also involve cranial nerves and respiratory inherited neurologic diseases, with a prevalence of 1 in 2,500 function. Nevertheless, in the majority of patients with HN individuals.1,2 They encompass a clinically heterogeneous set there is no shortening of life expectancy. of disorders and vary greatly in severity, spanning a spectrum Historically, hereditary neuropathies have been classified from mildly symptomatic forms to those resulting in severe based on the primary site of nerve pathology (myelin vs. -

343747488.Pdf
Washington University School of Medicine Digital Commons@Becker Open Access Publications 6-1-2020 Systematic validation of variants of unknown significance in APP, PSEN1 and PSEN2 Simon Hsu Anna A Pimenova Kimberly Hayes Juan A Villa Matthew J Rosene See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Authors Simon Hsu, Anna A Pimenova, Kimberly Hayes, Juan A Villa, Matthew J Rosene, Madhavi Jere, Alison M Goate, and Celeste M Karch Neurobiology of Disease 139 (2020) 104817 Contents lists available at ScienceDirect Neurobiology of Disease journal homepage: www.elsevier.com/locate/ynbdi Systematic validation of variants of unknown significance in APP, PSEN1 T and PSEN2 Simon Hsua, Anna A. Pimenovab, Kimberly Hayesa, Juan A. Villaa, Matthew J. Rosenea, ⁎ Madhavi Jerea, Alison M. Goateb, Celeste M. Karcha, a Department of Psychiatry, Washington University School of Medicine, 425 S Euclid Avenue, St Louis, MO 63110, USA b Department of Neuroscience, Mount Sinai School of Medicine, New York, NY, USA ARTICLE INFO ABSTRACT Keywords: Alzheimer's disease (AD) is a neurodegenerative disease that is clinically characterized by progressive cognitive APP decline. More than 200 pathogenic mutations have been identified in amyloid-β precursor protein (APP), presenilin PSEN1 1 (PSEN1) and presenilin 2 (PSEN2). Additionally, common and rare variants occur within APP, PSEN1, and PSEN2 PSEN2 that may be risk factors, protective factors, or benign, non-pathogenic polymorphisms. Yet, to date, no Alzheimer's disease single study has carefully examined the effect of all of the variants of unknown significance reported in APP, Cell-based assays PSEN1 and PSEN2 on Aβ isoform levels in vitro. -

Experiences of Rare Diseases: an Insight from Patients and Families
Experiences of Rare Diseases: An Insight from Patients and Families Unit 4D, Leroy House 436 Essex Road London N1 3QP tel: 02077043141 fax: 02073591447 [email protected] www.raredisease.org.uk By Lauren Limb, Stephen Nutt and Alev Sen - December 2010 Web and press design www.raredisease.org.uk WordsAndPeople.com About Rare Disease UK Rare Disease UK (RDUK) is the national alliance for people with rare diseases and all who support them. Our membership is open to all and includes patient organisations, clinicians, researchers, academics, industry and individuals with an interest in rare diseases. RDUK was established by Genetic RDUK is campaigning for a Alliance UK, the national charity strategy for integrated service of over 130 patient organisations delivery for rare diseases. This supporting all those affected by would coordinate: genetic conditions, in conjunction with other key stakeholders | Research in November 2008 following the European Commission’s | Prevention and diagnosis Communication on Rare Diseases: | Treatment and care Europe’s Challenges. | Information Subsequently RDUK successfully | Commissioning and planning campaigned for the adoption of the Council of the European into one cohesive strategy for all Union’s Recommendation on patients affected by rare disease in an action in the field of rare the UK. As well as securing better diseases. The Recommendation outcomes for patients, a strategy was adopted unanimously by each would enable the most effective Member State of the EU (including use of NHS resources. the -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Cadasil Pathogenesis, Clinical and Radiological Findings and Treatment
View and review Arq Neuropsiquiatr 2010;68(2):287-299 Cadasil Pathogenesis, clinical and radiological findings and treatment Charles André ABSTRACT Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is the most common genetic cause of ischemic strokes and a most important model for the study of subcortical vascular dementia. This unrelentlessly progressive disease affects many hundreds of families all over the world but is not well studied in Brazil. This manuscript reviews pathogenetic, clinical, radiological and therapeutic features of CADASIL. The causal mutations are now very well known, but the same can not be said about its intimate pathogenetic mechanisms. The variable clinical presentation should lead physicians to actively pursue the diagnosis in many settings and to more thouroughly investigate family history in first degree relatives. A rational approach to genetic testing is however needed. Treatment of CADASIL is still largely empiric. High- quality therapeutic studies involving medications and cognitive interventions are strongly needed in CADASIL. Key words: CADASIL, etiology, genetics, diagnosis, therapeutics. CADASIL: patogênese, achados clínicos e radiológicos e tratamento RESUMO CADASIL é a causa genética mais freqüente de infartos cerebrais e constitui modelo importante de estudo de demências vasculares subcorticais. De natureza inexoravelmente progressiva, afeta milhares de pessoas em todo o mundo. Sua importância é pouco reconhecida entre nós, o que nos levou à presente revisão dos principais aspectos patogenéticos, clínicos, neuroradiológicos e terapêuticos da doença. As mutações causais são hoje bem conhecidas, mas os mecanismos patogenéticos íntimos ainda permanecem misteriosos. A apresentação clínica variável deve fazer com que os médicos considerem o diagnóstico em vários contextos clínicos e investiguem de forma mais extensa que o usual a história familial deparentes de primeiro grau. -

Genetic Testing for Familial Alzheimer's Disease
Corporate Medical Policy Genetic Testing for Familial Alzheimer’s Disease AHS – M2038 File Name: genetic_testing_for_familial_alzheimers_disease Origination: 1/2019 Last CAP Review: 10/2020 Next CAP Review: 10/2021 Last Review: 10/2020 Description of Procedure or Service Alzheimer disease (AD) is a neurodegenerative disease defined by a gradual decline in memory, cognitive functions, gross atrophy of the brain, and an accumulation of extracellular amyloid plaques and intracellular neurofibrillary tangles (Karch, Cruchaga, & Goate, 2014). Familial Alzheimer disease (FAD) is a rare, inherited form of AD. FAD has a much earlier onset than other forms of Alzheimer disease with symptoms developing in individuals in their thirties or forties. Related Policies General Genetic Testing, Germline Disorders AHS – M2145 General Genetic Testing, Somatic Disorders AHS – M2146 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for genetic testing for familial Alzheimer disease when it is determined the medical criteria or reimbursement guidelines below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. -

Clinical Vignette Novel Bi-Allelic Variants in GJC2 Associated
Clinical Vignette Novel Bi-allelic Variants in GJC2 Associated Pelizaeus- Merzbacher-like Disease 1: Clinical Clues and Differential Diagnosis Veronica Arora, Sapna Sandal, Ishwar Verma Institute of Medical Genetics and Genomics, Sir Ganga Ram Hospital, New Delhi Correspondence to: Dr Ishwar C Verma Email: [email protected] Abstract the environment and did not follow objects. Head titubation was present. There was no facial dys- Hypomyelinating Leukodystrophy-2 (HLD2) or morphism. Anthropometric measurements were Pelizaeus-Merzbacher-like disease 1 (PMLD1) is a as follows: length 82cm (+1.2SD), weight 10.6Kg slowly progressive leukodystrophy characterized (+1.1SD) and head circumference 47.7cm (+1.2SD). by nystagmus, hypotonia, and developmental Central nervous system examination showed bilat- delay. It is a close differential diagnosis for eral pendular nystagmus, axial hypotonia, dystonic Pelizaeus- Merzbacher disease (PMD) and should posturing, and choreo-athetoid movements (Figure be suspected in patients with features of PMD but 1). Deep tendon reflexes were brisk with extensor who are negative on testing for duplication of the plantar responses. The rest of the systemic PLP1 gene. We describe a case of a 16-month-old examination was non-contributory. MRI of the boy with a novel homozygous mutation in the GJC2 brain (axial view) showed diffuse hypo-myelination gene resulting in hypomyelinating leukodystrophy- in the peri-ventricular and sub-cortical area and 2. The clinical clues as well as features of other cerebellar white matter changes (Figure 2). disorders presenting similarly are discussed. Given the presence of hypotonia, brisk reflexes, nystagmus and hypomyelination on MRI, a deletion Clinical description duplication analysis for the PLP1 gene was done which was negative. -

Primate Specific Retrotransposons, Svas, in the Evolution of Networks That Alter Brain Function
Title: Primate specific retrotransposons, SVAs, in the evolution of networks that alter brain function. Olga Vasieva1*, Sultan Cetiner1, Abigail Savage2, Gerald G. Schumann3, Vivien J Bubb2, John P Quinn2*, 1 Institute of Integrative Biology, University of Liverpool, Liverpool, L69 7ZB, U.K 2 Department of Molecular and Clinical Pharmacology, Institute of Translational Medicine, The University of Liverpool, Liverpool L69 3BX, UK 3 Division of Medical Biotechnology, Paul-Ehrlich-Institut, Langen, D-63225 Germany *. Corresponding author Olga Vasieva: Institute of Integrative Biology, Department of Comparative genomics, University of Liverpool, Liverpool, L69 7ZB, [email protected] ; Tel: (+44) 151 795 4456; FAX:(+44) 151 795 4406 John Quinn: Department of Molecular and Clinical Pharmacology, Institute of Translational Medicine, The University of Liverpool, Liverpool L69 3BX, UK, [email protected]; Tel: (+44) 151 794 5498. Key words: SVA, trans-mobilisation, behaviour, brain, evolution, psychiatric disorders 1 Abstract The hominid-specific non-LTR retrotransposon termed SINE–VNTR–Alu (SVA) is the youngest of the transposable elements in the human genome. The propagation of the most ancient SVA type A took place about 13.5 Myrs ago, and the youngest SVA types appeared in the human genome after the chimpanzee divergence. Functional enrichment analysis of genes associated with SVA insertions demonstrated their strong link to multiple ontological categories attributed to brain function and the disorders. SVA types that expanded their presence in the human genome at different stages of hominoid life history were also associated with progressively evolving behavioural features that indicated a potential impact of SVA propagation on a cognitive ability of a modern human. -

Restoration of Epithelial Sodium Channel Function by Synthetic Peptides in Pseudohypoaldosteronism Type 1B Mutants
ORIGINAL RESEARCH published: 24 February 2017 doi: 10.3389/fphar.2017.00085 Restoration of Epithelial Sodium Channel Function by Synthetic Peptides in Pseudohypoaldosteronism Type 1B Mutants Anita Willam 1*, Mohammed Aufy 1, Susan Tzotzos 2, Heinrich Evanzin 1, Sabine Chytracek 1, Sabrina Geppert 1, Bernhard Fischer 2, Hendrik Fischer 2, Helmut Pietschmann 2, Istvan Czikora 3, Rudolf Lucas 3, Rosa Lemmens-Gruber 1 and Waheed Shabbir 1, 2 1 Department of Pharmacology and Toxicology, University of Vienna, Vienna, Austria, 2 APEPTICO GmbH, Vienna, Austria, 3 Vascular Biology Center, Medical College of Georgia, Augusta University, Augusta, GA, USA Edited by: The synthetically produced cyclic peptides solnatide (a.k.a. TIP or AP301) and its Gildas Loussouarn, congener AP318, whose molecular structures mimic the lectin-like domain of human University of Nantes, France tumor necrosis factor (TNF), have been shown to activate the epithelial sodium Reviewed by: channel (ENaC) in various cell- and animal-based studies. Loss-of-ENaC-function Stephan Kellenberger, University of Lausanne, Switzerland leads to a rare, life-threatening, salt-wasting syndrome, pseudohypoaldosteronism type Yoshinori Marunaka, 1B (PHA1B), which presents with failure to thrive, dehydration, low blood pressure, Kyoto Prefectural University of Medicine, Japan anorexia and vomiting; hyperkalemia, hyponatremia and metabolic acidosis suggest *Correspondence: hypoaldosteronism, but plasma aldosterone and renin activity are high. The aim of Anita Willam the present study was to investigate whether the ENaC-activating effect of solnatide [email protected] and AP318 could rescue loss-of-function phenotype of ENaC carrying mutations at + Specialty section: conserved amino acid positions observed to cause PHA1B.