81993354.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Increased Nuchal Translucency Precision Panel
Increased Nuchal Translucency Precision Panel Overview Increased Nuchal Translucency (NT) is defined as an abnormal accumulation of fluid in the nuchal area, which is visualized as a thickened sonolucent area. It is a standardized measure obtained between 11 and 14 weeks of gestation to calculate the risk of a fetus being affected by a chromosomal aneuploidy. NT>3.5mm has been found to be associated with fetal chromosomal abnormalities and single-gene disorders as well as cardiac defects and other structural abnormalities in euploid and aneuploid fetuses. Proportionally as NT increases, even with a normal karyotype, there is a higher risk of adverse pregnancy outcomes such as miscarriage, intrauterine death, congenital heart defects and numerous other structural and genetic syndromes. There is not one single cause of increased NT, it is based on a complex and multifactorial process, linked to one or more embryonic processes. It has been shown that a persistently increased NT with a normal karyotype and aCGH has a 4-10% probability of being associated to Noonan Syndrome and/or other RASopathies using Whole Exome Sequencing (WES). However, the general tendency following detection of isolated enlarged NT in an euploid fetus is that most babies with normal detailed ultrasound examination and echocardiography will have uneventful outcomes. The Igenomix Increased Nuchal Translucency Precision Panel can be used to make a directed and accurate prenatal differential diagnosis of increased nuchal translucency in patients with or without a normal karyotype ultimately leading to a better management and prognosis of the associated comorbidities. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome -

Medical Genetics and Genomic Medicine in the United States of America
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by George Washington University: Health Sciences Research Commons (HSRC) Himmelfarb Health Sciences Library, The George Washington University Health Sciences Research Commons Pediatrics Faculty Publications Pediatrics 7-1-2017 Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease. Carlos R Ferreira George Washington University Debra S Regier George Washington University Donald W Hadley P Suzanne Hart Maximilian Muenke Follow this and additional works at: https://hsrc.himmelfarb.gwu.edu/smhs_peds_facpubs Part of the Genetics and Genomics Commons APA Citation Ferreira, C., Regier, D., Hadley, D., Hart, P., & Muenke, M. (2017). Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease.. Molecular Genetics and Genomic Medicine, 5 (4). http://dx.doi.org/10.1002/mgg3.318 This Journal Article is brought to you for free and open access by the Pediatrics at Health Sciences Research Commons. It has been accepted for inclusion in Pediatrics Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, please contact [email protected]. GENETICS AND GENOMIC MEDICINE AROUND THE WORLD Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease Carlos R. Ferreira1,2 , Debra S. Regier2, Donald W. Hadley1, P. Suzanne Hart1 & Maximilian Muenke1 1National Human Genome Research Institute, National Institutes of Health, Bethesda, Maryland 2Rare Disease Institute, Children’s National Health System, Washington, District of Columbia Correspondence Carlos R. -
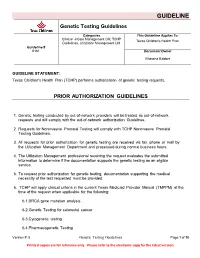
Genetic Testing Guidelines
GUIDELINE Genetic Testing Guidelines Categories This Guideline Applies To: Clinical Care Management CM, TCHP Texas Children's Health Plan Guidelines, Utilization Management UM Guideline # 6181 Document Owner Bhavana Babber GUIDELINE STATEMENT: Texas Children's Health Plan (TCHP) performs authorization of genetic testing requests. PRIOR AUTHORIZATION GUIDELINES 1. Genetic testing conducted by out-of-network providers will be treated as out-of-network requests and will comply with the out-of-network authorization Guidelines. 2. Requests for Noninvasive Prenatal Testing will comply with TCHP Noninvasive Prenatal Testing Guidelines. 3. All requests for prior authorization for genetic testing are received via fax, phone or mail by the Utilization Management Department and processed during normal business hours. 4. The Utilization Management professional receiving the request evaluates the submitted information to determine if the documentation supports the genetic testing as an eligible service. 5. To request prior authorization for genetic testing, documentation supporting the medical necessity of the test requested must be provided. 6. TCHP will apply clinical criteria in the current Texas Medicaid Provider Manual (TMPPM) at the time of the request when applicable for the following: 6.1.BRCA gene mutation analysis 6.2.Genetic Testing for colorectal cancer 6.3.Cytogenetic testing 6.4.Pharmacogenetic Testing Version #: 5 Genetic Testing Guidelines Page 1 of 10 Printed copies are for reference only. Please refer to the electronic copy for the latest version. GUIDELINE 6.5. A request for retroactive authorization must be submitted no later than seven calendar days beginning the day after the lab draw is performed per TMPPM 7. Whole genome sequencing (code 81415) requires preauthorization on a case-by-case basis. -

Crouzono-Dermo-Skeletal Syndrome, Crouzon Syndrome with Acanthosis Nigricans Syndrome
Journal of Perinatology (2014) 34, 164–165 & 2014 Nature America, Inc. All rights reserved 0743-8346/14 www.nature.com/jp IMAGING CASE REPORT Crouzono-dermo-skeletal syndrome, Crouzon syndrome with acanthosis nigricans syndrome TE Herman, K Sargar and MJ Siegel Journal of Perinatology (2014) 34, 164–165; doi:10.1038/jp.2013.139 CASE PRESENTATION mutation-associated conditions include five skeletal dysplasias: A 3495 g infant girl was born at 39 weeks gestation to a 17-year- achondroplasia, hypochondroplasia, thanatophoric dysplasia type 1 old gravida 1, para 0 mother. The mother had Crouzon syndrome 1, thanatophoric dysplasia type 2 and SADDAM syndrome. and hydrocephalus. She had undergone 11 craniofacial and plastic surgical procedures. The mother previously had genetic testing, which demonstrated a mutation in exon 10 of the FGFR3 (fibroblast growth factor receptor number 3) gene consistent with Crouzon syndrome with acanthosis nigricans (AN), also called Crouzono-dermo-skeletal syndrome (CDSS). No sonographic abnormalities were detected in the fetus during the pregnancy. At delivery, the infant had Apgars of 1 at 1 min, 6 at 5 min and 7 at 10 min. A nasogastric tube could not be passed. The patient was noted to have proptosis, depressed nasal bridge, hypertelorism, an anterior ectopic anus and normal appearing skin. Craniofacial computed tomography (CT) scan was performed (Figures 1 and 2) and plain radiographs of the pelvis and lumbar spine obtained (Figure 3). DENOUEMENT AND DISCUSSION The craniofacial CT scan demonstrates bicoronal synostosis with marked midface hypoplasia, with exophthalmos and hypertelor- ism. In addition, there was bilateral marked choanal stenosis. The pelvis (Figure 3) demonstrates squared-off iliac wings with small sciatic notches and narrowing of the lumbar interpediculate distances. -

Genetic Testing Medical Policy – Genetics
Genetic Testing Medical Policy – Genetics Please complete all appropriate questions fully. Suggested medical record documentation: • Current History & Physical • Progress Notes • Family Genetic History • Genetic Counseling Evaluation *Failure to include suggested medical record documentation may result in delay or possible denial of request. PATIENT INFORMATION Name: Member ID: Group ID: PROCEDURE INFORMATION Genetic Counseling performed: c Yes c No **Please check the requested analyte(s), identify number of units requested, and provide indication/rationale for testing. 81400 Molecular Pathology Level 1 Units _____ c ACADM (acyl-CoA dehydrogenase, C-4 to C-12 straight chain, MCAD) (e.g., medium chain acyl dehydrogenase deficiency), K304E variant _____ c ACE (angiotensin converting enzyme) (e.g., hereditary blood pressure regulation), insertion/deletion variant _____ c AGTR1 (angiotensin II receptor, type 1) (e.g., essential hypertension), 1166A>C variant _____ c BCKDHA (branched chain keto acid dehydrogenase E1, alpha polypeptide) (e.g., maple syrup urine disease, type 1A), Y438N variant _____ c CCR5 (chemokine C-C motif receptor 5) (e.g., HIV resistance), 32-bp deletion mutation/794 825del32 deletion _____ c CLRN1 (clarin 1) (e.g., Usher syndrome, type 3), N48K variant _____ c DPYD (dihydropyrimidine dehydrogenase) (e.g., 5-fluorouracil/5-FU and capecitabine drug metabolism), IVS14+1G>A variant _____ c F13B (coagulation factor XIII, B polypeptide) (e.g., hereditary hypercoagulability), V34L variant _____ c F2 (coagulation factor 2) (e.g., -

Craniosynostosis
European Journal of Human Genetics (2011) 19, 369–376 & 2011 Macmillan Publishers Limited All rights reserved 1018-4813/11 www.nature.com/ejhg PRACTICAL GENETICS In association with Craniosynostosis Craniosynostosis, defined as the premature fusion of the cranial sutures, presents many challenges in classification and treatment. At least 20% of cases are caused by specific single gene mutations or chromosome abnormalities. This article maps out approaches to clinical assessment of a child presenting with an unusual head shape, and illustrates how genetic analysis can contribute to diagnosis and management. In brief Apart from the genetic implications, it is important to recog- nise cases with a genetic cause because they are more likely to Craniosynostosis is best managed in a multispecialty tertiary be associated with multiple suture synostosis and extracranial referral unit. complications. Single suture synostosis affects the sagittal suture most com- Genes most commonly mutated in craniosynostosis are monly, followed by the coronal, metopic and lambdoid sutures. FGFR2, FGFR3, TWIST1 and EFNB1. Both environmental factors (especially intrauterine fetal head As well as being associated with syndromes, some clinically constraint) and genes (single gene mutations, chromosome non-syndromic synostosis (usually affecting the coronal abnormalities and polygenic background) predispose to cra- suture) can be caused by single gene mutations, particularly niosynostosis. the Pro250Arg mutation in FGFR3. Most genetically determined craniosynostosis is characterised In severe cases, initial care should be directed towards main- by autosomal dominant inheritance, but around half of cases tenance of the airway, support of feeding, eye protection and are accounted for by new mutations. treatment of raised intracranial pressure. -

Advantages and Disadvantages of Different Treatment Methods in Achondroplasia: a Review
International Journal of Molecular Sciences Review Advantages and Disadvantages of Different Treatment Methods in Achondroplasia: A Review Wiktoria Wrobel, Emilia Pach and Iwona Ben-Skowronek * Metabolic Laboratory, Department of Paediatric Endocrinology and Diabetology with Endocrine, Medical University in Lublin, Prof. A. Gebala Street 6, 20-093 Lublin, Poland; [email protected] (W.W.); [email protected] (E.P.) * Correspondence: [email protected]; Tel.: +48-817-185-440 Abstract: Achondroplasia (ACH) is a disease caused by a missense mutation in the FGFR3 (fibroblast growth factor receptor 3) gene, which is the most common cause of short stature in humans. The treatment of ACH is necessary and urgent because untreated achondroplasia has many complications, both orthopedic and neurological, which ultimately lead to disability. This review presents the current and potential pharmacological treatments for achondroplasia, highlighting the advantages and disadvantages of all the drugs that have been demonstrated in human and animal studies in different stages of clinical trials. The article includes the potential impacts of drugs on achondroplasia symptoms other than short stature, including their effects on spinal canal stenosis, the narrowing of the foramen magnum and the proportionality of body structure. Addressing these effects could significantly improve the quality of life of patients, possibly reducing the frequency and necessity of hospitalization and painful surgical procedures, which are currently the only therapeutic options used. The criteria for a good drug for achondroplasia are best met by recombinant human growth hormone at present and will potentially be met by vosoritide in the future, while the rest of the drugs Citation: Wrobel, W.; Pach, E.; are in the early stages of clinical trials. -

Congenital Hand Anomalies and Associated Syndromes Ghazi M
Congenital Hand Anomalies and Associated Syndromes Ghazi M. Rayan • Joseph Upton III Congenital Hand Anomalies and Associated Syndromes Editors Ghazi M. Rayan Joseph Upton III INTEGRIS Baptist Medical Center Chestnut Hill, USA Orthopaedic Surgery – Hand Oklahoma City, USA ISBN 978-3-642-54609-9 ISBN 978-3-642-54610-5 (eBook) DOI 10.1007/978-3-642-54610-5 Library of Congress Control Number: 2014946208 Springer © Springer-Verlag Berlin Heidelberg 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the mate- rial is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter devel- oped. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provi- sions of the Copyright Law of the Publisher´s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

Genetic Syndromes Associated with Craniosynostosis
www.jkns.or.kr http://dx.doi.org/10.3340/jkns.2016.59.3.187 Print ISSN 2005-3711 On-line ISSN 1598-7876 J Korean Neurosurg Soc 59 (3) : 187-191, 2016 Copyright © 2016 The Korean Neurosurgical Society Pediatric Issue Genetic Syndromes Associated with Craniosynostosis Jung Min Ko, M.D., Ph.D. Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea Craniosynostosis is defined as the premature fusion of one or more of the cranial sutures. It leads not only to secondary distortion of skull shape but to various complications including neurologic, ophthalmic and respiratory dysfunction. Craniosynostosis is very heterogeneous in terms of its causes, presentation, and management. Both environmental factors and genetic factors are associated with development of craniosynostosis. Nonsyndrom- ic craniosynostosis accounts for more than 70% of all cases. Syndromic craniosynostosis with a certain genetic cause is more likely to involve multi- ple sutures or bilateral coronal sutures. FGFR2, FGFR3, FGFR1, TWIST1 and EFNB1 genes are major causative genes of genetic syndromes associat- ed with craniosynostosis. Although most of syndromic craniosynostosis show autosomal dominant inheritance, approximately half of patients are de novo cases. Apert syndrome, Pfeiffer syndrome, Crouzon syndrome, and Antley-Bixler syndrome are related to mutations in FGFR family (especially in FGFR2), and mutations in FGFRs can be overlapped between different syndromes. Saethre-Chotzen syndrome, Muenke syndrome, and cranio- frontonasal syndrome are representative disorders showing isolated coronal suture involvement. Compared to the other types of craniosynostosis, single gene mutations can be more frequently detected, in one-third of coronal synostosis patients. Molecular diagnosis can be helpful to provide adequate genetic counseling and guidance for patients with syndromic craniosynostosis. -
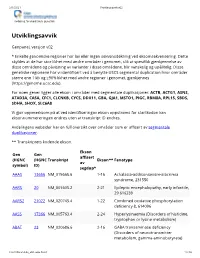
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Molocular Genetics Referral Department of Clinical Genetics Prøvenr.: Aarhus University Hospital
Molocular Genetics Referral Department of Clinical Genetics Prøvenr.: Aarhus University Hospital Patient name (label): Modtage dato: Date of birth Gender Male Female Familie nr.: Requesting physician: (capital letters) Clinic/Department Phone, fax, e-mail Billing to Person reference Postal address International Purchase Order (IPO) number Sample type Date Blood Your reference number: DNA Other tissue (tissue type) Clinical informations Family informations/proband Known mutation Screening Analyses DNA-analysis (please specify on page 2) (7,5 ml EDTA blood. Infants at least 3 ml EDTA blood) Array-CGH (180K, standard analyse) High resolution array-CGH (1000k) (7,5 ml EDTA blood and 2 ml Li-heparin blood) Chromosome analysis – blood (2 ml Li-heparin blood. Infants at least 0,5 ml Li-heparin blood.) Cytogenetic analysis for Fanconis anemia (5 ml Li-heparin blood, special conditions concerning sample shipment, see www.kga.skejby.dk) Chromosome analysis – other tissue FISH analysis for: (2 ml LI-heparin blood) continue on next page For Laboratory Use Only Lægevisitation Laboratoriesignatur / Department of Clinical Genetics Aarhus University Hospital Brendstrupgårdsvej 21 C, DK-8200 Aarhus N Tel. +45 7845 5510 • Fax: +45 8678 3181 • www.kga.auh.dk 1/2 Molocular Genetics Referral Patient name and date of birth (label) DNA-analyses Skeletal Dysplasia (7,5 ml EDTA- blood. Infants at least 3 ml EDTA- blood) Achondroplasia (FGFR3) Hypochondroplasia (FGFR3) Muscular Dystrophies Saethre-Chotzen syndrome (TWIST) Becker Muscular Dystrophy (DMD) Thanatophoric