Genetic Syndromes Associated with Craniosynostosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soonerstart Automatic Qualifying Syndromes and Conditions 001
SoonerStart Automatic Qualifying Syndromes and Conditions 001 Abetalipoproteinemia 272.5 002 Acanthocytosis (see Abetalipoproteinemia) 272.5 003 Accutane, Fetal Effects of (see Fetal Retinoid Syndrome) 760.79 004 Acidemia, 2-Oxoglutaric 276.2 005 Acidemia, Glutaric I 277.8 006 Acidemia, Isovaleric 277.8 007 Acidemia, Methylmalonic 277.8 008 Acidemia, Propionic 277.8 009 Aciduria, 3-Methylglutaconic Type II 277.8 010 Aciduria, Argininosuccinic 270.6 011 Acoustic-Cervico-Oculo Syndrome (see Cervico-Oculo-Acoustic Syndrome) 759.89 012 Acrocephalopolysyndactyly Type II 759.89 013 Acrocephalosyndactyly Type I 755.55 014 Acrodysostosis 759.89 015 Acrofacial Dysostosis, Nager Type 756.0 016 Adams-Oliver Syndrome (see Limb and Scalp Defects, Adams-Oliver Type) 759.89 017 Adrenoleukodystrophy, Neonatal (see Cerebro-Hepato-Renal Syndrome) 759.89 018 Aglossia Congenita (see Hypoglossia-Hypodactylia) 759.89 019 Albinism, Ocular (includes Autosomal Recessive Type) 759.89 020 Albinism, Oculocutaneous, Brown Type (Type IV) 759.89 021 Albinism, Oculocutaneous, Tyrosinase Negative (Type IA) 759.89 022 Albinism, Oculocutaneous, Tyrosinase Positive (Type II) 759.89 023 Albinism, Oculocutaneous, Yellow Mutant (Type IB) 759.89 024 Albinism-Black Locks-Deafness 759.89 025 Albright Hereditary Osteodystrophy (see Parathyroid Hormone Resistance) 759.89 026 Alexander Disease 759.89 027 Alopecia - Mental Retardation 759.89 028 Alpers Disease 759.89 029 Alpha 1,4 - Glucosidase Deficiency (see Glycogenosis, Type IIA) 271.0 030 Alpha-L-Fucosidase Deficiency (see Fucosidosis) -

Increased Nuchal Translucency Precision Panel
Increased Nuchal Translucency Precision Panel Overview Increased Nuchal Translucency (NT) is defined as an abnormal accumulation of fluid in the nuchal area, which is visualized as a thickened sonolucent area. It is a standardized measure obtained between 11 and 14 weeks of gestation to calculate the risk of a fetus being affected by a chromosomal aneuploidy. NT>3.5mm has been found to be associated with fetal chromosomal abnormalities and single-gene disorders as well as cardiac defects and other structural abnormalities in euploid and aneuploid fetuses. Proportionally as NT increases, even with a normal karyotype, there is a higher risk of adverse pregnancy outcomes such as miscarriage, intrauterine death, congenital heart defects and numerous other structural and genetic syndromes. There is not one single cause of increased NT, it is based on a complex and multifactorial process, linked to one or more embryonic processes. It has been shown that a persistently increased NT with a normal karyotype and aCGH has a 4-10% probability of being associated to Noonan Syndrome and/or other RASopathies using Whole Exome Sequencing (WES). However, the general tendency following detection of isolated enlarged NT in an euploid fetus is that most babies with normal detailed ultrasound examination and echocardiography will have uneventful outcomes. The Igenomix Increased Nuchal Translucency Precision Panel can be used to make a directed and accurate prenatal differential diagnosis of increased nuchal translucency in patients with or without a normal karyotype ultimately leading to a better management and prognosis of the associated comorbidities. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. -

A Novel Locus for Brachydactyly Type A1 on Chromosome 5P13.3-P13.2 C M Armour, M E Mccready, a Baig,Agwhunter, D E Bulman
186 LETTERS TO JMG J Med Genet: first published as 10.1136/jmg.39.3.189 on 1 March 2002. Downloaded from A novel locus for brachydactyly type A1 on chromosome 5p13.3-p13.2 C M Armour, M E McCready, A Baig,AGWHunter, D E Bulman ............................................................................................................................. J Med Genet 2002;39:186–189 he brachydactylies are a group of inherited disorders METHODS characterised by shortened or malformed digits that are The linkage study comprised 34 members including 20 Tthought to be the result of abnormal growth of the affected subjects and was conducted after approval by the phalanges and/or metacarpals. First classified by Bell into Children’s Hospital of Eastern Ontario Ethics Review Com- types A, B, C, D, and E, they were reclassified by Temtamy and mittee. McKusick1 and Fitch.2 Brachydactyly type A1 (BDA1, MIM Peripheral blood samples were taken with informed 112500) is characterised by shortened or absent middle consent from all participating family members, and a stand- phalanges. Often the second and fifth digits, as well as the first ard protocol was used to isolate DNA. A genome wide scan proximal phalanx, are the most severely affected. In addition, was initiated using 36 primer sets from the MAPPAIRS™ all of the small tubular bones tend to be reduced in size and microsatellite markers (Research Genetics, Huntsville, Ala- the metacarpals may be shortened, particularly the fifth bama), encompassing markers from 16 chromosomes. metacarpal. Radial/ulnar clinodactyly, as well as malformed or Particular emphasis was placed on markers from chromo- 11 absent epiphyses, have also been reported.12 Complex some 5 and 17, based on the report by Fukushima et al syndromes have been described in which BDA1 is one of a describing a translocation between 5q11.2 and 17q23 in a girl number of manifestations.3 with Klippel-Feil anomaly and BDA1. -

The Genetic Heterogeneity of Brachydactyly Type A1: Identifying the Molecular Pathways
The genetic heterogeneity of brachydactyly type A1: Identifying the molecular pathways Lemuel Jean Racacho Thesis submitted to the Faculty of Graduate Studies and Postdoctoral Studies in partial fulfillment of the requirements for the Doctorate in Philosophy degree in Biochemistry Specialization in Human and Molecular Genetics Department of Biochemistry, Microbiology and Immunology Faculty of Medicine University of Ottawa © Lemuel Jean Racacho, Ottawa, Canada, 2015 Abstract Brachydactyly type A1 (BDA1) is a rare autosomal dominant trait characterized by the shortening of the middle phalanges of digits 2-5 and of the proximal phalange of digit 1 in both hands and feet. Many of the brachymesophalangies including BDA1 have been associated with genetic perturbations along the BMP-SMAD signaling pathway. The goal of this thesis is to identify the molecular pathways that are associated with the BDA1 phenotype through the genetic assessment of BDA1-affected families. We identified four missense mutations that are clustered with other reported BDA1 mutations in the central region of the N-terminal signaling peptide of IHH. We also identified a missense mutation in GDF5 cosegregating with a semi-dominant form of BDA1. In two families we reported two novel BDA1-associated sequence variants in BMPR1B, the gene which codes for the receptor of GDF5. In 2002, we reported a BDA1 trait linked to chromosome 5p13.3 in a Canadian kindred (BDA1B; MIM %607004) but we did not discover a BDA1-causal variant in any of the protein coding genes within the 2.8 Mb critical region. To provide a higher sensitivity of detection, we performed a targeted enrichment of the BDA1B locus followed by high-throughput sequencing. -

Physician Service Fee Schedule-Affordable Care Act(ACA) Taxonomy Defined Rates Pricing Specialty 01E Fee Schedule Updated On: 6/26/2020
NC Medicaid Physician Services Fee Schedule (See Affordable Care Act (ACA) Tab for Applicable ACA Defined Taxonomy Rates) Provider Specialty 001 Fee Schedule Updated on: 6/26/2020 ***The Agency's fee schedule rates below were set as of January 1, 2014 unless otherwise noted*** Rate changes after January 1, 2014 are based on the January 1st RVU of the year in which the service was initally established. The inclusion of a rate on this table does not guarantee that a service is covered. Please refer to the Medicaid Billing Guide and the Medicaid and Health Choice Clinical Policies on the DHB Web Site. Providers should always bill their usual and customary charges. Please use the monthly NC Medicaid Bulletins for additions, changes and deletion to this schedule. Medicaid Maximum Allowable NON-FACILITY Effective FEE END DATE PROCEDURE CODE MODIFIER PROCEDURE DESCRIPTION FACILITY RATE RATE Date of Rate 01967 ANESTH/ANALG VAG DELIVERY $ 220.11 $ 220.11 3/1/2020 12/31/9999 01996 HOSP MANAGE CONT DRUG ADMIN $ 40.88 $ 40.88 3/1/2020 12/31/9999 10004 FNA BX W/O IMG GDN EA ADDL $ 38.83 $ 46.10 3/1/2020 12/31/9999 10005 FNA BX W/US GDN 1ST LES $ 65.75 $ 110.89 3/1/2020 12/31/9999 10006 FNA BX W/US GDN EA ADDL $ 44.80 $ 53.29 3/1/2020 12/31/9999 10007 FNA BX W/FLUOR GDN 1ST LES $ 84.41 $ 247.72 3/1/2020 12/31/9999 10008 FNA BX W/FLUOR GDN EA ADDL $ 55.05 $ 139.88 3/1/2020 12/31/9999 10009 FNA BX W/CT GDN 1ST LES $ 102.46 $ 404.53 3/1/2020 12/31/9999 10010 FNA BX W/CT GDN EA ADDL $ 74.89 $ 244.25 3/1/2020 12/31/9999 10011 FNA BX W/MR GDN 1ST LES $ 54.57 -

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

Orphanet Journal of Rare Diseases Biomed Central
Orphanet Journal of Rare Diseases BioMed Central Review Open Access Brachydactyly Samia A Temtamy* and Mona S Aglan Address: Department of Clinical Genetics, Human Genetics and Genome Research Division, National Research Centre (NRC), El-Buhouth St., Dokki, 12311, Cairo, Egypt Email: Samia A Temtamy* - [email protected]; Mona S Aglan - [email protected] * Corresponding author Published: 13 June 2008 Received: 4 April 2008 Accepted: 13 June 2008 Orphanet Journal of Rare Diseases 2008, 3:15 doi:10.1186/1750-1172-3-15 This article is available from: http://www.ojrd.com/content/3/1/15 © 2008 Temtamy and Aglan; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Brachydactyly ("short digits") is a general term that refers to disproportionately short fingers and toes, and forms part of the group of limb malformations characterized by bone dysostosis. The various types of isolated brachydactyly are rare, except for types A3 and D. Brachydactyly can occur either as an isolated malformation or as a part of a complex malformation syndrome. To date, many different forms of brachydactyly have been identified. Some forms also result in short stature. In isolated brachydactyly, subtle changes elsewhere may be present. Brachydactyly may also be accompanied by other hand malformations, such as syndactyly, polydactyly, reduction defects, or symphalangism. For the majority of isolated brachydactylies and some syndromic forms of brachydactyly, the causative gene defect has been identified. -

Craniofacial Development After Three Different Palatoplasties in Children Born with Isolated Cleft Palate
From the DEPARTMENT OF DENTAL MEDICINE Karolinska Institutet, Stockholm, Sweden CRANIOFACIAL DEVELOPMENT AFTER THREE DIFFERENT PALATOPLASTIES IN CHILDREN BORN WITH ISOLATED CLEFT PALATE Konstantinos A. Parikakis Stockholm 2018 All previously published papers were reproduced with permission from the publisher Published by Karolinska Institutet Printed by Eprint AB 2018 © Konstantinos A. Parikakis, 2018 ISBN 978-91-7831-277-1 Craniofacial development after three different palatoplasties in children born with isolated cleft palate THESIS FOR DOCTORAL DEGREE (Ph.D.) By Konstantinos A. Parikakis Principal Supervisor: Opponent: Associate Professor Agneta Karsten Professor David Rice Karolinska Institutet University of Helsinki Department of Dental Medicine Department of Orthodontics Division of Orthodontics and Pedodontics Examination Board: Co-supervisor(s): Associate Professor Magnus Becker Associate Professor Ola Larson University of Lund Karolinska University Hospital Department of Plastic and Reconstructive Surgery Department of Reconstructive Plastic Surgery Professor Britt Gustafsson Karolinska Institutet Department of Clinical Science, Intervention and Technology (CLINTEC) Division of Pediatrics Associate Professor Farhan Bazargani University of Örebro Centrum för Specialisttandvard Department of Orthodontics To Christina, little Anastasios and…forthcoming Vassilios “Wherever the art of Medicine is loved, there is also a love of Humanity” Hippocrates of Kos, c.460-370 B.C. ABSTRACT Introduction: Different palatoplasties are applied for -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome -

Free PDF Download
Eur opean Rev iew for Med ical and Pharmacol ogical Sci ences 2015; 19: 4549-4552 Concomitance of types D and E brachydactyly: a case report T. TÜLAY KOCA 1, F. ÇILEDA ğ ÖZDEMIR 2 1Malatya State Hospital, Physical Medicine and Rehabilitation Clinic, Malatya, Turkey 2Inonu University School of Medicine, Department of Physical Medicine and Rehabilitation, Malatya, Turkey Abstract. – Here, we present of a 35-year old examination, it was determined that the patient, female diagnosed with an overlapping form of who had kyphotic posture and brachydactyly in non-syndromic brachydactyly types D and E the 3 rd and 4 th finger of the right hand, in the 4th with phenotypic and radiological signs. There finger of the left hand and clinodactyly with was observed to be shortening in the right hand th metacarpal of 3 rd and 4 th fingers and left hand brachdactyly in the 4 toe of the left foot (Fig - metacarpal of 4 th finger and left foot metatarsal ures 1 and 2). It was learned that these deformi - of 4 th toe. There was also shortening of the distal ties had been present since birth and a younger phalanx of the thumbs and thoracic kyphosis. sister had similar shortness of the fingers. There The syndromic form of brachydactyly type E is was no known systemic disease. The menstrual firmly associated with pseudo-hypopthyroidism cycle was regular and there was no known his - as resistance to pthyroid hormone is the most prominent feature. As the patient had normal tory of osteoporosis. In the laboratory tests, the stature, normal laboratory parameters and no results of full blood count, sedimentation, psychomotor developmental delay, the case was parathormon (PTH), vitamin D, calcium, alka - classified as isolated E type brachydactyly. -

Medical Genetics and Genomic Medicine in the United States of America
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by George Washington University: Health Sciences Research Commons (HSRC) Himmelfarb Health Sciences Library, The George Washington University Health Sciences Research Commons Pediatrics Faculty Publications Pediatrics 7-1-2017 Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease. Carlos R Ferreira George Washington University Debra S Regier George Washington University Donald W Hadley P Suzanne Hart Maximilian Muenke Follow this and additional works at: https://hsrc.himmelfarb.gwu.edu/smhs_peds_facpubs Part of the Genetics and Genomics Commons APA Citation Ferreira, C., Regier, D., Hadley, D., Hart, P., & Muenke, M. (2017). Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease.. Molecular Genetics and Genomic Medicine, 5 (4). http://dx.doi.org/10.1002/mgg3.318 This Journal Article is brought to you for free and open access by the Pediatrics at Health Sciences Research Commons. It has been accepted for inclusion in Pediatrics Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, please contact [email protected]. GENETICS AND GENOMIC MEDICINE AROUND THE WORLD Medical genetics and genomic medicine in the United States of America. Part 1: history, demographics, legislation, and burden of disease Carlos R. Ferreira1,2 , Debra S. Regier2, Donald W. Hadley1, P. Suzanne Hart1 & Maximilian Muenke1 1National Human Genome Research Institute, National Institutes of Health, Bethesda, Maryland 2Rare Disease Institute, Children’s National Health System, Washington, District of Columbia Correspondence Carlos R. -
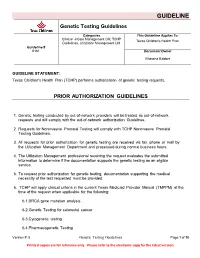
Genetic Testing Guidelines
GUIDELINE Genetic Testing Guidelines Categories This Guideline Applies To: Clinical Care Management CM, TCHP Texas Children's Health Plan Guidelines, Utilization Management UM Guideline # 6181 Document Owner Bhavana Babber GUIDELINE STATEMENT: Texas Children's Health Plan (TCHP) performs authorization of genetic testing requests. PRIOR AUTHORIZATION GUIDELINES 1. Genetic testing conducted by out-of-network providers will be treated as out-of-network requests and will comply with the out-of-network authorization Guidelines. 2. Requests for Noninvasive Prenatal Testing will comply with TCHP Noninvasive Prenatal Testing Guidelines. 3. All requests for prior authorization for genetic testing are received via fax, phone or mail by the Utilization Management Department and processed during normal business hours. 4. The Utilization Management professional receiving the request evaluates the submitted information to determine if the documentation supports the genetic testing as an eligible service. 5. To request prior authorization for genetic testing, documentation supporting the medical necessity of the test requested must be provided. 6. TCHP will apply clinical criteria in the current Texas Medicaid Provider Manual (TMPPM) at the time of the request when applicable for the following: 6.1.BRCA gene mutation analysis 6.2.Genetic Testing for colorectal cancer 6.3.Cytogenetic testing 6.4.Pharmacogenetic Testing Version #: 5 Genetic Testing Guidelines Page 1 of 10 Printed copies are for reference only. Please refer to the electronic copy for the latest version. GUIDELINE 6.5. A request for retroactive authorization must be submitted no later than seven calendar days beginning the day after the lab draw is performed per TMPPM 7. Whole genome sequencing (code 81415) requires preauthorization on a case-by-case basis.