208151Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chlorpromazine-Induced Cataract and Corneal Pigmentation
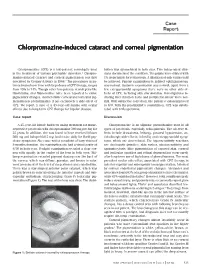
Case Report Chlorpromazine-induced cataract and corneal pigmentation Chlorpromazine (CPZ) is a low-potency neuroleptic used bution was symmetrical in both eyes. Two independent clini- in the treatment of various psychiatric disorders.1 Chlorpro- cians documented the condition. The pupils were dilated with mazine-induced cataract and corneal pigmentation was first 1% tropicamide for retinoscopy. A dilatation of only 4 mm could described by Greiner & Berry in 1964.2 The prevalence in pa- be achieved. Fundus examination by indirect ophthalmoscopy tients treated over time with large doses of CPZ therapy, ranges was normal. Systemic examination was normal; apart from a from 15% to 74%. Though other low-potency neuroleptics like few extrapyramidal symptoms there were no other side-ef- thioridazine and fluphenazine have been reported to cause fects of CPZ, including skin discoloration. Investigations in- pigmentary changes, characteristic corneal and lenticular pig- cluding liver function tests and peripheral smear were nor- mentation is predominantly if not exclusively a side-effect of mal. With subjective correction, the patient’s vision improved CPZ. We report a case of a 45-year-old female with ocular to 6/9. With the psychiatrist’s consultation, CPZ was substi- effects due to long-term CPZ therapy for bipolar disease. tuted with trifluoperazine. Case report Discussion A 45-year-old female had been taking treatment for manic- Chlorpromazine is an aliphatic phenothiazine used in all depressive psychosis with chlorpromazine 300 mg per day for types of psychosis, especially schizophrenia. The adverse ef- 25 years. In addition, she was found to have received lithium fects include drowsiness, lethargy, postural hypotension, an- 300 mg and haloperidol 5 mg, both twice daily for florid psy- ticholinergic side-effects, infertility and extrapyramidal symp- chotic symptoms. -

Non-Steroidal Drug-Induced Glaucoma MR Razeghinejad Et Al 972
Eye (2011) 25, 971–980 & 2011 Macmillan Publishers Limited All rights reserved 0950-222X/11 www.nature.com/eye 1,2 1 1 Non-steroidal drug- MR Razeghinejad , MJ Pro and LJ Katz REVIEW induced glaucoma Abstract vision. The majority of drugs listed as contraindicated in glaucoma are concerned with Numerous systemically used drugs are CAG. These medications may incite an attack in involved in drug-induced glaucoma. Most those individuals with narrow iridocorneal reported cases of non-steroidal drug-induced angle.3 At least one-third of acute closed-angle glaucoma are closed-angle glaucoma (CAG). glaucoma (ACAG) cases are related to an Indeed, many routinely used drugs that have over-the-counter or prescription drug.1 Prevalence sympathomimetic or parasympatholytic of narrow angles in whites from the Framingham properties can cause pupillary block CAG in study was 3.8%. Narrow angles are more individuals with narrow iridocorneal angle. The resulting acute glaucoma occurs much common in the Asian population. A study of a more commonly unilaterally and only rarely Vietnamese population estimated a prevalence 4 bilaterally. CAG secondary to sulfa drugs is a of occludable angles at 8.5%. The reported bilateral non-pupillary block type and is due prevalence of elevated IOP months to years to forward movement of iris–lens diaphragm, after controlling ACAG with laser iridotomy 5,6 which occurs in individuals with narrow or ranges from 24 to 72%. Additionally, a open iridocorneal angle. A few agents, significant decrease in retinal nerve fiber layer including antineoplastics, may induce thickness and an increase in the cup/disc ratio open-angle glaucoma. -

Muscarinic Acetylcholine Receptor
mAChR Muscarinic acetylcholine receptor mAChRs (muscarinic acetylcholine receptors) are acetylcholine receptors that form G protein-receptor complexes in the cell membranes of certainneurons and other cells. They play several roles, including acting as the main end-receptor stimulated by acetylcholine released from postganglionic fibersin the parasympathetic nervous system. mAChRs are named as such because they are more sensitive to muscarine than to nicotine. Their counterparts are nicotinic acetylcholine receptors (nAChRs), receptor ion channels that are also important in the autonomic nervous system. Many drugs and other substances (for example pilocarpineand scopolamine) manipulate these two distinct receptors by acting as selective agonists or antagonists. Acetylcholine (ACh) is a neurotransmitter found extensively in the brain and the autonomic ganglia. www.MedChemExpress.com 1 mAChR Inhibitors & Modulators (+)-Cevimeline hydrochloride hemihydrate (-)-Cevimeline hydrochloride hemihydrate Cat. No.: HY-76772A Cat. No.: HY-76772B Bioactivity: Cevimeline hydrochloride hemihydrate, a novel muscarinic Bioactivity: Cevimeline hydrochloride hemihydrate, a novel muscarinic receptor agonist, is a candidate therapeutic drug for receptor agonist, is a candidate therapeutic drug for xerostomia in Sjogren's syndrome. IC50 value: Target: mAChR xerostomia in Sjogren's syndrome. IC50 value: Target: mAChR The general pharmacol. properties of this drug on the The general pharmacol. properties of this drug on the gastrointestinal, urinary, and reproductive systems and other… gastrointestinal, urinary, and reproductive systems and other… Purity: >98% Purity: >98% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 10mM x 1mL in DMSO, Size: 10mM x 1mL in DMSO, 1 mg, 5 mg 1 mg, 5 mg AC260584 Aclidinium Bromide Cat. No.: HY-100336 (LAS 34273; LAS-W 330) Cat. -

Viewed the Existence of Multiple Muscarinic CNS Penetration May Occur When the Blood-Brain Barrier Receptors in the Mammalian Myocardium and Have Is Compromised
BMC Pharmacology BioMed Central Research article Open Access In vivo antimuscarinic actions of the third generation antihistaminergic agent, desloratadine G Howell III†1, L West†1, C Jenkins2, B Lineberry1, D Yokum1 and R Rockhold*1 Address: 1Department of Pharmacology and Toxicology, University of Mississippi Medical Center, Jackson, MS 39216, USA and 2Tougaloo College, Tougaloo, MS, USA Email: G Howell - [email protected]; L West - [email protected]; C Jenkins - [email protected]; B Lineberry - [email protected]; D Yokum - [email protected]; R Rockhold* - [email protected] * Corresponding author †Equal contributors Published: 18 August 2005 Received: 06 October 2004 Accepted: 18 August 2005 BMC Pharmacology 2005, 5:13 doi:10.1186/1471-2210-5-13 This article is available from: http://www.biomedcentral.com/1471-2210/5/13 © 2005 Howell et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Muscarinic receptor mediated adverse effects, such as sedation and xerostomia, significantly hinder the therapeutic usefulness of first generation antihistamines. Therefore, second and third generation antihistamines which effectively antagonize the H1 receptor without significant affinity for muscarinic receptors have been developed. However, both in vitro and in vivo experimentation indicates that the third generation antihistamine, desloratadine, antagonizes muscarinic receptors. To fully examine the in vivo antimuscarinic efficacy of desloratadine, two murine and two rat models were utilized. The murine models sought to determine the efficacy of desloratadine to antagonize muscarinic agonist induced salivation, lacrimation, and tremor. -

Muscarinic Cholinergic Receptors in Developing Rat Lung
1136 WHITSETT AND HOLLINGER Am J Obstet Gynecol 126:956 Michaelis LL 1978 The effects of arterial COztension on regional myocardial 2. Belik J, Wagerle LC, Tzimas M, Egler JM, Delivoria-Papadopoulos M 1983 and renal blood flow: an experimental study. J Surg Res 25:312 Cerebral blood flow and metabolism following pancuronium paralysis in 18. Leahy FAN. Cates D. MacCallum M. Rigatto H 1980 Effect of COz and 100% newborn lambs. Pediatr Res 17: 146A (abstr) O2 on cerebral blood flow in preterm infants. J Appl Physiol48:468 3. Berne RM, Winn HR, Rubio R 1981 The local regulation of cerebral blood 19. Norman J, MacIntyre J, Shearer JR, Craigen IM, Smith G 1970 Effect of flow. Prog Cardiovasc Dis 24:243 carbon dioxide on renal blood flow. Am J Physiol 219:672 4. Brann AW Jr, Meyers RE 1975 Central nervous system findings in the newborn 20. Nowicki PT, Stonestreet BS, Hansen NB, Yao AC, Oh W 1983 Gastrointestinal monkey following severe in utero partial asphyxia. Neurology 25327 blood flow and oxygen in awake newborn piglets: the effect of feeding. Am 5. Bucciarelli RL, Eitzman DV 1979 Cerebral blood flow during acute acidosis J Physiol245:G697 in perinatal goats. Pediatr Res 13: 178 21. Paulson OB, Olesen J, Christensen MS 1972 Restoration of auto-regulation of 6. Dobbing J, Sands J 1979 Comparative aspects of the brain growth spurt. Early cerebral blood flow by hypocapnia. Neurology 22:286 Hum Dev 3:79 22. Peckham GJ. Fox WW 1978 Physiological factors affecting pulmonary artery 7. Fox WW 1982 Arterial blood gas evaluation and mechanical ventilation in the pressure in infants with persistent pulmonary hypertension.J Pediatr 93: 1005 management of persistent pulmonary hypertension of the neonate. -

Palliative Care
World Health Organisation Essential Medicines List for Children (EMLc); Palliative Care CONSULTATION DOCUMENT Prepared by Anita Aindow Medicines Information Pharmacist Alder Hey Children’s Hospital, Liverpool, UK Dr Lynda Brook Macmillan Consultant in Paediatric Palliative Care Alder Hey Children’s Hospital, Liverpool, UK Acknowledgements Professor Tim Eden Professor of Paediatric Oncology, Royal Manchester Children’s Hospital, Manchester, UK Mr Anthony Nunn, Clinical Director of Pharmacy, Alder Hey Children’s Hospital, Liverpool, UK Dr Suzanne Hill Scientist, Policy, Access and Rational Use: Medicines Policy and Standards World health Authority, Geneva For their help and guidance in the preparation of this document Correspondence to Dr Lynda Brook, Macmillan Consultant in Paediatric Palliative Care Department of Paediatric Oncology, Royal Liverpool Children’s Hospital, Eaton Road, Liverpool, L12 2AP Tel: 0151 252 5187 Fax: 0151 252 5676 E-mail: [email protected] DECLARATION OF CONFLICT OF INTERESTS : None June 2008 WHO EMLc: Palliative Care – June 2008 CONTENTS Abstract 3 Summary of recommendations 5 Background 15 Methods 17 Identification of priorities for pharmacological management in palliative 17 care for children Pharmacological management of identified symptoms 17 Results 19 PRIORITIES FOR PHARMACOLOGICAL MANAGEMENT IN PALLIATIVE CARE FOR 19 CHILDREN ESSENTIAL MEDICINES FOR PHARMACOLOGICAL MANAGEMENT IN PALLIATIVE 23 CARE FOR CHILDREN Fatigue and weakness 24 Pain 29 Anorexia and weight loss 52 Delirium and agitation 55 Breathlessness 61 Nausea and vomiting 68 Constipation 89 Depression 95 Excess respiratory tract secretions 106 Anxiety 113 Appendix 116 2 WHO EMLc: Palliative Care – June 2008 ABSTRACT Background The World Health Organization (WHO) Essential Medicines List for Children (EMLc) aims to promote worldwide equity of access to essential medicines for children and is based on the criteria of safety, efficacy and cost effectiveness. -

Role of Muscarinic Acetylcholine Receptors in Adult Neurogenesis and Cholinergic Seizures
Role of Muscarinic Acetylcholine Receptors in Adult Neurogenesis and Cholinergic Seizures Rebecca L. Kow A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2014 Reding Committee: Neil Nathanson, Chair Sandra Bajjalieh Joseph Beavo Program Authorized to Offer Degree: Pharmacology ©Copyright 2014 Rebecca L. Kow University of Washington Abstract Role of Muscarinic Acetylcholine Receptors in Adult Neurogenesis and Cholinergic Seizures Rebecca L. Kow Chair of the Supervisory Committee: Professor Neil M. Nathanson Department of Pharmacology Muscarinic acetylcholine receptors (mAChRs) are G protein-coupled receptors (GPCRs) that mediate important functions in the periphery and in the central nervous systems. In the brain these receptors modulate many processes including learning, locomotion, pain, and reward behaviors. In this work we investigated the role of mAChRs in adult neurogenesis and further clarified the regulation of muscarinic agonist-induced seizures. We first investigated the role of mAChRs in adult neurogenesis in the subventricular zone (SVZ) and the subgranular zone (SGZ). We were unable to detect any modulation of adult neurogenesis by mAChRs. Administration of muscarinic agonists or antagonists did not alter proliferation or viability of adult neural progenitor cells (aNPCs) in vitro. Similarly, muscarinic agonists did not alter proliferation or survival of new adult cells in vivo. Loss of the predominant mAChR subtype in the forebrain, the M1 receptor, also caused no alterations in adult neurogenesis in vitro or in vivo, indicating that the M1 receptor does not mediate the actions of endogenous acetylcholine on adult neurogenesis. We also investigated the interaction between mAChRs and cannabinoid receptor 1 (CB1) in muscarinic agonist pilocarpine-induced seizures. -
Prohibited Substances List
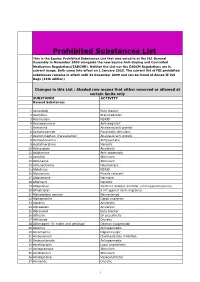
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Drug Repurposing for the Management of Depression: Where Do We Stand Currently?
life Review Drug Repurposing for the Management of Depression: Where Do We Stand Currently? Hosna Mohammad Sadeghi 1,†, Ida Adeli 1,† , Taraneh Mousavi 1,2, Marzieh Daniali 1,2, Shekoufeh Nikfar 3,4,5 and Mohammad Abdollahi 1,2,* 1 Toxicology and Diseases Group (TDG), Pharmaceutical Sciences Research Center (PSRC), The Institute of Pharmaceutical Sciences (TIPS), Tehran University of Medical Sciences, Tehran 1417614411, Iran; [email protected] (H.M.S.); [email protected] (I.A.); [email protected] (T.M.); [email protected] (M.D.) 2 Department of Toxicology and Pharmacology, School of Pharmacy, Tehran University of Medical Sciences, Tehran 1417614411, Iran 3 Personalized Medicine Research Center, Endocrinology and Metabolism Research Institute, Tehran University of Medical Sciences, Tehran 1417614411, Iran; [email protected] 4 Pharmaceutical Sciences Research Center (PSRC) and the Pharmaceutical Management and Economics Research Center (PMERC), Evidence-Based Evaluation of Cost-Effectiveness and Clinical Outcomes Group, The Institute of Pharmaceutical Sciences (TIPS), Tehran University of Medical Sciences, Tehran 1417614411, Iran 5 Department of Pharmacoeconomics and Pharmaceutical Administration, School of Pharmacy, Tehran University of Medical Sciences, Tehran 1417614411, Iran * Correspondence: [email protected] † Equally contributed as first authors. Citation: Mohammad Sadeghi, H.; Abstract: A slow rate of new drug discovery and higher costs of new drug development attracted Adeli, I.; Mousavi, T.; Daniali, M.; the attention of scientists and physicians for the repurposing and repositioning of old medications. Nikfar, S.; Abdollahi, M. Drug Experimental studies and off-label use of drugs have helped drive data for further studies of ap- Repurposing for the Management of proving these medications. -
![[3H]Acetylcholine to Muscarinic Cholinergic Receptors’](https://docslib.b-cdn.net/cover/7448/3h-acetylcholine-to-muscarinic-cholinergic-receptors-1087448.webp)
[3H]Acetylcholine to Muscarinic Cholinergic Receptors’
0270.6474/85/0506-1577$02.00/O The Journal of Neuroscience CopyrIght 0 Smety for Neurosmnce Vol. 5, No. 6, pp. 1577-1582 Prrnted rn U S.A. June 1985 High-affinity Binding of [3H]Acetylcholine to Muscarinic Cholinergic Receptors’ KENNETH J. KELLAR,2 ANDREA M. MARTINO, DONALD P. HALL, Jr., ROCHELLE D. SCHWARTZ,3 AND RICHARD L. TAYLOR Department of Pharmacology, Georgetown University, Schools of Medicine and Dentistry, Washington, DC 20007 Abstract affinities (Birdsall et al., 1978). Evidence for this was obtained using the agonist ligand [3H]oxotremorine-M (Birdsall et al., 1978). High-affinity binding of [3H]acetylcholine to muscarinic Studies of the actions of muscarinic agonists and detailed analy- cholinergic sites in rat CNS and peripheral tissues was meas- ses of binding competition curves between muscarinic agonists and ured in the presence of cytisin, which occupies nicotinic [3H]antagonists have led to the concept of muscarinic receptor cholinergic receptors. The muscarinic sites were character- subtypes (Rattan and Goyal, 1974; Goyal and Rattan, 1978; Birdsall ized with regard to binding kinetics, pharmacology, anatom- et al., 1978). This concept was reinforced by the discovery of the ical distribution, and regulation by guanyl nucleotides. These selective actions and binding properties of the antagonist pirenze- binding sites have characteristics of high-affinity muscarinic pine (Hammer et al., 1980; Hammer and Giachetti, 1982; Watson et cholinergic receptors with a Kd of approximately 30 nM. Most al., 1983; Luthin and Wolfe, 1984). An evolving classification scheme of the muscarinic agonist and antagonist drugs tested have for these muscarinic receptors divides them into M-l and M-2 high affinity for the [3H]acetylcholine binding site, but piren- subtypes (Goyal and Rattan, 1978; for reviews, see Hirschowitz et zepine, an antagonist which is selective for M-l receptors, al., 1984). -

Acepromazine and Chlorpromazine As Pharmaceutical-Grade Alternatives to Chlorprothixene for Pupillary Light Reflex Imaging in Mice
Journal of the American Association for Laboratory Animal Science Vol 59, No 2 Copyright 2020 March 2020 by the American Association for Laboratory Animal Science Pages 197–203 Acepromazine and Chlorpromazine as Pharmaceutical-grade Alternatives to Chlorprothixene for Pupillary Light Reflex Imaging in Mice Samantha S Eckley,1 Jason S Villano,1 Nora S Kuo,1 and Kwoon Y Wong2,* Studies of visual responses in isoflurane-anesthetized mice often use the sedative chlorprothixene to decrease the amount of isoflurane used because excessive isoflurane could adversely affect light-evoked responses. However, data are not available to justify the use of this nonpharmaceutical-grade chemical. The current study tested whether pharmaceutical-grade sedatives would be appropriate alternatives for imaging pupillary light reflexes. Male 15-wk-old mice were injected intraperitoneally with 1 mg/kg chlorprothixene, 5 mg/kg acepromazine, 10 mg/kg chlorpromazine, or saline. After anesthetic induction, anes- thesia maintenance used 0.5% and 1% isoflurane for sedative- and saline-injected mice, respectively. A photostimulus (16.0 log photons cm−2 s−1; 470 nm) was presented to the right eye for 20 min, during which the left eye was imaged for consensual pupillary constriction and involuntary pupil drift. Time to immobilization, loss of righting reflex, physiologic parameters, gain of righting reflex, and degree of recovery were assessed also. The sedative groups were statistically indistinguishable for all measures. By contrast, pupillary drift occurred far more often in saline-treated mice than in the sedative groups. Fur- thermore, saline-treated mice took longer to reach maximal pupil constriction than all sedative groups and had lower heart rates compared with chlorpromazine- and chlorprothixene-sedated mice. -

Tropicamide Tropicamide Eye Drops
Minims® Tropicamide Tropicamide Eye Drops Consumer Medicine Information Tell your doctor if you have or What is in this leaflet Before you use Minims have had any of the following Tropicamide This leaflet answers some common medical conditions: questions about Minims * glaucoma (high pressure in the Tropicamide, including how to use When you must not use it eye) the eye drops. * fast heartbeat or any heart Do not use Minims Tropicamide if It does not contain all the available condition or had heart surgery. you have an allergy to: information. It does not take the Tell your doctor if you are place of talking to your doctor or * any medicine containing pregnant or are breast-feeding. pharmacist. tropicamide Your doctor will discuss with you * any of the ingredients listed at the All medicines have benefits and the risks and benefits involved. risks. Your doctor has weighed the end of this leaflet. Tell your doctor if you wear risks of you using Minims Some of the symptoms of an allergic contact lenses. Tropicamide against the benefits they reaction may include: You should not wear contact lenses expect it will have for you. * shortness of breath while using this medicine. If you have any concerns about * wheezing or difficulty breathing using this medicine, ask your * swelling of the face, lips, tongue If you have not told your doctor doctor or pharmacist. about any of the above, tell or other parts of the body him/her before you start using Keep this leaflet with the medicine. * rash, itching or hives on the skin.