Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

URGENT/EMERGENT When to Refer Financial Disclosure
URGENT/EMERGENT When to Refer Financial Disclosure Speaker, Amy Eston, M.D. has a financial interest/agreement or affiliation with Lansing Ophthalmology, where she is employed as a ophthalmologist. 58 yr old WF with 6 month history of decreased vision left eye. Ache behind the left eye for 2-3 months. Using husband’s contact lens solution made it feel better. Seen by two eye care professionals. Given glasses & told eye exam was normal. No past ocular history Medical history of depression Takes only aspirin and vitamins 20/20 OD 20/30 OS Eye Pressure 15 OD 16 OS – normal Dilated fundus exam & slit lamp were normal Pupillary exam was normal Extraocular movements were full Confrontation visual fields were full No red desaturation Color vision was slightly decreased but the same in both eyes Amsler grid testing was normal OCT disc – OD normal OS slight decreased RNFL OCT of the macula was normal Most common diagnoses: Dry Eye Optic Neuritis Treatment - copious amount of artificial tears. Return to recheck refraction Visual field testing Visual Field testing - Small defect in the right eye Large nasal defect in the left eye Visual Field - Right Hemianopsia. MRI which showed a subacute parietal and occipital lobe infarct. ANISOCORIA Size of the Pupil Constrictor muscles innervated by the Parasympathetic system & Dilating muscles innervated by the Sympathetic system The Sympathetic System Begins in the hypothalamus, travels through the brainstem. Then through the upper chest, up through the neck and to the eye. The Sympathetic System innervates Mueller’s muscle which helps to elevate the upper eyelid. -

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -
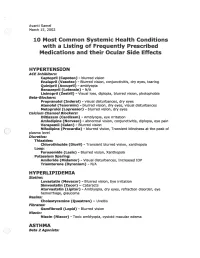
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Anisocoria in an Intubated Patient with COVID-19 Sam Myers ,1,2 Minak Bhalla,1 Rohit Jolly,3 Saurabh Jain3
Case report BMJ Case Rep: first published as 10.1136/bcr-2020-240003 on 22 July 2021. Downloaded from Anisocoria in an intubated patient with COVID-19 Sam Myers ,1,2 Minak Bhalla,1 Rohit Jolly,3 Saurabh Jain3 1Department of Ophthalmology, SUMMARY CASE PRESENTATION Whittington Health NHS Trust, The effects of COVID-19 on the eye are still widely A- 74- year old man was admitted to the hospital London, UK 2 unknown. We describe a case of a patient who was with a 2- week history of cough, fever and progres- UCL Medical School, University intubated and proned in the intensive care unit (ICU) sive shortness of breath. He had a background of College London, London, UK hypothyroidism, hypertension and benign pros- 3Department of Ophthalmology, for COVID-19 and developed unilateral anisocoria. Royal Free London NHS CT venogram excluded a cavernous sinus thrombosis. tate hypertrophy. His initial imaging and swab test Foundation Trust, London, UK MRI of the head showed microhaemorrhages in the confirmed COVID-19. The patient was placed midbrain where the pupil reflex nuclei are located. After on a trial of continuous positive airway pressure Correspondence to the patient was stepped down from ICU, intraocular to support his deteriorating oxygen saturation. Dr Sam Myers; pressure (IOP) was found to be raised in that eye. A However, after a week of supportive therapy, he sam. myers1@ nhs. net diagnosis of subacute closed angle glaucoma was made. was transferred to the ICU and was supported with It is important for clinicians to rule out thrombotic mechanical ventilation and proning. -

Miotic Adie's Pupils
Journal of Cll/lical Neuro-ophtllJllmology 9(1): 43-45, 1989. RilVen Press, Ltd., New York Miotic Adie's Pupils Michael L. Rosenberg, M.D. Two young adults, aged 24 and 31, had a long history of Adie's syndrome or, pupillotonia, is typically small, poorly reactive pupilS. There was no history of characterized by either unilaterally or bilaterally large pupils, and a review of old photographs confirmed enlarged pupils that are unresponsive to light (1). 10 and 5 years, respectively, of miosis. Both were found to have bilateral tonic pupils that were supersensitive to The diagnosis is made clinically by watching for a diluted pilocarpine. Although it is possible that they had tonic constriction to near stimulation followed by a an unusually early onset of bilateral Adie's syndrome tonic redilatation. with dilated pupils that was not noticed, it is suggested Two young adults are described who were noted that some patients might have primary miotic Adie's during routine examinations to have bilaterally mi pupils without ever passing through a mydriatic phase. Key Words: Adie's syndrome-Argyll Robertson pu otic pupils that were thought to be fixed to light. pils-Miosis. They were both referred for the evaluation of Ar gyll Robertson pupils. Evaluation revealed bilat eral tonic reactions to near stimulation in both pa tients, typical of Adie's tonic pupilS. The diagnosis of parasympathetic denervation was confirmed in both patients as their pupils constricted with di luted pilocarpine. The cases reinforce the principle that any pupil regardless of size should be evalu ated for the possibility of pupillotonia. -

Changes in Intraocular Pressure After Pharmacologic Pupil Dilation
UCLA UCLA Previously Published Works Title Changes in intraocular pressure after pharmacologic pupil dilation Permalink https://escholarship.org/uc/item/7nz7c380 Journal BMC Ophthalmology, 12(1) ISSN 1471-2415 Authors Kim, Joon Park, Ki Han, So et al. Publication Date 2012-09-27 DOI http://dx.doi.org/10.1186/1471-2415-12-53 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Kim et al. BMC Ophthalmology 2012, 12:53 http://www.biomedcentral.com/1471-2415/12/53 RESEARCH ARTICLE Open Access Changes in intraocular pressure after pharmacologic pupil dilation Joon Mo Kim1, Ki Ho Park2*, So Young Han1, Kwan Soo Kim1, Dong Myung Kim2, Tae Woo Kim3 and Joseph Caprioli4 Abstract Background: Intraocular pressure (IOP) may vary according to the change of ocular conditions. In this study, we want to assess the effect and mechanism of pupil dilation on IOP in normal subjects. Methods: We prospectively evaluated 32 eyes of 32 patients (age; 61.7 ± 8.2 years) with normal open angles under diurnal IOP. IOP was measured every two hours from 9 AM to 11 PM for one day to establish baseline values and was measured again for one day to assess the differences after dilation. To induce dilation, we administered 2.5% phenylephrine and 1% tropicamide every 5 minutes from 8:30 AM to 8:45 AM and for every two hours from 11 AM to 9 PM to keep the pupil dilated. Diurnal IOP, biometry, Visante OCT, and laser flare photometry were measured before and after dilation. Results: We observed a significant increase in IOP after dilation, 1.85 ± 2.01 mmHg (p = 0.002). -

Anisocoria Greater in the Dark: It’S Not Just All About Horner Pupil
RESIDENT & FELLOW SECTION Pearls & Oy-sters: Anisocoria Greater in the Dark: It’s Not Just All About Horner Pupil Emily Witsberger, MD, Sasha A. Mansukhani, MBBS, John J. Chen, MD, PhD, and M. Tariq Bhatti, MD Correspondence Dr. Bhatti Neurology 2021;96:719-722. doi:10.1212/WNL.0000000000011221 ® Bhatti.Muhammad@ mayo.edu Pearls MORE ONLINE c An initial step in the evaluation of anisocoria is assessing the pupillary light reflex. If a pupil Video is not responsive to light, then the near pupillary reflex needs to be evaluated. Unilateral light-near pupil dissociation occurs due to a lesion of the ciliary ganglion, postganglionic parasympathetic pathway, retina, or optic nerve. Oy-sters c In addition to a Horner pupil, anisocoria can be more pronounced in the dark with physiologic anisocoria, miosis due to posterior iris synechiae, pharmacologic miosis due to a parasympathomimetic agent (i.e., pilocarpine), traumatic miosis, iris ischemia, and a chronic Adie tonic pupil. c Adie tonic pupil most frequently presents with a mydriatic pupil, light-near dissociation, vermiform iris sphincter muscle movement, and anisocoria greater in the light. However, a chronic Adie tonic pupil may be characterized by a miotic pupil, light-near dissociation, and anisocoria that is greater in the dark. An asymptomatic 65-year-old patient with no prior ocular surgery but a history of hypertension, hyperlipidemia, and hypothyroidism was noted to have a left miotic pupil during a routine ophthalmic examination. The anisocoria was noted to be greater in the dark and was interpreted as a left Horner pupil. No pharmacologic testing was performed. -

Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia
CASE REPORT Print ISSN 1738-6586 / On-line ISSN 2005-5013 J Clin Neurol 2014 Open Access Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia Fabrice C. Deprez,a Julie Coulier,b Denis Rommel,a Antonella Boschib aDepartments of Radiology and bOphthalmology, Cliniques Universitaires Saint-Luc, UCL, Brussels, Belgium BackgroundzzHorner syndrome (HS), also known as Claude-Bernard-Horner syndrome or Received August 5, 2013 oculosympathetic palsy, comprises ipsilateral ptosis, miosis, and facial anhidrosis. Revised April 15, 2014 Accepted April 21, 2014 Case ReportzzWe report herein the case of a 67-year-old man who presented with congenital HS associated with ipsilateral hypoplasia of the internal carotid artery (ICA), as revealed by Correspondence heterochromia iridis and confirmed by computed tomography (CT). Fabrice C. Deprez, MD Department of Radiology, ConclusionszzCT evaluation of the skull base is essential to establish this diagnosis and dis- Cliniques Universitaires Saint-Luc, tinguish aplasia from agenesis/hypoplasia (by the absence or hypoplasia of the carotid canal) or UCL, Avenue Hippocrate 10, from acquired ICA obstruction as demonstrated by angiographic CT. 1200 Woluwe-Saint-Lambert, J Clin Neurol 2014 Belgium Tel +32.472.93.34.80 Key Wordszzcongenital horner syndrome, internal carotid artery agenesis, Fax +32.81.42.35.05 heterochromia iridis, computed tomography. E-mail [email protected] Introduction spindly left ICA, which was misinterpreted as ICA thrombosis (Fig. 1). The left anterior cerebral artery and MCA were sup- Horner syndrome (HS), also known as Claude-Bernard-Horn- plied by a large posterior communicating artery from the bas- er syndrome or oculosympathetic palsy, comprises ipsilateral ilar artery. -

Pupil Dilatation with Tropicamide. the Effects on Acuity, Accommodation and Refraction
Eye (1989) 3, 845-848 Pupil Dilatation with Tropicamide. The Effects on Acuity, Accommodation and Refraction D. M. I. MONTGOMERY! and C. J. MACEWANZ Glasgow and Dundee. Summary The effect of pupil dilatation with tropicamide 1 % on visual acuity and accommo dation was assessed in 100 eyes of 52 consecutive patients attending the general ophthalmic outpatient clinic. Snellen visual acuity remained unchanged in 55 eyes and deteriorated by one line in 41 eyes. The remaining four eyes deteriorated by two lines. Tropicamide gave rise to a reduction in the amplitude of accommodation which tended to vary inversely with the age of the patient. However, all patients who wore reading glasses for presbyopia were still able to read when their pupils had been dilated. Many drugs are used routinely in ophthalmic acuity and accommodation in such a practice to dilate the pupil for adequate exam population. ination of the ocular fundus. Selection may be based on the speed of onset and duration of action of the drug as well as on the presence Materials and methods and severity of any unwanted effects such as Tropicamide 1 % was used to dilate the pupils cycloplegia. Tropicamide is a drug often of 100 eyes of 52 consecutive patients who favoured because of its short duration of required fundoscopy during attendance at the action and relatively greater mydriatic than general ophthalmology outpatient clinic. The cycloplegic effect. mean patient age was 38 years (range 6-84 Concern is often expressed with regard to years). Prior to dilatation retinoscopy was adverse effects of pupil dilatation on vision carried out and the uncorrected and best cor which might affect patients' ability to travel rected visual acuities were recorded using a home safely or to return to work. -

Marfan Syndrome: Jeffrey Welder MSIII, Erik L
Marfan Syndrome: Jeffrey Welder MSIII, Erik L. Nylen MSE, Thomas Oetting MS MD May 6, 2010 Chief Complaint: Decreased vision and glare in both eyes. History of Present Illness: A 28 year old woman with a history of Marfan syndrome presented to the comprehensive ophthalmology clinic reporting a progressive decrease in vision and worsening glare in both eyes. She had been seen by ophthalmologists in the past, and had been told that her crystalline lenses were subluxed in both eyes. She had not had problems with her vision until recent months. Past Medical History: Marfan syndrome with aortic stenosis followed by cardiology Medications: Oral beta blocker Family History: No known family members with Marfan Syndrome. Grandmother with glaucoma. Social History: The patient is a graduate student. Ocular Exam: External Exam normal. VA (with correction): OD 20/40 OS 20/50 Current glasses: OD: 6.75+ 5.00 x 135 OS: -5.25 + 4.25 x 60 Pupils: No anisocoria and no relative afferent pupillary defect Motility: Ocular motility full OU. Anterior segment exam: Inferiorly subluxed lenses OU (figure 1 and 2). The angle was deep OU and there was no lens apposition to the cornea in either eye. Dilated funduscopic exam: Posterior segment was normal OU with no peripheral retinal degeneration . Course: The patient’s subluxed lenses led to poor vision from peripheral lenticular irregular astigmatism and glare. She was taken to the operating room where her relatively clear lenses were removed and iris sutured intraocular lenses were placed. The surgical video for one of the eyes may be viewed at http://www.facebook.com/video/video.php?v=153379281140 Page | 1 Figure One: Note the inferiorly subluxed lens.