Adrenergic Agents Adrenergic Agonists Directly Stimulate the Α-Adrenergic Receptors of the Iris Dilator Muscle, Resulting in Mydriasis Without Cycloplegia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Non-Steroidal Drug-Induced Glaucoma MR Razeghinejad Et Al 972
Eye (2011) 25, 971–980 & 2011 Macmillan Publishers Limited All rights reserved 0950-222X/11 www.nature.com/eye 1,2 1 1 Non-steroidal drug- MR Razeghinejad , MJ Pro and LJ Katz REVIEW induced glaucoma Abstract vision. The majority of drugs listed as contraindicated in glaucoma are concerned with Numerous systemically used drugs are CAG. These medications may incite an attack in involved in drug-induced glaucoma. Most those individuals with narrow iridocorneal reported cases of non-steroidal drug-induced angle.3 At least one-third of acute closed-angle glaucoma are closed-angle glaucoma (CAG). glaucoma (ACAG) cases are related to an Indeed, many routinely used drugs that have over-the-counter or prescription drug.1 Prevalence sympathomimetic or parasympatholytic of narrow angles in whites from the Framingham properties can cause pupillary block CAG in study was 3.8%. Narrow angles are more individuals with narrow iridocorneal angle. The resulting acute glaucoma occurs much common in the Asian population. A study of a more commonly unilaterally and only rarely Vietnamese population estimated a prevalence 4 bilaterally. CAG secondary to sulfa drugs is a of occludable angles at 8.5%. The reported bilateral non-pupillary block type and is due prevalence of elevated IOP months to years to forward movement of iris–lens diaphragm, after controlling ACAG with laser iridotomy 5,6 which occurs in individuals with narrow or ranges from 24 to 72%. Additionally, a open iridocorneal angle. A few agents, significant decrease in retinal nerve fiber layer including antineoplastics, may induce thickness and an increase in the cup/disc ratio open-angle glaucoma. -

M100907, a Serotonin 5-HT2A Receptor Antagonist and Putative Antipsychotic, Blocks Dizocilpine-Induced Prepulse Inhibition Defic
M100907, a Serotonin 5-HT2A Receptor Antagonist and Putative Antipsychotic, Blocks Dizocilpine-Induced Prepulse Inhibition Deficits in Sprague–Dawley and Wistar Rats Geoffrey B. Varty, Ph.D., Vaishali P. Bakshi, Ph.D., and Mark A. Geyer, Ph.D. a In a recent study using Wistar rats, the serotonergic 5-HT2 1 receptor agonist cirazoline disrupts PPI. As risperidone a receptor antagonists ketanserin and risperidone reduced the and M100907 have affinity at the 1 receptor, a final study disruptive effects of the noncompetitive N-methyl-D- examined whether M100907 would block the effects of aspartate (NMDA) antagonist dizocilpine on prepulse cirazoline on PPI. Risperidone partially, but inhibition (PPI), suggesting that there is an interaction nonsignificantly, reduced the effects of dizocilpine in Wistar between serotonin and glutamate in the modulation of PPI. rats, although this effect was smaller than previously In contrast, studies using the noncompetitive NMDA reported. Consistent with previous studies, risperidone did antagonist phencyclidine (PCP) in Sprague–Dawley rats not alter the effects of dizocilpine in Sprague–Dawley rats. found no effect with 5-HT2 antagonists. To test the hypothesis Most importantly, M100907 pretreatment fully blocked the that strain differences might explain the discrepancy in effect of dizocilpine in both strains; whereas SDZ SER 082 these findings, risperidone was tested for its ability to had no effect. M100907 had no influence on PPI by itself reduce the PPI-disruptive effects of dizocilpine in Wistar and did not reduce the effects of cirazoline on PPI. These and Sprague–Dawley rats. Furthermore, to determine studies confirm the suggestion that serotonin and glutamate which serotonergic receptor subtype may mediate this effect, interact in modulating PPI and indicate that the 5-HT2A the 5-HT2A receptor antagonist M100907 (formerly MDL receptor subtype mediates this interaction. -

Abcd (Ipratropium Bromide and Albuterol Sulfate) Inhalation Aerosol
ATTENTION PHARMACIST: Detach “Patient’s Instructions for Use” from package insert and dispense with the product. Combivent® abcd (ipratropium bromide and albuterol sulfate) Inhalation Aerosol Bronchodilator Aerosol For Oral Inhalation Only Rx only Prescribing Information DESCRIPTION COMBIVENT Inhalation Aerosol is a combination of ipratropium bromide (as the monohydrate) and albuterol sulfate. Ipratropium bromide is an anticholinergic bronchodilator chemically described as 8-azoniabicyclo[3.2.1] octane, 3-(3-hydroxy-1-oxo-2-phenylpropoxy)-8-methyl 8-(1-methylethyl)-, bromide monohydrate, (3-endo, 8-syn)-: a synthetic quaternary ammonium compound chemically related to atropine. Ipratropium bromide is a white to off-white crystalline substance, freely soluble in water and methanol, sparingly soluble in ethanol, and insoluble in lipophilic solvents such as ether, chloroform, and fluorocarbons. The structural formula is: + N OH Br . H O H 2 O O C20H30BrNO3•H2O ipratropium bromide Mol. Wt. 430.4 Albuterol sulfate, chemically known as (1,3-benzenedimethanol, α'-[[(1,1dimethylethyl) amino] methyl]-4-hydroxy, sulfate (2:1)(salt), (±)- is a relatively selective beta2-adrenergic bronchodilator. Albuterol is the official generic name in the United States. The World Health Organization recommended name for the drug is salbutamol. Albuterol sulfate is a white to off-white crystalline powder, freely soluble in water and slightly soluble in alcohol, chloroform, and ether. The structural formula is: Reference ID: 2927161 OH NH * . H2SO4 OH OH 2 (C13H21NO3)2•H2SO4 albuterol sulfate Mol. Wt. 576.7 Combivent® (ipratropium bromide and albuterol sulfate) Inhalation Aerosol contains a microcrystalline suspension of ipratropium bromide and albuterol sulfate in a pressurized metered-dose aerosol unit for oral inhalation administration. -

Covalent Agonists for Studying G Protein-Coupled Receptor Activation
Covalent agonists for studying G protein-coupled receptor activation Dietmar Weicherta, Andrew C. Kruseb, Aashish Manglikb, Christine Hillera, Cheng Zhangb, Harald Hübnera, Brian K. Kobilkab,1, and Peter Gmeinera,1 aDepartment of Chemistry and Pharmacy, Friedrich Alexander University, 91052 Erlangen, Germany; and bDepartment of Molecular and Cellular Physiology, Stanford University School of Medicine, Stanford, CA 94305 Contributed by Brian K. Kobilka, June 6, 2014 (sent for review April 21, 2014) Structural studies on G protein-coupled receptors (GPCRs) provide Disulfide-based cross-linking approaches (17, 18) offer important insights into the architecture and function of these the advantage that the covalent binding of disulfide-containing important drug targets. However, the crystallization of GPCRs in compounds is chemoselective for cysteine and enforced by the active states is particularly challenging, requiring the formation of affinity of the ligand-pharmacophore rather than by the elec- stable and conformationally homogeneous ligand-receptor com- trophilicity of the cross-linking function (19). We refer to the plexes. Native hormones, neurotransmitters, and synthetic ago- described ligands as covalent rather than irreversible agonists nists that bind with low affinity are ineffective at stabilizing an because cleavage may be promoted by reducing agents and the active state for crystallogenesis. To promote structural studies on disulfide transfer process is a reversible chemical reaction the pharmacologically highly relevant class -

The Adrenergic Control of Lower Esophageal Sphincter Function: an EXPERIMENTAL MODEL of DENERVATION SUPERSENSITIVITY
The Adrenergic Control of Lower Esophageal Sphincter Function: AN EXPERIMENTAL MODEL OF DENERVATION SUPERSENSITIVITY Anthony J. DiMarino, Sidney Cohen J Clin Invest. 1973;52(9):2264-2271. https://doi.org/10.1172/JCI107413. To evaluate the adrenergic regulation of lower esophageal sphincter (LES) function, LES pressure, LES relaxation during swallowing, and blood pressure were measured in the anesthetized opossum, Didelphis virginiana, during intravenous administration of alpha and beta adrenergic agonists and antagonists. Studies were done in controls and animals adrenergically denervated with 6-hydroxydopamine. Alpha adrenergic agonists (norepinephrine, phenylephrine) increased LES pressure and blood pressure, whereas a beta adrenergic agonist (isoproterenol) decreased both pressures. Alpha adrenergic antagonism (phentolamine) reduced basal LES pressure by 38.3±3.8% (mean ±SEM) (P < 0.001). Beta adrenergic antagonism (propranolol) had no significant effect on either basal LES pressure or percent of LES relaxation with swallowing. After adrenergic denervation with 6-hydroxydopamine, basal LES pressure was reduced by 22.5±5.3% (P < 0.025) but LES relaxation during swallowing was unaltered. In denervated animals, both LES pressure and blood pressure dose response curves showed characteristics of denervation supersensitivity to alpha but not to beta adrenergic agonists. These studies suggest: (a) a significant portion of basal LES pressure is dependent upon alpha adrenergic stimulation; (b) LES relaxation during swallowing is not an adrenergically mediated response; c( ) the LES pressure response to alpha adrenergic agonists after 6-hydroxydopamine may serve as a model of denervation supersensitivity in the gastrointestinal tract. Find the latest version: https://jci.me/107413/pdf The Adrenergic Control of Lower Esophageal Sphincter Function AN EXPERIMENTAL MODEL OF DENERVATION SUPERSENSITIVITY ANTHoNY J. -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -

Update on Surgical Management of Corneal Ulceration and Perforation
Romanian Journal of Ophthalmology, Volume 63, Issue 2, April-June 2019. pp:166-173 GENERAL ARTICLE Update on surgical management of corneal ulceration and perforation Stamate Alina-Cristina* **, Tătaru Călin Petru* ***, Zemba Mihail* **** *Department of Ophthalmology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania **Arena Med Clinic, Bucharest, Romania ***Clinical Hospital of Ophthalmologic Emergencies, Bucharest, Romania ****Department of Ophthalmology, “Dr. Carol Davila” Central Military Emergency University Hospital, Bucharest, Romania Correspondence to: Stamate Alina-Cristina, MD, Arena Med Clinic, Bucharest, 68 Basarabia Boulevard, Ap. 1, District 2, Bucharest, Romania, Mobile phone: +40737 027 067, E-mail: [email protected] Accepted: May 28th, 2019 Abstract Corneal ulcerations are a medical emergency, and in recalcitrant cases, leading to perforation, a surgical ophthalmological emergency. The urgency of the treatment is dictated by the necessity of preventing complications that can lead to serious ocular morbidities. Medical treatment represents the first therapeutic approach and is a defining step in the further management of a patient with corneal ulceration. Multiple surgical strategies are available, but the option depends on the etiology and parameters of the ulceration: size, depth, and location. Keywords: corneal ulceration, corneal perforation, tissue adhesives, cross-linking, amniotic membrane, conjunctival flap, keratoplasty Introduction reepithelialization by using preservative-free lubricants, -

Pharmacology of Ophthalmic Agents
Ophthalmic Pharmacology Richard Alan Lewis M.D., M.S., PHARMACOLOGY FOPS PHARMACOKINETICS OF Professor, Departments of Ophthalmology, • The study of the absorption, OPHTHALMIC Medicine, Pediatrics, and Molecular distribution, metabolism, AGENTS and Human Genetics and excretion of a drug or and the National School of Tropical agent Introduction and Review Medicine Houston, Texas PHARMACOKINETICS Factors Affecting Drug Penetration Factors Affecting Drug Penetration into Ocular Tissues • A drug can be delivered to ocular tissue: into Ocular Tissues – Locally: • Drug concentration and solubility: The higher the concentration the better the penetration, • Surfactants: The preservatives in ocular • Eye drop but limited by reflex tearing. preparations alter cell membrane in the cornea • Ointment and increase drug permeability, e.g., • Viscosity: Addition of methylcellulose and benzalkonium and thiomersal • Periocular injection polyvinyl alcohol increases drug penetration by • pH: The normal tear pH is 7.4; if the drug pH is • Intraocular injection increasing the contact time with the cornea and altering corneal epithelium. much different, it will cause reflex tearing. – Systemically: • Lipid solubility: Because of the lipid rich • Drug tonicity: When an alkaloid drug is put in • Orally environment of the epithelial cell membranes, relatively alkaloid medium, the proportion of the uncharged form will increase, thus more • IM the higher lipid solubility, the more the penetration. • IV penetration. FLUORESCEIN FLUORESCEIN Chemistry Dosage ● C20H1205, brown crystal ● Adults: 500-750 mg IV ● M.W. 322.3 e.g., 3 cc 25% solution ● Peak absorption 485-500 nm. 5 cc 10% solution ● Peak emission 520-530 nm. ● Children: 1.5-2.5 mg/kg IV Richard Alan Lewis, M.D., M.S. -

Pharmacological Approach to Sleep Disturbances in Autism Spectrum Disorders with Psychiatric Comorbidities: a Literature Review
medical sciences Review Pharmacological Approach to Sleep Disturbances in Autism Spectrum Disorders with Psychiatric Comorbidities: A Literature Review Sachin Relia 1,* and Vijayabharathi Ekambaram 2,* 1 Department of Psychiatry, University of Tennessee Health Sciences Center, 920, Madison Avenue, Suite 200, Memphis, TN 38105, USA 2 Department of Psychiatry, University of Oklahoma Health Sciences Center, 920, Stanton L Young Blvd, Oklahoma City, OK 73104, USA * Correspondence: [email protected] (S.R.); [email protected] (V.E.); Tel.: +1-901-448-4266 (S.R.); +1-405-271-5251 (V.E.); Fax: +1-901-297-6337 (S.R.); +1-405-271-3808 (V.E.) Received: 15 August 2018; Accepted: 17 October 2018; Published: 25 October 2018 Abstract: Autism is a developmental disability that can cause significant emotional, social and behavioral dysfunction. Sleep disorders co-occur in approximately half of the patients with autism spectrum disorder (ASD). Sleep problems in individuals with ASD have also been associated with poor social interaction, increased stereotypy, problems in communication, and overall autistic behavior. Behavioral interventions are considered a primary modality of treatment. There is limited evidence for psychopharmacological treatments in autism; however, these are frequently prescribed. Melatonin, antipsychotics, antidepressants, and α agonists have generally been used with melatonin, having a relatively large body of evidence. Further research and information are needed to guide and individualize treatment for this population group. Keywords: autism spectrum disorder; sleep disorders in ASD; medications for sleep disorders in ASD; comorbidities in ASD 1. Introduction Autism is a developmental disability that can cause significant emotional, social, and behavioral dysfunction. According to the Diagnostic and Statistical Manual (DSM-V) classification [1], autism spectrum disorder (ASD) is characterized by persistent deficits in domains of social communication, social interaction, restricted and repetitive patterns of behavior, interests, or activities. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -
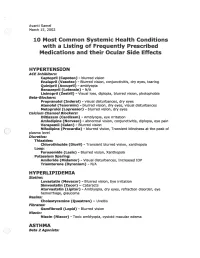
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)-