Identifying the Misshapen Head: Craniosynostosis and Related Disorders Mark S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
New Guidelines Review Evidence on PT, Helmets for Positional Plagiocephaly by Sandi K
Neurologic Disorders, Neurological Surgery, News Articles New guidelines review evidence on PT, helmets for positional plagiocephaly by Sandi K. Lam M.D., M.B.A., FACS; Thomas G. Luerssen M.D., FACS, FAAP Positional plagiocephaly is a common condition encountered by pediatricians and referred to pediatric subspecialty physicians such as neurosurgeons and plastic surgeons. About one in four U.S. infants has some degree of positional plagiocephaly. The incidence has increased since the Academy initiated the Back to Sleep campaign in 1994 to prevent sudden infant death syndrome. Due to practice variation in diagnosis and treatment paradigms for this common condition, the Joint Section on Pediatric Neurosurgery of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons (CNS) sought to develop evidence-based management guidelines. A multidisciplinary task force conducted a systematic review of the literature from 1966 to October 2014 on pediatric plagiocephaly. Nearly 400 abstracts were reviewed yielding 110 articles for full review; 60 were deemed relevant. The task force made 10 recommendations pertaining to imaging diagnosis, repositioning, physical therapy and helmet orthoses. The guidelines are published in CNS' journal Neurosurgery and have been endorsed by the Academy. They are available at http://bit.ly/2d7NzS1. Definition of positional plagiocephaly In the guidelines, the term positional plagiocephaly encompasses both positional occipital plagiocephaly (unilateral flattening of parieto-occipital region, compensatory anterior shift of the ipsilateral ear, bulging of the ipsilateral forehead) and positional brachycephaly (symmetric flattening of the occiput, foreshortened anterior- posterior dimension of the skull, compensatory biparietal widening) and the combination of both of these deformities. -

Pfeiffer Syndrome Type II Discovered Perinatally
Diagnostic and Interventional Imaging (2012) 93, 785—789 CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector LETTER / Musculoskeletal imaging Pfeiffer syndrome type II discovered perinatally: Report of an observation and review of the literature a,∗ a a a H. Ben Hamouda , Y. Tlili , S. Ghanmi , H. Soua , b c b a S. Jerbi , M.M. Souissi , H. Hamza , M.T. Sfar a Unité de néonatologie, service de pédiatrie, CHU Tahar Sfar, 5111 Mahdia, Tunisia b Service de radiologie, CHU Tahar Sfar, 5111 Mahdia, Tunisia c Service de gynéco-obstétrique, CHU Tahar Sfar, 5111 Mahdia, Tunisia Pfeiffer syndrome, described for the first time by Pfeiffer in 1964, is a rare hereditary KEYWORDS condition combining osteochondrodysplasia with craniosynostosis [1]. This syndrome is Pfeiffer syndrome; also called acrocephalosyndactyly type 5, which is divided into three sub-types. Type I Cloverleaf skull; is the classic Pfeiffer syndrome, with autosomal dominant transmission, often associated Craniosynostosis; with normal intelligence. Types II and III occur as sporadic cases in individuals who have Syndactyly; craniosynostosis with broad thumbs, broad big toes, ankylosis of the elbows and visceral Prenatal diagnosis abnormalities [2]. We report a case of Pfeiffer syndrome type II, discovered perinatally, which is distinguished from type III by the skull appearing like a cloverleaf, and we shall discuss the clinical, radiological and evolutive features and the advantage of prenatal diagnosis of this syndrome with a review of the literature. Observation The case involved a male premature baby born at 36 weeks of amenorrhoea with multiple deformities at birth. The parents were not blood-related and in good health who had two other boys and a girl with normal morphology. -

A Novel Locus for Brachydactyly Type A1 on Chromosome 5P13.3-P13.2 C M Armour, M E Mccready, a Baig,Agwhunter, D E Bulman
186 LETTERS TO JMG J Med Genet: first published as 10.1136/jmg.39.3.189 on 1 March 2002. Downloaded from A novel locus for brachydactyly type A1 on chromosome 5p13.3-p13.2 C M Armour, M E McCready, A Baig,AGWHunter, D E Bulman ............................................................................................................................. J Med Genet 2002;39:186–189 he brachydactylies are a group of inherited disorders METHODS characterised by shortened or malformed digits that are The linkage study comprised 34 members including 20 Tthought to be the result of abnormal growth of the affected subjects and was conducted after approval by the phalanges and/or metacarpals. First classified by Bell into Children’s Hospital of Eastern Ontario Ethics Review Com- types A, B, C, D, and E, they were reclassified by Temtamy and mittee. McKusick1 and Fitch.2 Brachydactyly type A1 (BDA1, MIM Peripheral blood samples were taken with informed 112500) is characterised by shortened or absent middle consent from all participating family members, and a stand- phalanges. Often the second and fifth digits, as well as the first ard protocol was used to isolate DNA. A genome wide scan proximal phalanx, are the most severely affected. In addition, was initiated using 36 primer sets from the MAPPAIRS™ all of the small tubular bones tend to be reduced in size and microsatellite markers (Research Genetics, Huntsville, Ala- the metacarpals may be shortened, particularly the fifth bama), encompassing markers from 16 chromosomes. metacarpal. Radial/ulnar clinodactyly, as well as malformed or Particular emphasis was placed on markers from chromo- 11 absent epiphyses, have also been reported.12 Complex some 5 and 17, based on the report by Fukushima et al syndromes have been described in which BDA1 is one of a describing a translocation between 5q11.2 and 17q23 in a girl number of manifestations.3 with Klippel-Feil anomaly and BDA1. -

FROGLOG Newsletter of the Declining Amphibian Populations Task Force
Salamandra salamandra by Franco Andreone ISSN 1026-0269 FROGLOG Newsletter of the Declining Amphibian Populations Task Force August 2004, Number 64. Meteyer et al. (2000) and Ouellet very low number of abnormalities. We (2000). only found one L. kuhlii, which may We examined a total of 4,331 have strayed from a nearby stream. frogs of 23 species and found 20 A third of abnormalities were types of deformities in 9 species of due to trauma; these included digit frogs. We divided deformities into two amputations (16% of all general types: developmental abnormalities), limb amputations (2%), abnormalities and trauma (injuries). fractured limbs (7%) and skin wounds Morphological Abnormalities in We distinguished trauma (4%). The most common Frogs of West Java, Indonesia abnormalities based on the developmental abnormalities were appearance of old scars or, if they digital (43%) and, of these, By Mirza D. Kusrini, Ross A. Alford, involved digits, the occurrence of brachydactyly (16.3%), syndactyly Anisa Fitri, Dede M. Nasir, Sumantri digital re-growth. Developmental (14.6%) and ectrodactyly (11.4%) Rahardyansah abnormalities occurred in limbs were the three most common. In recent decades, amphibian (amelia, micromelia, brachymelia, The oldest specimen of F. deformities have generated public hemimelia, ectromelia, taumelia, cuta- limnocharis stored in the MZB that interest as high incidences have been neous fusions), digits (ectrodactyly, exhibited abnormalities was a juvenile found in several locations, notably in brachydactyly, syndactyly, polydactyly, frog captured on 16 November 1921 North America (Helgen et al., 1998; clinodactyly), the back-bone (scoli- from Bogor without one leg (amelia) Ouellet, 2000). The only report on the osis), the eyes (anophthalmy) and the (ID057.10). -

Nasal Morphology and Its Correlation to Craniofacial Morphology in Lateral Cephalometric Analysis
International Journal of Environmental Research and Public Health Article Nasal Morphology and Its Correlation to Craniofacial Morphology in Lateral Cephalometric Analysis Agnieszka Jankowska 1 , Joanna Janiszewska-Olszowska 2,* and Katarzyna Grocholewicz 2 1 Private Practice “Dental Clinic Jankowscy”, 68-200 Zary,˙ Poland; [email protected] 2 Department of Interdisciplinary Dentistry, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-91-466-1690 Abstract: Nose shape, size, and inclination influence facial appearance, but few studies concern the relationship between the nasal profile and craniofacial structures. The objective of this study was to analyze association of nasal cephalometric variables with skeletal structures, age, and sex. Cephalometric and nasal analysis was performed in 386 Polish orthodontic patients (aged 9–25 years). Student t-test and Mann–Whitney test were used to compare quantitative variables and Pearson’s or Spearman’s correlation coefficients—to find correlations. Soft tissue facial convexity angle corre- lates to Holdaway ratio, ANB (A-Nasion-B), and Wits appraisal. Nasal dorsum axis, nose length, nose depth (1) and nose depth (2), nose hump, lower dorsum convexity, and columella convexity increase with age. Nasal base angle, nasolabial angle, nasomental angle, soft tissue facial convex- ity and nasal bone angle decrease with age. Nasal base angle and nasomental angle are smaller in females. Thus, a relationship exists between nasal morphology and sagittal jaw configuration. Nasal parameters significantly change with age. Sexual dimorphism characterizes nasal bone angle Citation: Jankowska, A.; and nasomental angle. Janiszewska-Olszowska, J.; Grocholewicz, K. Nasal Morphology Keywords: nose; nose profile; cephalometry; orthodontics and Its Correlation to Craniofacial Morphology in Lateral Cephalometric Analysis. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

The Genetic Heterogeneity of Brachydactyly Type A1: Identifying the Molecular Pathways
The genetic heterogeneity of brachydactyly type A1: Identifying the molecular pathways Lemuel Jean Racacho Thesis submitted to the Faculty of Graduate Studies and Postdoctoral Studies in partial fulfillment of the requirements for the Doctorate in Philosophy degree in Biochemistry Specialization in Human and Molecular Genetics Department of Biochemistry, Microbiology and Immunology Faculty of Medicine University of Ottawa © Lemuel Jean Racacho, Ottawa, Canada, 2015 Abstract Brachydactyly type A1 (BDA1) is a rare autosomal dominant trait characterized by the shortening of the middle phalanges of digits 2-5 and of the proximal phalange of digit 1 in both hands and feet. Many of the brachymesophalangies including BDA1 have been associated with genetic perturbations along the BMP-SMAD signaling pathway. The goal of this thesis is to identify the molecular pathways that are associated with the BDA1 phenotype through the genetic assessment of BDA1-affected families. We identified four missense mutations that are clustered with other reported BDA1 mutations in the central region of the N-terminal signaling peptide of IHH. We also identified a missense mutation in GDF5 cosegregating with a semi-dominant form of BDA1. In two families we reported two novel BDA1-associated sequence variants in BMPR1B, the gene which codes for the receptor of GDF5. In 2002, we reported a BDA1 trait linked to chromosome 5p13.3 in a Canadian kindred (BDA1B; MIM %607004) but we did not discover a BDA1-causal variant in any of the protein coding genes within the 2.8 Mb critical region. To provide a higher sensitivity of detection, we performed a targeted enrichment of the BDA1B locus followed by high-throughput sequencing. -

Crouzon Syndrome with Ophthalmological Complications
Journal of Rawalpindi Medical College (JRMC); 2012;16(1):80-81 Case Report Crouzon Syndrome With Ophthalmological Complications Rahela Nasir Paediatric Department, Capital Hospital, CDA Islamabad. Crouzon Syndrome is characterized by premature bilateral optic atrophy. Other facial features included a craniosynostosis. It has an autosomal dominant inheritance prominent nose and deep and narrow palate. No but represents fresh mutation also. Other craniofacial digital abnormalities were seen. No dental aplasia was abnormalities include ocular proptosis caused by shallow present. Systemic examination revealed no orbits with or without divergent strabismus. There may be abnormality. increased intracranial pressure for which surgical morcellation procedures are indicated. A case of He was diagnosed as a case of Crouzon syndrome craniosynostosis is reported which is diagnosed as Crouzon with ocular complications on clinical basis. He was Syndrome with ocular complications on clinical grounds. investigated for microcephaly and suspected Split craniotomy was performed by a neurosurgeon to craniosynostosis. Radiographs of skull showed small relieve raised intracranial pressure and to enhance brain sized skull with early closure of sutures and fontanelle growth. Crouzon Syndrome was originally described in 1912 suggestive of craniosynstosis(Fig 2). A hammered- by Crouzon in a mother and her daughter. It is an autosomal silver (beaten metal/ copper beaten) appearance was dominant inherited disorder but represents fresh mutation also seen due to raised intracranial pressure and also. Crouzon syndrome is characterized by premature compression of the developing brain on the fused craniosynostosis which is quite variable but the coronal suture is nearly always bilaterally involved. Craniofacial bone. CT scan brain with contrast was done which abnormalities include brachycephaly, shallow orbits and confirmed the features suggestive of craniosynostosis maxillary hypoplasia. -

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

Syndromic Ear Anomalies and Renal Ultrasounds
Syndromic Ear Anomalies and Renal Ultrasounds Raymond Y. Wang, MD*; Dawn L. Earl, RN, CPNP‡; Robert O. Ruder, MD§; and John M. Graham, Jr, MD, ScD‡ ABSTRACT. Objective. Although many pediatricians cific MCA syndromes that have high incidences of renal pursue renal ultrasonography when patients are noted to anomalies. These include CHARGE association, Townes- have external ear malformations, there is much confusion Brocks syndrome, branchio-oto-renal syndrome, Nager over which specific ear malformations do and do not syndrome, Miller syndrome, and diabetic embryopathy. require imaging. The objective of this study was to de- Patients with auricular anomalies should be assessed lineate characteristics of a child with external ear malfor- carefully for accompanying dysmorphic features, includ- mations that suggest a greater risk of renal anomalies. We ing facial asymmetry; colobomas of the lid, iris, and highlight several multiple congenital anomaly (MCA) retina; choanal atresia; jaw hypoplasia; branchial cysts or syndromes that should be considered in a patient who sinuses; cardiac murmurs; distal limb anomalies; and has both ear and renal anomalies. imperforate or anteriorly placed anus. If any of these Methods. Charts of patients who had ear anomalies features are present, then a renal ultrasound is useful not and were seen for clinical genetics evaluations between only in discovering renal anomalies but also in the diag- 1981 and 2000 at Cedars-Sinai Medical Center in Los nosis and management of MCA syndromes themselves. Angeles and Dartmouth-Hitchcock Medical Center in A renal ultrasound should be performed in patients with New Hampshire were reviewed retrospectively. Only pa- isolated preauricular pits, cup ears, or any other ear tients who underwent renal ultrasound were included in anomaly accompanied by 1 or more of the following: the chart review. -
Macrocephaly Information Sheet 6-13-19
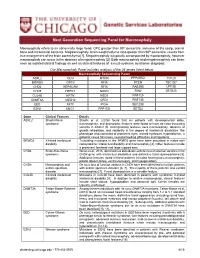
Next Generation Sequencing Panel for Macrocephaly Clinical Features: Macrocephaly refers to an abnormally large head, OFC greater than 98th percentile, inclusive of the scalp, cranial bone and intracranial contents. Megalencephaly, brain weight/volume ratio greater than 98th percentile, results from true enlargement of the brain parenchyma [1]. Megalencephaly is typically accompanied by macrocephaly, however macrocephaly can occur in the absence of megalencephaly [2]. Both macrocephaly and megalencephaly can been seen as isolated clinical findings as well as clinical features of a mutli-systemic syndromic diagnosis. Our Macrocephaly Panel includes analysis of the 36 genes listed below. Macrocephaly Sequencing Panel ASXL2 GLI3 MTOR PPP2R5D TCF20 BRWD3 GPC3 NFIA PTEN TBC1D7 CHD4 HEPACAM NFIX RAB39B UPF3B CHD8 HERC1 NONO RIN2 ZBTB20 CUL4B KPTN NSD1 RNF125 DNMT3A MED12 OFD1 RNF135 EED MITF PIGA SEC23B EZH2 MLC1 PPP1CB SETD2 Gene Clinical Features Details ASXL2 Shashi-Pena Shashi et al. (2016) found that six patients with developmental delay, syndrome macrocephaly, and dysmorphic features were found to have de novo truncating variants in ASXL2 [3]. Distinguishing features were macrocephaly, absence of growth retardation, and variability in the degree of intellectual disabilities The phenotype also consisted of prominent eyes, arched eyebrows, hypertelorism, a glabellar nevus flammeus, neonatal feeding difficulties and hypotonia. BRWD3 X-linked intellectual Truncating mutations in the BRWD3 gene have been described in males with disability nonsyndromic intellectual disability and macrocephaly [4]. Other features include a prominent forehead and large cupped ears. CHD4 Sifrim-Hitz-Weiss Weiss et al., 2016, identified five individuals with de novo missense variants in the syndrome CHD4 gene with intellectual disabilities and distinctive facial dysmorphisms [5]. -
Craniosynostosis and Related Disorders Mark S
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care Identifying the Misshapen Head: Craniosynostosis and Related Disorders Mark S. Dias, MD, FAAP, FAANS,a Thomas Samson, MD, FAAP,b Elias B. Rizk, MD, FAAP, FAANS,a Lance S. Governale, MD, FAAP, FAANS,c Joan T. Richtsmeier, PhD,d SECTION ON NEUROLOGIC SURGERY, SECTION ON PLASTIC AND RECONSTRUCTIVE SURGERY Pediatric care providers, pediatricians, pediatric subspecialty physicians, and abstract other health care providers should be able to recognize children with abnormal head shapes that occur as a result of both synostotic and aSection of Pediatric Neurosurgery, Department of Neurosurgery and deformational processes. The purpose of this clinical report is to review the bDivision of Plastic Surgery, Department of Surgery, College of characteristic head shape changes, as well as secondary craniofacial Medicine and dDepartment of Anthropology, College of the Liberal Arts characteristics, that occur in the setting of the various primary and Huck Institutes of the Life Sciences, Pennsylvania State University, State College, Pennsylvania; and cLillian S. Wells Department of craniosynostoses and deformations. As an introduction, the physiology and Neurosurgery, College of Medicine, University of Florida, Gainesville, genetics of skull growth as well as the pathophysiology underlying Florida craniosynostosis are reviewed. This is followed by a description of each type of Clinical reports from the American Academy of Pediatrics benefit from primary craniosynostosis (metopic, unicoronal, bicoronal, sagittal, lambdoid, expertise and resources of liaisons and internal (AAP) and external reviewers. However, clinical reports from the American Academy of and frontosphenoidal) and their resultant head shape changes, with an Pediatrics may not reflect the views of the liaisons or the emphasis on differentiating conditions that require surgical correction from organizations or government agencies that they represent.