Unilateral Mydriasis in a Child with A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

URGENT/EMERGENT When to Refer Financial Disclosure
URGENT/EMERGENT When to Refer Financial Disclosure Speaker, Amy Eston, M.D. has a financial interest/agreement or affiliation with Lansing Ophthalmology, where she is employed as a ophthalmologist. 58 yr old WF with 6 month history of decreased vision left eye. Ache behind the left eye for 2-3 months. Using husband’s contact lens solution made it feel better. Seen by two eye care professionals. Given glasses & told eye exam was normal. No past ocular history Medical history of depression Takes only aspirin and vitamins 20/20 OD 20/30 OS Eye Pressure 15 OD 16 OS – normal Dilated fundus exam & slit lamp were normal Pupillary exam was normal Extraocular movements were full Confrontation visual fields were full No red desaturation Color vision was slightly decreased but the same in both eyes Amsler grid testing was normal OCT disc – OD normal OS slight decreased RNFL OCT of the macula was normal Most common diagnoses: Dry Eye Optic Neuritis Treatment - copious amount of artificial tears. Return to recheck refraction Visual field testing Visual Field testing - Small defect in the right eye Large nasal defect in the left eye Visual Field - Right Hemianopsia. MRI which showed a subacute parietal and occipital lobe infarct. ANISOCORIA Size of the Pupil Constrictor muscles innervated by the Parasympathetic system & Dilating muscles innervated by the Sympathetic system The Sympathetic System Begins in the hypothalamus, travels through the brainstem. Then through the upper chest, up through the neck and to the eye. The Sympathetic System innervates Mueller’s muscle which helps to elevate the upper eyelid. -

Chlorpromazine-Induced Cataract and Corneal Pigmentation
Case Report Chlorpromazine-induced cataract and corneal pigmentation Chlorpromazine (CPZ) is a low-potency neuroleptic used bution was symmetrical in both eyes. Two independent clini- in the treatment of various psychiatric disorders.1 Chlorpro- cians documented the condition. The pupils were dilated with mazine-induced cataract and corneal pigmentation was first 1% tropicamide for retinoscopy. A dilatation of only 4 mm could described by Greiner & Berry in 1964.2 The prevalence in pa- be achieved. Fundus examination by indirect ophthalmoscopy tients treated over time with large doses of CPZ therapy, ranges was normal. Systemic examination was normal; apart from a from 15% to 74%. Though other low-potency neuroleptics like few extrapyramidal symptoms there were no other side-ef- thioridazine and fluphenazine have been reported to cause fects of CPZ, including skin discoloration. Investigations in- pigmentary changes, characteristic corneal and lenticular pig- cluding liver function tests and peripheral smear were nor- mentation is predominantly if not exclusively a side-effect of mal. With subjective correction, the patient’s vision improved CPZ. We report a case of a 45-year-old female with ocular to 6/9. With the psychiatrist’s consultation, CPZ was substi- effects due to long-term CPZ therapy for bipolar disease. tuted with trifluoperazine. Case report Discussion A 45-year-old female had been taking treatment for manic- Chlorpromazine is an aliphatic phenothiazine used in all depressive psychosis with chlorpromazine 300 mg per day for types of psychosis, especially schizophrenia. The adverse ef- 25 years. In addition, she was found to have received lithium fects include drowsiness, lethargy, postural hypotension, an- 300 mg and haloperidol 5 mg, both twice daily for florid psy- ticholinergic side-effects, infertility and extrapyramidal symp- chotic symptoms. -

Non-Steroidal Drug-Induced Glaucoma MR Razeghinejad Et Al 972
Eye (2011) 25, 971–980 & 2011 Macmillan Publishers Limited All rights reserved 0950-222X/11 www.nature.com/eye 1,2 1 1 Non-steroidal drug- MR Razeghinejad , MJ Pro and LJ Katz REVIEW induced glaucoma Abstract vision. The majority of drugs listed as contraindicated in glaucoma are concerned with Numerous systemically used drugs are CAG. These medications may incite an attack in involved in drug-induced glaucoma. Most those individuals with narrow iridocorneal reported cases of non-steroidal drug-induced angle.3 At least one-third of acute closed-angle glaucoma are closed-angle glaucoma (CAG). glaucoma (ACAG) cases are related to an Indeed, many routinely used drugs that have over-the-counter or prescription drug.1 Prevalence sympathomimetic or parasympatholytic of narrow angles in whites from the Framingham properties can cause pupillary block CAG in study was 3.8%. Narrow angles are more individuals with narrow iridocorneal angle. The resulting acute glaucoma occurs much common in the Asian population. A study of a more commonly unilaterally and only rarely Vietnamese population estimated a prevalence 4 bilaterally. CAG secondary to sulfa drugs is a of occludable angles at 8.5%. The reported bilateral non-pupillary block type and is due prevalence of elevated IOP months to years to forward movement of iris–lens diaphragm, after controlling ACAG with laser iridotomy 5,6 which occurs in individuals with narrow or ranges from 24 to 72%. Additionally, a open iridocorneal angle. A few agents, significant decrease in retinal nerve fiber layer including antineoplastics, may induce thickness and an increase in the cup/disc ratio open-angle glaucoma. -

Acepromazine and Chlorpromazine As Pharmaceutical-Grade Alternatives to Chlorprothixene for Pupillary Light Reflex Imaging in Mice
Journal of the American Association for Laboratory Animal Science Vol 59, No 2 Copyright 2020 March 2020 by the American Association for Laboratory Animal Science Pages 197–203 Acepromazine and Chlorpromazine as Pharmaceutical-grade Alternatives to Chlorprothixene for Pupillary Light Reflex Imaging in Mice Samantha S Eckley,1 Jason S Villano,1 Nora S Kuo,1 and Kwoon Y Wong2,* Studies of visual responses in isoflurane-anesthetized mice often use the sedative chlorprothixene to decrease the amount of isoflurane used because excessive isoflurane could adversely affect light-evoked responses. However, data are not available to justify the use of this nonpharmaceutical-grade chemical. The current study tested whether pharmaceutical-grade sedatives would be appropriate alternatives for imaging pupillary light reflexes. Male 15-wk-old mice were injected intraperitoneally with 1 mg/kg chlorprothixene, 5 mg/kg acepromazine, 10 mg/kg chlorpromazine, or saline. After anesthetic induction, anes- thesia maintenance used 0.5% and 1% isoflurane for sedative- and saline-injected mice, respectively. A photostimulus (16.0 log photons cm−2 s−1; 470 nm) was presented to the right eye for 20 min, during which the left eye was imaged for consensual pupillary constriction and involuntary pupil drift. Time to immobilization, loss of righting reflex, physiologic parameters, gain of righting reflex, and degree of recovery were assessed also. The sedative groups were statistically indistinguishable for all measures. By contrast, pupillary drift occurred far more often in saline-treated mice than in the sedative groups. Fur- thermore, saline-treated mice took longer to reach maximal pupil constriction than all sedative groups and had lower heart rates compared with chlorpromazine- and chlorprothixene-sedated mice. -

Tropicamide Tropicamide Eye Drops
Minims® Tropicamide Tropicamide Eye Drops Consumer Medicine Information Tell your doctor if you have or What is in this leaflet Before you use Minims have had any of the following Tropicamide This leaflet answers some common medical conditions: questions about Minims * glaucoma (high pressure in the Tropicamide, including how to use When you must not use it eye) the eye drops. * fast heartbeat or any heart Do not use Minims Tropicamide if It does not contain all the available condition or had heart surgery. you have an allergy to: information. It does not take the Tell your doctor if you are place of talking to your doctor or * any medicine containing pregnant or are breast-feeding. pharmacist. tropicamide Your doctor will discuss with you * any of the ingredients listed at the All medicines have benefits and the risks and benefits involved. risks. Your doctor has weighed the end of this leaflet. Tell your doctor if you wear risks of you using Minims Some of the symptoms of an allergic contact lenses. Tropicamide against the benefits they reaction may include: You should not wear contact lenses expect it will have for you. * shortness of breath while using this medicine. If you have any concerns about * wheezing or difficulty breathing using this medicine, ask your * swelling of the face, lips, tongue If you have not told your doctor doctor or pharmacist. about any of the above, tell or other parts of the body him/her before you start using Keep this leaflet with the medicine. * rash, itching or hives on the skin. -

Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Eye (2018) 32, 457–459 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2 2 2 Intermittent mydriasis PD Chamberlain , A Sadaka , S Berry CASE SERIES 1,2,3,4,5,6 associated with carotid and AG Lee vascular occlusion Abstract the literature as benign episodic pupillary dilation or BEUM. We report two patients with Purpose To describe two cases of 1 stereotyped, intermittent, neurologically acquired occlusive disease of the ipsilateral ICA Department of Ophthalmology, Blanton isolated, unilateral mydriasis in patients who developed multiple, stereotyped, neurologically isolated, transient episodes of Eye Institute, Houston with a history of acquired internal carotid Methodist Hospital, artery (ICA) occlusive disease on the mydriasis consistent with BEUM. We discuss the Houston, TX, USA ipsilateral side. possible mechanisms, differential diagnosis and 2 Patients Two patients with intermittent recommended evaluation for atypical cases for Department of episodic mydriasis. Ophthalmology, Baylor mydriasis. College of Medicine, Methods Case Series. Houston, TX, USA Results Case one: A 78-year-old man Case one 3 experienced 10 episodes of intermittent, Departments of Ophthalmology, Neurology, unilateral, and painless mydriasis in the left A 78-year-old man presented with 10 episodes of and Neurosurgery, Weill stereotyped, intermittent, unilateral, painless eye and had 100% occlusion of the left ICA Cornell Medical College, artery due to atherosclerotic disease. Case two: pupillary dilation of the left eye (OS) lasting New York, NY, USA A 26-year-old woman with history of migraine minutes to hours at a time without diplopia or fi 4Department of developed new painless, intermittent episodes ptosis. -

208151Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208151Orig1s000 SUMMARY REVIEW NDA 208151, ISOPTO Atropine (atropine sulfate ophthalmic solution) 1% Cycloplegia, Mydriasis, Penalization of the healthy eye in the treatment of amblyopia Division Director Summary Review Material Reviewed/Consulted OND Action Package, including: Names of discipline reviewers Medical Officer Review Wiley Chambers, William Boyd 9/13/2016 CDTL Review William Boyd, Wiley Chambers 11/29/2016 Statistical Review Abel Eshete, Yan Wang 11/8/2016 Pharmacology Toxicology Review Aaron Ruhland, Lori Kotch 11/7/2016 CMC Review Haripada Sanker, Milton Sloan, Maotang Zhou, Denise Miller, Vidya Pai, Om Anand, Erin Andrews, Chunchun Zhang, Paul Perdue 10/12/2016, 11/10/2016 Clinical Pharmacology Review Abhay Joshi, Philip Colangelo 11/9/2016 OPDP/DPDP Carrie Newcomer 11/7/2016 OSI/DGCPC N/A Proprietary Name Michelle Rutledge, Yelena Maslov, Lubna Merchant 6/1/2016 Conditionally acceptable letter Todd Bridges 6/2/2016 OSE/DMEPA Michelle Rutledge, Yelena Maslov 6/8/2016 OSE/DDRE N/A OSE/DRISK N/A Project Manager Michael Puglisi OND=Office of New Drugs CDTL=Cross-Discipline Team Leader OSI/DGCPC=Office of Scientific Investigations/Division of Good Clinical Practice Compliance OPDP/DPDP=Office of Prescription Drug Promotion/Division of Prescription Drug Promotion OSE= Office of Surveillance and Epidemiology DMEPA=Division of Medication Error Prevention and Analysis DDRE= Division of Drug Risk Evaluation DRISK=Division of Risk Management Page 2 of 24 Reference ID: 4021108 NDA 208151, ISOPTO Atropine (atropine sulfate ophthalmic solution) 1% Cycloplegia, Mydriasis, Penalization of the healthy eye in the treatment of amblyopia Division Director Summary Review Signatory Authority Review Template 1. -

Anisocoria in an Intubated Patient with COVID-19 Sam Myers ,1,2 Minak Bhalla,1 Rohit Jolly,3 Saurabh Jain3
Case report BMJ Case Rep: first published as 10.1136/bcr-2020-240003 on 22 July 2021. Downloaded from Anisocoria in an intubated patient with COVID-19 Sam Myers ,1,2 Minak Bhalla,1 Rohit Jolly,3 Saurabh Jain3 1Department of Ophthalmology, SUMMARY CASE PRESENTATION Whittington Health NHS Trust, The effects of COVID-19 on the eye are still widely A- 74- year old man was admitted to the hospital London, UK 2 unknown. We describe a case of a patient who was with a 2- week history of cough, fever and progres- UCL Medical School, University intubated and proned in the intensive care unit (ICU) sive shortness of breath. He had a background of College London, London, UK hypothyroidism, hypertension and benign pros- 3Department of Ophthalmology, for COVID-19 and developed unilateral anisocoria. Royal Free London NHS CT venogram excluded a cavernous sinus thrombosis. tate hypertrophy. His initial imaging and swab test Foundation Trust, London, UK MRI of the head showed microhaemorrhages in the confirmed COVID-19. The patient was placed midbrain where the pupil reflex nuclei are located. After on a trial of continuous positive airway pressure Correspondence to the patient was stepped down from ICU, intraocular to support his deteriorating oxygen saturation. Dr Sam Myers; pressure (IOP) was found to be raised in that eye. A However, after a week of supportive therapy, he sam. myers1@ nhs. net diagnosis of subacute closed angle glaucoma was made. was transferred to the ICU and was supported with It is important for clinicians to rule out thrombotic mechanical ventilation and proning. -

World Health Organization Model List of Essential Medicines, 21St List, 2019
World Health Organizatio n Model List of Essential Medicines 21st List 2019 World Health Organizatio n Model List of Essential Medicines 21st List 2019 WHO/MVP/EMP/IAU/2019.06 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. World Health Organization Model List of Essential Medicines, 21st List, 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -

Tropicamide 2018 Newborn Use Only
Tropicamide 2018 Newborn Use Only Alert Watch for apnoeas and abdominal distension following administration. Lower concentration solutions and regimens minimising number of additional drops are recommended. Indication Induction of mydriasis and cycloplegia for diagnostic and therapeutic ophthalmic procedures. Action Anticholinergic drug that produces pupillary dilatation by inhibiting the sphincter pupillae muscle and paralysis of accommodation. Drug Type Antimuscarinic. Trade Name Minims Tropicamide Eye Drops Mydriacyl Eye drops Presentation Minims Tropicamide Eye Drops 0.5%, 1.0% solution. Mydriacyl Eye drops 0.5%, 1.0% 15 mL (multidose—excipients benzalkonium chloride 0.01%, sodium chloride, disodium edetate, hydrochloric acid and/or sodium hydroxide, purified water). Dosage/Interval Use in combination with phenylephrine 2.5% with or without cyclopentolate 0.5%. REGIMEN 1: Phenylephrine 2.5% + cyclopentolate 0.5% + tropicamide 0.5% eye drops [1-4]. Instil one drop of each agent (5 minutes apart) into each eye 60 minutes prior to examination. Repeat if pupillary dilatation inadequate. Perform examination 60 to 120 minutes after instillation. REGIMEN 2: Phenylephrine 2.5% + tropicamide 0.5% eye drops [5-7]. Instil one drop of each agent (5 minutes apart) into each eye 60 minutes prior to examination. Repeat if pupillary dilatation inadequate. Perform examination 60 to 120 minutes after instillation. Dark irides may require additional drops. Maximum daily dose REGIMEN 1: 3 drops of each agent. REGIMEN 2: 4 drops of each agent. Route Topical instillation into the eyes from the container or use a microdrop (5–7 microL) cannula. Preparation/Dilution Administration Apply pressure to the lacrimal sac during and for 60 seconds after instillation of eye drop to minimise systemic absorption. -

Anisocoria Greater in the Dark: It’S Not Just All About Horner Pupil
RESIDENT & FELLOW SECTION Pearls & Oy-sters: Anisocoria Greater in the Dark: It’s Not Just All About Horner Pupil Emily Witsberger, MD, Sasha A. Mansukhani, MBBS, John J. Chen, MD, PhD, and M. Tariq Bhatti, MD Correspondence Dr. Bhatti Neurology 2021;96:719-722. doi:10.1212/WNL.0000000000011221 ® Bhatti.Muhammad@ mayo.edu Pearls MORE ONLINE c An initial step in the evaluation of anisocoria is assessing the pupillary light reflex. If a pupil Video is not responsive to light, then the near pupillary reflex needs to be evaluated. Unilateral light-near pupil dissociation occurs due to a lesion of the ciliary ganglion, postganglionic parasympathetic pathway, retina, or optic nerve. Oy-sters c In addition to a Horner pupil, anisocoria can be more pronounced in the dark with physiologic anisocoria, miosis due to posterior iris synechiae, pharmacologic miosis due to a parasympathomimetic agent (i.e., pilocarpine), traumatic miosis, iris ischemia, and a chronic Adie tonic pupil. c Adie tonic pupil most frequently presents with a mydriatic pupil, light-near dissociation, vermiform iris sphincter muscle movement, and anisocoria greater in the light. However, a chronic Adie tonic pupil may be characterized by a miotic pupil, light-near dissociation, and anisocoria that is greater in the dark. An asymptomatic 65-year-old patient with no prior ocular surgery but a history of hypertension, hyperlipidemia, and hypothyroidism was noted to have a left miotic pupil during a routine ophthalmic examination. The anisocoria was noted to be greater in the dark and was interpreted as a left Horner pupil. No pharmacologic testing was performed. -
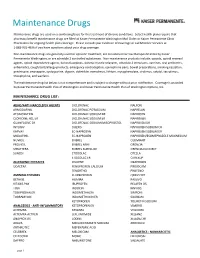
Maintenance Drug List Below Is Not Comprehensive and Is Subject to Change Without Prior Notification
Maintenance Drugs Maintenance drugs are used on a continuing basis for the treatment of chronic conditions. Select health plans require that pharmacy benefit maintenance drugs are filled at Kaiser Permanente Washington Mail Order or Kaiser Permanente Clinic Pharmacies for ongoing health plan coverage. Please consult your Evidence of Coverage or call Member Services at 1-888-901-4636 if you have questions about your drug coverage. Non-maintenance drugs are generally used for episodic treatment, are considered narrow therapeutic index by Kaiser Permanente Washington, or are schedule 2 controlled substances. Non-maintenance products include: opioids, opioid reversal agents, opioid dependence agents, benzodiazepines, skeletal muscle relaxants, schedule 2 stimulants, vaccines, oral antibiotics, antiemetics, cough/cold/allergy products, emergency contraception, epinephrine pens, bowel preparations, smoking cessation, prednisone, enoxaparin, cyclosporine, digoxin, dofetilide, everolimus, lithium, mycophenolate, sirolimus, sotalol, tacrolimus, theophylline, and warfarin. The maintenance drug list below is not comprehensive and is subject to change without prior notification. Coverage is provided by Kaiser Permanente Health Plan of Washington and Kaiser Permanente Health Plan of Washington Options, Inc. MAINTENANCE DRUG LIST: ADHD/ANTI-NARCOLEPSY AGENTS DICLOFENAC NALFON ARMODAFINIL DICLOFENAC POTASSIUM NAPRELAN ATOMOXETINE DICLOFENAC SODIUM DR NAPROSYN CLONIDINE HCL ER DICLOFENAC SODIUM ER NAPROXEN GUANFACINE ER DICLOFENAC SODIUM/MISOPROSTOL NAPROXEN