Changes in Intraocular Pressure After Pharmacologic Pupil Dilation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -
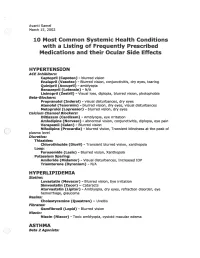
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Eye (2018) 32, 457–459 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2 2 2 Intermittent mydriasis PD Chamberlain , A Sadaka , S Berry CASE SERIES 1,2,3,4,5,6 associated with carotid and AG Lee vascular occlusion Abstract the literature as benign episodic pupillary dilation or BEUM. We report two patients with Purpose To describe two cases of 1 stereotyped, intermittent, neurologically acquired occlusive disease of the ipsilateral ICA Department of Ophthalmology, Blanton isolated, unilateral mydriasis in patients who developed multiple, stereotyped, neurologically isolated, transient episodes of Eye Institute, Houston with a history of acquired internal carotid Methodist Hospital, artery (ICA) occlusive disease on the mydriasis consistent with BEUM. We discuss the Houston, TX, USA ipsilateral side. possible mechanisms, differential diagnosis and 2 Patients Two patients with intermittent recommended evaluation for atypical cases for Department of episodic mydriasis. Ophthalmology, Baylor mydriasis. College of Medicine, Methods Case Series. Houston, TX, USA Results Case one: A 78-year-old man Case one 3 experienced 10 episodes of intermittent, Departments of Ophthalmology, Neurology, unilateral, and painless mydriasis in the left A 78-year-old man presented with 10 episodes of and Neurosurgery, Weill stereotyped, intermittent, unilateral, painless eye and had 100% occlusion of the left ICA Cornell Medical College, artery due to atherosclerotic disease. Case two: pupillary dilation of the left eye (OS) lasting New York, NY, USA A 26-year-old woman with history of migraine minutes to hours at a time without diplopia or fi 4Department of developed new painless, intermittent episodes ptosis. -

Miotic Adie's Pupils
Journal of Cll/lical Neuro-ophtllJllmology 9(1): 43-45, 1989. RilVen Press, Ltd., New York Miotic Adie's Pupils Michael L. Rosenberg, M.D. Two young adults, aged 24 and 31, had a long history of Adie's syndrome or, pupillotonia, is typically small, poorly reactive pupilS. There was no history of characterized by either unilaterally or bilaterally large pupils, and a review of old photographs confirmed enlarged pupils that are unresponsive to light (1). 10 and 5 years, respectively, of miosis. Both were found to have bilateral tonic pupils that were supersensitive to The diagnosis is made clinically by watching for a diluted pilocarpine. Although it is possible that they had tonic constriction to near stimulation followed by a an unusually early onset of bilateral Adie's syndrome tonic redilatation. with dilated pupils that was not noticed, it is suggested Two young adults are described who were noted that some patients might have primary miotic Adie's during routine examinations to have bilaterally mi pupils without ever passing through a mydriatic phase. Key Words: Adie's syndrome-Argyll Robertson pu otic pupils that were thought to be fixed to light. pils-Miosis. They were both referred for the evaluation of Ar gyll Robertson pupils. Evaluation revealed bilat eral tonic reactions to near stimulation in both pa tients, typical of Adie's tonic pupilS. The diagnosis of parasympathetic denervation was confirmed in both patients as their pupils constricted with di luted pilocarpine. The cases reinforce the principle that any pupil regardless of size should be evalu ated for the possibility of pupillotonia. -

Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia
CASE REPORT Print ISSN 1738-6586 / On-line ISSN 2005-5013 J Clin Neurol 2014 Open Access Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia Fabrice C. Deprez,a Julie Coulier,b Denis Rommel,a Antonella Boschib aDepartments of Radiology and bOphthalmology, Cliniques Universitaires Saint-Luc, UCL, Brussels, Belgium BackgroundzzHorner syndrome (HS), also known as Claude-Bernard-Horner syndrome or Received August 5, 2013 oculosympathetic palsy, comprises ipsilateral ptosis, miosis, and facial anhidrosis. Revised April 15, 2014 Accepted April 21, 2014 Case ReportzzWe report herein the case of a 67-year-old man who presented with congenital HS associated with ipsilateral hypoplasia of the internal carotid artery (ICA), as revealed by Correspondence heterochromia iridis and confirmed by computed tomography (CT). Fabrice C. Deprez, MD Department of Radiology, ConclusionszzCT evaluation of the skull base is essential to establish this diagnosis and dis- Cliniques Universitaires Saint-Luc, tinguish aplasia from agenesis/hypoplasia (by the absence or hypoplasia of the carotid canal) or UCL, Avenue Hippocrate 10, from acquired ICA obstruction as demonstrated by angiographic CT. 1200 Woluwe-Saint-Lambert, J Clin Neurol 2014 Belgium Tel +32.472.93.34.80 Key Wordszzcongenital horner syndrome, internal carotid artery agenesis, Fax +32.81.42.35.05 heterochromia iridis, computed tomography. E-mail [email protected] Introduction spindly left ICA, which was misinterpreted as ICA thrombosis (Fig. 1). The left anterior cerebral artery and MCA were sup- Horner syndrome (HS), also known as Claude-Bernard-Horn- plied by a large posterior communicating artery from the bas- er syndrome or oculosympathetic palsy, comprises ipsilateral ilar artery. -

Pupil Dilatation with Tropicamide. the Effects on Acuity, Accommodation and Refraction
Eye (1989) 3, 845-848 Pupil Dilatation with Tropicamide. The Effects on Acuity, Accommodation and Refraction D. M. I. MONTGOMERY! and C. J. MACEWANZ Glasgow and Dundee. Summary The effect of pupil dilatation with tropicamide 1 % on visual acuity and accommo dation was assessed in 100 eyes of 52 consecutive patients attending the general ophthalmic outpatient clinic. Snellen visual acuity remained unchanged in 55 eyes and deteriorated by one line in 41 eyes. The remaining four eyes deteriorated by two lines. Tropicamide gave rise to a reduction in the amplitude of accommodation which tended to vary inversely with the age of the patient. However, all patients who wore reading glasses for presbyopia were still able to read when their pupils had been dilated. Many drugs are used routinely in ophthalmic acuity and accommodation in such a practice to dilate the pupil for adequate exam population. ination of the ocular fundus. Selection may be based on the speed of onset and duration of action of the drug as well as on the presence Materials and methods and severity of any unwanted effects such as Tropicamide 1 % was used to dilate the pupils cycloplegia. Tropicamide is a drug often of 100 eyes of 52 consecutive patients who favoured because of its short duration of required fundoscopy during attendance at the action and relatively greater mydriatic than general ophthalmology outpatient clinic. The cycloplegic effect. mean patient age was 38 years (range 6-84 Concern is often expressed with regard to years). Prior to dilatation retinoscopy was adverse effects of pupil dilatation on vision carried out and the uncorrected and best cor which might affect patients' ability to travel rected visual acuities were recorded using a home safely or to return to work. -

Afe Mydriasis
Br J Ophthalmol: first published as 10.1136/bjo.54.10.690 on 1 October 1970. Downloaded from Brit. J. Ophthal. (1970) 54, 690 afe mydriasis R. MAPSTONE From the Department of Ophthalmology, (Jniversity of Liverpool, St. Paul's Eye Hospital, Liverpool Routine examination of the fundus requires a dilated pupil. If a cycloplegic drug is used the three major disadvantages are: paralysis of accommodation, an increase in intraocular pressure produced by a mechanism not involving angle-closure (Schimek and Lieberman, I96I; Christensen and Pearce, I963), and a frank attack of acute closed-angle glaucoma. With a sympathomimetic drug only the last complication is of consequence. After the pupil has been dilated it can be either left as such, inviting potential disaster in an eye with a narrow angle, or a parasympathomimetic drug can be instilled, which, if successful in producing miosis, causes a tonic pupil and spasm of accommodation. Neither com- bination is therefore satisfactory. copyright. The purpose of this paper is to describe a mydriatic - miotic combination in which the dangers and disadvantages are reduced to a minimum and to illustrate the properties of the miotic used. Material and methods One drop of thymoxamine (a sympathetic alpha inhibitor: Birmingham and Szolcsfnyi, 1965) was http://bjo.bmj.com/ instilled into the right conjunctival sac of ten subjects. Photographs of both eyes were then taken at a fixed distance, at hourly intervals for 6 hours and again at 24 hours. Each subject received on separate occasions o. I, 0.5, and i o per cent. concentrations. Subsequently, the slides were pro- jected and the horizontal pupil diameter of the eye receiving thymoxamine was expressed as a percentage of the opposite normal eye. -

Ipratropium-Bromide-Induced Acute Anisocoria in the Intensive Care Setting Due to Ill-Fitting Face Masks
Joshua O Benditt MD, Section Editor Teaching Case of the Month Ipratropium-Bromide-Induced Acute Anisocoria in the Intensive Care Setting Due to Ill-Fitting Face Masks Rebecca A Bisquerra MD, Gregory H Botz MD, and Joseph L Nates MD Introduction Case Report 1 Anisocoria, or unequal pupil size, may be an early sign A 78-year-old woman with acute myelogeous leukemia, of an impending neurologic emergency in any patient.1 atrial fibrillation, and coronary-artery disease was admit- Acute unilateral mydriasis is often suggestive of a life- ted to our ICU with respiratory insufficiency following threatening condition affecting cranial nerve function, such induction chemotherapy. Noninvasive positive-pressure as tumor compression, intracranial hypertension with im- ventilation delivered via oronasal mask was used to sup- pending uncal herniation, expanding intracranial aneurysm, port oxygenation and alveolar ventilation. Nebulized le- or hemorrhage. Benign mydriasis can be due to prior trauma, valbuterol and ipratropium bromide were administered for medication effects, and congenital abnormalities. Deter- wheezing noted on physical examination. On ICU day 2 mining the cause of anisocoria can be challenging in crit- (hospital day 18), the patient had an acute mental-status ical care settings because patients often are sedated, par- change. A noncontrast head CT revealed no mass effect, alyzed, intubated, or have a baseline altered mental status nor intracranial hemorrhage. On ICU day 4, a magnetic that makes full neurologic examination difficult. -

Ocular Emergencies – Chemical Burns (Alkali) – Temporal Arteritis Victoria M
Acute Conditions Emergency – Retinal Artery Occlusion Ocular Emergencies – Chemical burns (alkali) – Temporal Arteritis Victoria M. Romaniuk, MD – Orbital compartment syndrome Clinical Instructor of Emergency Medicine University of Maryland School of Medicine Very Urgent – Perforation – Rupture – Acute glaucoma Acute Conditions Non Traumatic Red Eye Possible Causes Urgent – Orbital cellulitis Conjunctivitis – Orbital injury Corneal – Corneal ulcer Inflammation/Infection – Corneal abrasion Iritis (Uveitis) – Hyphema Acute glaucoma – Intraocular foreign body – Retinal detachment – Macular edema Non Traumatic Red Eye Anatomy Conjunctivitis Discharge type Etiology Purulent Bacterial Serous or clear Viral Stringy, white Allergic Pre-auricular lymph node enlargement: Viral 1 Non Traumatic Red Eye Non Traumatic Red Eye Bacterial Conjunctivitis Bacterial Conjunctivitis – Mucopurulent d/c – Staph, strep – Visual acuity good – Treatment: Antibiotic ointment or drops (Erythromycin, fluoroquinolone) Non Traumatic Red Eye Non Traumatic Red Eye Bacterial Conjunctivitis Gonococcal Conjunctivitis Gonococcal – Copious discharge – Pre-auricular adenopathy – Neonates: Bilateral, 3-5 days post vaginal delivery – Treatment: IV Penicillin – Can cause perforation Non Traumatic Red Eye Non Traumatic Red Eye Bacterial Conjunctivitis Viral Conjunctivitis Chlamydia (Inclusion) – Adenovirus – Lymphoid follicles – Frequently bilateral – Neonates: 5-14 days post vaginal delivery – Associated with URI – Adults: recurring symptoms, – Treatment: supportive ocular -

Dilating Dangerous Pupils R
Br J Ophthalmol: first published as 10.1136/bjo.61.8.517 on 1 August 1977. Downloaded from British Journal of Ophthalmology, 1977, 61, 517-524 Dilating dangerous pupils R. MAPSTONE From St. Paul's Eye Hospital, Liverpool SUMMARY Altogether 85 eyes from patients at risk to the development of closed-angle glaucoma were dilated with either parasympatholytic or sympathomimetic drugs. Of 21 eyes dilated with cyclopentolate i %, 9 developed angle closure and a significantly raised pressure at some stage during dilatation and subsequent miosis. Of 58 eyes dilated with tropicamide 1 %, 19 developed angle closure and a significantly raised pressure during dilatation. Treatment with intravenous acetazolamide and pilocarpine rapidly returned pressure to normal levels. Six eyes that had previously had a positive provocative test with simultaneous pilocarpine and phenylephrine were safely dilated with phenylephrine alone. Subsequent miosis with pilocarpine produced closed-angle glaucoma in all eyes. The significance of these observations is explained and discussed, and it is suggested that high- risk eyes should never be dilated with cyclopentolate. Tropicamide is safe if elementary precautions are observed. Safest of all, however, is phenylephrine-induced mydriasis and subsequent miosis with thymoxamine drops I %. copyright. Pupillary dilatation is potentially dangerous, since a Material and methods variable proportion of eyes at risk to closed-angle glaucoma develop a rise in pressure of 8 mmHg or (1) Twenty-one eyes at risk to the development of more. A much smaller percentage of narrow-angle closed-angle glaucoma (because the contralateral eyes with no relevant history will respond similarly. eye had had an episode of acute closed-angle Given a particular eye with a narrow angle, how can glaucoma) were on no treatment.