Afe Mydriasis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Taking the Mystery out of Abnormal Pupils
Taking the mystery out of abnormal pupils No financial disclosures Course Title: Taking the mystery out [email protected] of abnormal pupils Lecturer: Brad Sutton, OD, FAAO Clinical Professor IU School of Optometry . •Review of Anatomy Iris anatomy Iris sphincter Iris dilator Parasympathetic pathway Sympathetic pathway Parasympathetic Pathway Parasympathetic Pathway Light stimulates the retina then impulse Four neuron arc travels with the ganglion cells through the Retina to the pretectal nucleus in the chiasm into the optic tracts. 80% go to the midbrain (1) LGN , 20% to the pretectal nuclei.They Pretectal nucleus to the EW nucleus (2) then hemidecussate and terminate at the EW nucleus EW nucleus to the ciliary ganglion (3) Ciliary ganglion to the iris sphincter with short ciliary nerves (4) 1 Points of Interest Sympathetic Pathway Within the second order neuron there are Three neuron arc 30 near response fibers for every light Posterior hypothalamus to ciliospinal response fiber. This allows for light - near center of Budge ( C8 - T2 ). (1) dissociation. Center of Budge to the superior cervical The third order neuron runs with cranial ganglion in the neck (2) nerve III from the brain stem to the ciliary Superior cervical ganglion to the dilator ganglion. Superficially located prior to the muscle (3) cavernous sinus. Points of Interest Second order neuron runs along the surface of the lung, can be affected by a Pancoast tumor Third order neuron runs with the carotid artery then with the ophthalmic division of cranial nerve V 2 APD Testing testing……………….AKA……… … APD / reverse APD Direct and consensual response Which is the abnormal pupil ? Very simple rule. -

Miotics in Closed-Angle Glaucoma
Brit. J. Ophthal. (I975) 59, 205 Br J Ophthalmol: first published as 10.1136/bjo.59.4.205 on 1 April 1975. Downloaded from Miotics in closed-angle glaucoma F. GANIAS AND R. MAPSTONE St. Paul's Eye Hospital, Liverpool The initial treatment of acute primary closed-angle Table i Dosage in Groups I, 2, and 3 glaucoma (CAG) is directed towards lowering intraocular pressure (IOP) to normal levels as Group Case no. Duration IOP Time rapidly as possible. To this end, aqueous inflow is (days) (mm. Hg) (hrs) reduced by a drug such as acetazolamide (Diamox), and aqueous outflow is increased via the trabecular I I 2 8 5 meshwork by opening the closed angle with miotics. 3 7 21 3 The use of miotics is of respectable lineage and hal- 5 '4 48 7 lowed by usage, but regimes vary from "intensive" 7 8 I4 5 9 I0 I8 6 (i.e. frequent) to "occasional" (i.e. infrequent) instilla- I I 2 12 6 tions. Finally, osmotic agents are used after a variable '3 5 20 6 interval of time if the IOP remains raised. Tlle pur- I5 '4 I8 6 pose of this paper is to investigate the value of '7 '4 i6 6 miotics in the initial treatment of CAG. I9 6 02 2 2 2 8 2I 5 Material and methods 4 20t 20 6 Twenty patients with acute primary closed-angle glau- 6 I i8 5 http://bjo.bmj.com/ coma were treated, alternately, in one of two ways 8 4 i8 5 detailed below: I0 6 I8 6 I2 I0 20 6 (I) Intravenous Diamox 500 mg. -

Drug Class Review Ophthalmic Cholinergic Agonists
Drug Class Review Ophthalmic Cholinergic Agonists 52:40.20 Miotics Acetylcholine (Miochol-E) Carbachol (Isopto Carbachol; Miostat) Pilocarpine (Isopto Carpine; Pilopine HS) Final Report November 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Glaucoma Therapies ................................................................................................. 5 Table 2. Summary of Agents .................................................................................................. 6 Disease Overview ........................................................................................................................ 8 Table 3. Summary of Current Glaucoma Clinical Practice Guidelines ................................... 9 Pharmacology ............................................................................................................................... 10 Methods ....................................................................................................................................... -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -

Mydriasis Associated with Local Dysfunction of Parasympathetic Nerves in Two Dogs
NOTE Internal Medicine Mydriasis Associated with Local Dysfunction of Parasympathetic Nerves in Two Dogs Teppei KANDA1), Kazuhiro TSUJI1), Keiko HIYAMA2), Takeshi TSUKA1), Saburo MINAMI1), Yoshiaki HIKASA1), Toshinori FURUKAWA3) and Yoshiharu OKAMOTO1)* 1)Department of Veterinary Medicine, Faculty of Agriculture, Tottori University, 4–101, Koyama-minami, Tottori 680–8553, 2)Takamori Animal Hospital, 3706–2, Agarimichi, Sakaiminato, Tottori 684–0033 and 3)Department of Comparative Animal Science, College of Life Science, Kurashiki University of Science and the Arts, 2640, Tsurajima-nishinoura, Kurashiki, Okayama 712–8505, Japan. (Received 13 August 2009/Accepted 16 November 2009/Published online in J-STAGE 9 December 2009) ABSTRACT. In clinical practice, photophobia resulting from persistent mydriasis may be associated with dysfunction of ocular parasympa- thetic nerves or primary iris lesions. We encountered a 5-year-old Miniature Dachshund and a 7-year-old Shih Tzu with mydriasis, abnormal pupillary light reflexes, and photophobia. Except for sustained mydriasis and photophobia, no abnormalities were detected on general physical examination or ocular examination of either dog. We performed pharmacological examinations using 0.1% and 2% pilo- carpine to evaluate and diagnose parasympathetic denervation of the affected pupillary sphincter muscles. On the basis of the results, we diagnosed a pupillary abnormality due to parasympathetic dysfunction and not to overt primary iris lesions. The test revealed that neuroanatomic localization of the lesion was postciliary ganglionic in the first dog. KEY WORDS: autonomic nervous system, canine, mydriasis, ophthalmology, tonic pupil. J. Vet. Med. Sci. 72(3): 387–389, 2010 Mydriasis and miosis are normal physiological reactions and we report herein the clinical features, diagnosis, and that allow the eye to adjust to the level of incoming light. -
2002 Samel 10 Most Common Systemic Health Conditions with A
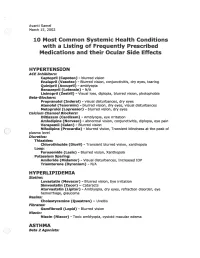
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

COMPLEMENTARY THERAPY ASSESSMENT VISUAL TRAINING for REFRACTIVE ERRORS August 2013
COMPLEMENTARY THERAPY ASSESSMENT VISUAL TRAINING FOR REFRACTIVE ERRORS August 2013 SUMMARY DESCRIPTION OF VISUAL TRAINING Vision training consists of a variety of programs designed to enhance visual efficiency and processing. Vision training, or orthoptics, typically addresses how well both eyes work together. Eye exercises may include, muscle relaxation techniques, biofeedback, eye patches, eye massages, the use of under-corrected prescription lenses, and/or nutritional supplements. Training is most often provided by an optometrist. BENEFITS One randomized controlled trial (RCT) of biofeedback training for control of accommodation for myopia reported no statistically significant benefits from training (Level I evidence). Another RCT (2013), which investigated vision training modalities to evaluate changes in peripheral refraction profiles in myopes, also found no evidence of benefits (Level 1 evidence). In other studies undertaken over the last 60 years, an improvement in subjective visual acuity (VA) in myopes with no corresponding improvement in objective VA has been reported (Level II/III evidence). RISKS The only risk attributable to visual training is financial. Most health insurers do not cover visual training programs. At the start of treatment, the optometrist should provide a reasonable estimate of what improvement to expect and how long it will take. CONCLUSIONS There is Level I evidence that visual training for control of accommodation has no effect on myopia. In other studies (Level II/III evidence), an improvement in subjective VA for patients with myopia that have undertaken visual training has been shown, but no corresponding physiological cause for the improvement has been demonstrated. It is postulated that the improvements in myopic patients noted in these studies were due to improvements in interpreting blurred images, changes in mood or motivation, creation of an artificial contact lens by tear film changes, or a pinhole effect from miosis of the pupil. -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Eye (2018) 32, 457–459 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2 2 2 Intermittent mydriasis PD Chamberlain , A Sadaka , S Berry CASE SERIES 1,2,3,4,5,6 associated with carotid and AG Lee vascular occlusion Abstract the literature as benign episodic pupillary dilation or BEUM. We report two patients with Purpose To describe two cases of 1 stereotyped, intermittent, neurologically acquired occlusive disease of the ipsilateral ICA Department of Ophthalmology, Blanton isolated, unilateral mydriasis in patients who developed multiple, stereotyped, neurologically isolated, transient episodes of Eye Institute, Houston with a history of acquired internal carotid Methodist Hospital, artery (ICA) occlusive disease on the mydriasis consistent with BEUM. We discuss the Houston, TX, USA ipsilateral side. possible mechanisms, differential diagnosis and 2 Patients Two patients with intermittent recommended evaluation for atypical cases for Department of episodic mydriasis. Ophthalmology, Baylor mydriasis. College of Medicine, Methods Case Series. Houston, TX, USA Results Case one: A 78-year-old man Case one 3 experienced 10 episodes of intermittent, Departments of Ophthalmology, Neurology, unilateral, and painless mydriasis in the left A 78-year-old man presented with 10 episodes of and Neurosurgery, Weill stereotyped, intermittent, unilateral, painless eye and had 100% occlusion of the left ICA Cornell Medical College, artery due to atherosclerotic disease. Case two: pupillary dilation of the left eye (OS) lasting New York, NY, USA A 26-year-old woman with history of migraine minutes to hours at a time without diplopia or fi 4Department of developed new painless, intermittent episodes ptosis. -

Glaucoma Medical Treatment: Philosophy, Principles and Practice
Glaucoma medical CLIVE MIGDAL treatment: philosophy, principles and practice Abstract assessment of these parameters. Indeed There have been numerous recent advances in compounds are under evaluation that affect the the management of glaucoma, not least the function of the optic nerve (via improved blood development of new drugs to help manage supply or improved neuronal cell physiology) raised intraocular pressure. In addition, the but may or may not lower lOP. It may even be concepts of improving blood flow to the optic possible in the future to therapeutically alter the nerve head and neuroprotection are currently human genome, genetically deliver provoking considerable interest. This article neuroprotective substances or aid regeneration considers the aims and philosophy of of the optic nerve axons. glaucoma drug therapy, summarises some of The main aim of glaucoma therapy must still the basic facts and principles of modem be the preservation of visual function. At the glaucoma medications, and suggests a same time, the therapy should not have adverse practical approach to the choice of therapy. side effects and should not affect the quality of life of the patient (by causing either side effects Key words Blood flow, Intraocular pressure, or inconvenience and disruption of daily Neuroprotection, Primary open angle glaucoma, Topical medications lifestyle). The cost of the therapy, both direct and indirect, must also be taken into consideration.s Currently, typical glaucoma management Philosophy consists of lowering the lOP to a satisfactory Primary open-angle glaucoma is a complex and safe target leve1.6 To determine the success disease for which a number of risk factors have of this treatment, the patient must be followed been identified, including intraocular pressure, long-term with routine assessment of lOP, discs age, race and family history.l,2 Due to our and fields to exclude progressive damage. -

Miotic Adie's Pupils
Journal of Cll/lical Neuro-ophtllJllmology 9(1): 43-45, 1989. RilVen Press, Ltd., New York Miotic Adie's Pupils Michael L. Rosenberg, M.D. Two young adults, aged 24 and 31, had a long history of Adie's syndrome or, pupillotonia, is typically small, poorly reactive pupilS. There was no history of characterized by either unilaterally or bilaterally large pupils, and a review of old photographs confirmed enlarged pupils that are unresponsive to light (1). 10 and 5 years, respectively, of miosis. Both were found to have bilateral tonic pupils that were supersensitive to The diagnosis is made clinically by watching for a diluted pilocarpine. Although it is possible that they had tonic constriction to near stimulation followed by a an unusually early onset of bilateral Adie's syndrome tonic redilatation. with dilated pupils that was not noticed, it is suggested Two young adults are described who were noted that some patients might have primary miotic Adie's during routine examinations to have bilaterally mi pupils without ever passing through a mydriatic phase. Key Words: Adie's syndrome-Argyll Robertson pu otic pupils that were thought to be fixed to light. pils-Miosis. They were both referred for the evaluation of Ar gyll Robertson pupils. Evaluation revealed bilat eral tonic reactions to near stimulation in both pa tients, typical of Adie's tonic pupilS. The diagnosis of parasympathetic denervation was confirmed in both patients as their pupils constricted with di luted pilocarpine. The cases reinforce the principle that any pupil regardless of size should be evalu ated for the possibility of pupillotonia.