Ophthalmology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

2018 Department of Ophthalmology Chair Report
SAVE THE▼ DATE Department of 200 Ophthalmology Years www.NYEE.edu Anniversary SPECIALTY REPORT | FALL 2018 www.NYEE.edu Celebration Join us for 200 Years and Counting: Bicentennial Cocktail Celebration October 15, 2020 Research Breakthrough: The Plaza 768 5th Avenue Gene Transfer New York, NY Therapy Restores 200 Years and Counting: Ophthalmology Vision in Mice Symposium October 16, 2020 Stay tuned for details on tickets and registration information. Cover image: Slice of a central retina section showing all layers (ONL, INL, GCL). Red indicates rod photoreceptors, located in outer nuclear layer (ONL). Green indicates Müller glial cells, whose cell bodies are located in inner nuclear layer (INL), and their branches across all three layers. Dark blue indicates the nucleus of all cells in three layers (GCL). Icahn School of Medicine at Medical Directors Neuro-Ophthalmology Uveitis and Ocular Immunology Mount Sinai Departmental Mark Kupersmith, MD Douglas Jabs, MD, MBA Avnish Deobhakta, MD Leadership System Chief, System Chief, Uveitis and Ocular Medical Director, NYEE - Neuro-Ophthalmology, Immunology, MSHS James C. Tsai, MD, MBA East 85th Street MSHS President, NYEE Stephanie Llop, MD System Chair, Department of Robin N. Ginsburg, MD 3 Message From the System Chair of the DepartmentValerie Elmalem, of Ophthalmology MD Sophia Saleem, MD Ophthalmology, MSHS Medical Director, NYEE- Joel Mindel, MD East 102nd Street Louis4 R. Pasquale,Breaking MD New Ground in Gene Transfer Therapy to Restore Vision Affiliated Leadership Ocular Oncology Site Chair, Department of Gennady Landa, MD Paul Finger, MD Ebby Elahi, MD, MBA Ophthalmology, MSH and MSQ Medical Director, NYEE- 6 This i-Doctor Is Transforming the Field of Ophthalmology President, NYEE/MSH System Vice Chair, Translational Williamsburg and Tribeca Ophthalmic Pathology Ophthalmology Alumni Ophthalmology Research, MSHS Jodi Sassoon, MD Society Kira Manusis, MD Inside Feature Site Chair, Pathology, NYEE Medical Director, NYEE- Paul A. -
RETINAL DISORDERS Eye63 (1)
RETINAL DISORDERS Eye63 (1) Retinal Disorders Last updated: May 9, 2019 CENTRAL RETINAL ARTERY OCCLUSION (CRAO) ............................................................................... 1 Pathophysiology & Ophthalmoscopy ............................................................................................... 1 Etiology ............................................................................................................................................ 2 Clinical Features ............................................................................................................................... 2 Diagnosis .......................................................................................................................................... 2 Treatment ......................................................................................................................................... 2 BRANCH RETINAL ARTERY OCCLUSION ................................................................................................ 3 CENTRAL RETINAL VEIN OCCLUSION (CRVO) ..................................................................................... 3 Pathophysiology & Etiology ............................................................................................................ 3 Clinical Features ............................................................................................................................... 3 Diagnosis ......................................................................................................................................... -
Outer Retina Changes on Optical Coherence Tomography in Vitamin a Defciency Meghan K
Berkenstock et al. Int J Retin Vitr (2020) 6:23 https://doi.org/10.1186/s40942-020-00224-1 International Journal of Retina and Vitreous CASE REPORT Open Access Outer retina changes on optical coherence tomography in vitamin A defciency Meghan K. Berkenstock, Charles J. Castoro and Andrew R. Carey* Abstract Background: Vitamin A defciency is rare in the United States and can be missed in patients with malabsorption syn- dromes without a high dose of suspicion. Ocular complications of hypovitaminosis A include xerosis and nyctalopia, and to a lesser extent reduction in visual acuity and color vision. Outer retinal changes, as seen on spectral domain optic coherence tomography (SD-OCT), in patients with vitamin A defciency have previously not been documented. Case presentation: We present two cases with symptoms of severe nyctalopia who were subsequently diagnosed with severe Vitamin A defciency and their unique fndings on SD-OCT of outer nuclear layer difuse thinning with irregular appearance of the interdigitating zone and the ellipsoid zone as well as normalization after vitamin A supplementation. Conclusions: Outer nuclear layer thinning and disruption of the outer retinal bands on SD-OCT are reversible with correction of vitamin A defciency. Improvement in visual acuity, color vision, and nyctalopia are possible with early diagnosis and appropriate treatment. Keywords: Vitamin A defciency, Optical coherence tomography, Nyctalopia Background reverse ocular complications prior to permanent vision Most commonly seen in regions with food insecurity, loss [16, 24, 25]. Only a few reports have described the nutritional defciencies, or restricted diets, vitamin A photoreceptor changes on spectral domain optical coher- defciency is rare in developed countries [1–9]. -

MRSA Ophthalmic Infection, Part 2: Focus on Orbital Cellulitis
Clinical Update COMPREHENSIVE MRSA Ophthalmic Infection, Part 2: Focus on Orbital Cellulitis by gabrielle weiner, contributing writer interviewing preston h. blomquist, md, vikram d. durairaj, md, and david g. hwang, md rbital cellulitis is a poten- Acute MRSA Cellulitis tially sight- and life-threat- ening disease that tops the 1A 1B ophthalmology worry list. Add methicillin-resistant OStaphylococcus aureus (MRSA) to the mix of potential causative bacteria, and the level of concern rises even higher. MRSA has become a relatively prevalent cause of ophthalmic infec- tions; for example, one study showed that 89 percent of preseptal cellulitis S. aureus isolates are MRSA.1 And (1A) This 19-month-old boy presented with left periorbital edema and erythema preseptal cellulitis can rapidly develop five days after having been diagnosed in an ER with conjunctivitis and treated into the more worrisome condition of with oral and topical antibiotics. (1B) Axial CT image of the orbits with contrast orbital cellulitis if not treated promptly shows lacrimal gland abscess and globe displacement. and effectively. Moreover, the community-associ- and Hospital System in Dallas, 86 per- When to Suspect ated form of MRSA (CA-MRSA) now cent of those with preseptal cellulitis MRSA Orbital Cellulitis accounts for a larger proportion of and/or lid abscesses had CA-MRSA. Patients with orbital cellulitis com- ophthalmic cases than health care– These studies also found that preseptal monly complain of pain when moving associated MRSA (HA-MRSA). Thus, cellulitis was the most common oph- the eye, decreased vision, and limited many patients do not have the risk fac- thalmic MRSA presentation from 2000 eye movement. -

Taking the Mystery out of Abnormal Pupils
Taking the mystery out of abnormal pupils No financial disclosures Course Title: Taking the mystery out [email protected] of abnormal pupils Lecturer: Brad Sutton, OD, FAAO Clinical Professor IU School of Optometry . •Review of Anatomy Iris anatomy Iris sphincter Iris dilator Parasympathetic pathway Sympathetic pathway Parasympathetic Pathway Parasympathetic Pathway Light stimulates the retina then impulse Four neuron arc travels with the ganglion cells through the Retina to the pretectal nucleus in the chiasm into the optic tracts. 80% go to the midbrain (1) LGN , 20% to the pretectal nuclei.They Pretectal nucleus to the EW nucleus (2) then hemidecussate and terminate at the EW nucleus EW nucleus to the ciliary ganglion (3) Ciliary ganglion to the iris sphincter with short ciliary nerves (4) 1 Points of Interest Sympathetic Pathway Within the second order neuron there are Three neuron arc 30 near response fibers for every light Posterior hypothalamus to ciliospinal response fiber. This allows for light - near center of Budge ( C8 - T2 ). (1) dissociation. Center of Budge to the superior cervical The third order neuron runs with cranial ganglion in the neck (2) nerve III from the brain stem to the ciliary Superior cervical ganglion to the dilator ganglion. Superficially located prior to the muscle (3) cavernous sinus. Points of Interest Second order neuron runs along the surface of the lung, can be affected by a Pancoast tumor Third order neuron runs with the carotid artery then with the ophthalmic division of cranial nerve V 2 APD Testing testing……………….AKA……… … APD / reverse APD Direct and consensual response Which is the abnormal pupil ? Very simple rule. -

Adult Patients Common Eye Infections
Common Eye Dermatitis: HZV and HSV Infections: Adult • Redness of periocular skin can be allergic Patients (if associated with prominent itching) or bacterial (if associated with open sores/wounds) Julie D. Meier, MD Assistant Professor of Ophthalmology • Both HZV and HSV can have devastating ocular sequelae if not treated promptly OSU Eye and Ear Institute General Categories of Herpes Zoster Eye Infections Ophthalmicus • Symptoms: Skin rash and pain, may be • Dermatitis of Lids (HZV, HSV) preceded by headache, fever, eye pain or • Cellulitis of Lids (pre- vs post-septal) blurred vision • Blepharitis • Signs: Vesicular skin rash involving CN V • Conjunctivitis distribution; Involvement of tip of nose can predict higher rate of ocular involvement • Keratitis 1 Herpes Zoster Herpes Simplex Virus Ophthalmicus • Symptoms: • Work-up 9 Duration of rash; Immunocompromised? 9 Red eye, pain, light sensitivity, skin rash 9 Complete ocular exam, including slit 9 Fever, flu-like symptoms lamp, IOP, and dilated exam • Signs: • Can have conjunctival or corneal involvement, elevated IOP, anterior 9 Skin rash: Clear vesicles on chamber inflammation, scleritis, or erythematous base that progress to even involvement of retina and optic crusting nerve. Herpes Zoster Herpes Simplex Virus Ophthalmicus • Work-up: • Treatment: 9 Previous episodes? 9 If present within 3 days of rash’s 9 Previous nasal, oral or genital sores? appearance: oral Acyclovir/ Valacyclovir 9 Recurrences can be triggered by fever, stress, trauma, UV exposure 9 Bacitracin ointment to skin lesions 9 External exam: More suggestive of HSV 9 Warm compresses if lesions centered around eye and no involvement of forehead/scalp 9 TOPICAL ANTIVIRALS (e.g. -

(12) Patent Application Publication (10) Pub. No.: US 2013/0172829 A1 BADAW (43) Pub
US 2013 0172829A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0172829 A1 BADAW (43) Pub. Date: Jul. 4, 2013 (54) DRY EYE TREATMENT SYSTEMS (52) U.S. Cl. CPC .................................... A61F 9/0008 (2013.01) (71) Applicant: SIGHT SCIENCES, INC., San USPC .......................................................... 604/294 Francisco, CA (US) (72) Inventor: Paul BADAWI, San Francisco, CA (US) (57) ABSTRACT (73) Assignee: SIGHT SCIENCES, INC., San Dry eye treatment apparatus and methods are described Francisco, CA (US) herein which generally comprise a patch or strip affixed to the skin of the upper and/or lower eyelids to deliver heat or other (21) Appl. No.: 13/645,985 forms of energy, pressure, drugs, moisture, etc. (alone or in combination) to the one or more meibomianglands contained (22) Filed: Oct. 5, 2012 within the underlying skin. The treatment strip or strips include one or more strips configured to adhere to an under Related U.S. Application Data lying region of skin in proximity to one or both eyes of a (63) Continuation-in-part of application No. 13/343,407, subject such that the one or more strips allow for the subject filed on Jan. 4, 2012. to blink naturally without restriction from the one or more patches. Moreover, the one or more Strips may be configured Publication Classification to emit energy to the underlying region of skin and where the one or more strips are shaped to follow a location of one or 51) Int.nt. CC. more me1bOm1amibomiam gland S COnta1nedined W1thinwithin the underlyingunderW1n A6DF 9/00 (2006.01) region of skin. -

Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy
Medical Coverage Policy Effective Date ............................................. 7/10/2021 Next Review Date ....................................... 3/15/2022 Coverage Policy Number .................................. 0554 Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy Table of Contents Related Coverage Resources Overview .............................................................. 1 Balloon Sinus Ostial Dilation for Chronic Sinusitis and Coverage Policy ................................................... 2 Eustachian Tube Dilation General Background ............................................ 3 Drug-Eluting Devices for Use Following Endoscopic Medicare Coverage Determinations .................. 10 Sinus Surgery Coding/Billing Information .................................. 10 Rhinoplasty, Vestibular Stenosis Repair and Septoplasty References ........................................................ 28 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence -

UCSF Ophthalmology Advice Guide Authors: Seanna Grob, MD, MAS
UCSF Ophthalmology Advice Guide Authors: Seanna Grob, MD, MAS and Neeti Parikh, MD Hello! We are excited that you are interested in ophthalmology! It is truly a special field in medicine. From saving someone’s vision after severe eye trauma, to restoring vision with cataract, retina, or cornea surgery, to preserving someone’s vision with glaucoma management and surgery, to reconstructing someone’s periocular area after trauma, burns, or tumor removal, amazing things can happen in ophthalmology. Ophthalmologists love their job and the majority say they would pick this specialty again if they had the choice. An incredible amount of job satisfaction comes from saving someone’s vision! We are here for you in the UCSF Department of Ophthalmology! We have put together this guide to help you through the process. This guide is meant to be very comprehensive. We want to make sure you are aware of all the opportunities and resources you have so that you can plan accordingly. You do not have to do everything we mention! Please feel free to reach out with questions about the specialty, how to get involved, and how to become a great ophthalmology applicant! 1 Medical School A well-rounded application is important for a successful match and any way you can prove to ophthalmology programs that you are dedicated to the field will be helpful to you. As more objective data (such as grades and board scores become less prevalent) other parts of your application will become more important. Various experiences you seek out are not only fun and educational, but will offer exposure to this wonderful field. -

JMSCR Vol||08||Issue||02||Page 208-210||February 2020
JMSCR Vol||08||Issue||02||Page 208-210||February 2020 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v8i2.40 Keratomalacia - A Case Report Authors Deepthi Pullepu1*, Deepthi Janga2, V Murali Krishna3 *Corresponding Author Deepthi Pullepu Department of Ophthalmology, Rangaraya Medical College, Kakinada, Andhra Pradesh, India Abstract Xerophthalmia refers to an ocular condition of destructive dryness of conjunctiva and cornea caused due to severe vitamin A deficiency. Usually affects infants, children and women of reproductive age group. It is estimated to affect about one-third of children under the age of five around the world. Keratomalacia means dry and cloudy cornea which melts and perforates, caused due to severe vitamin A deficiency. Here we describe a case of 21 year old female with neurofibromatosis type 1 presenting with keratomalacia. Keywords: Vitamin A deficiency, Xerophthalmia, Keratomalacia. Introduction blindness is a significant contributor Vitamin A is essential for the functioning of the In India, it is estimated that there are immune system, healthy growth and development approximately 6.8 million people who have vision of body and is usually acquired through diet. less than 6/60 in at least one eye due to corneal Globally, 190 million children under five years of diseases; of these, about a million have bilateral age are affected by vitamin A deficiency involvement. They suffer from an increased risk of visual Corneal blindness resulting due to this disease can impairment, illness and death from childhood be completely prevented by institution of effective infections such as measles and those causing preventive or prophylactic measures at the diarrhoea community level. -
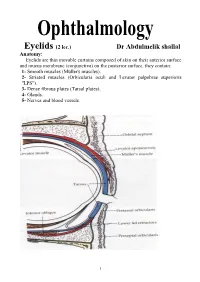
Eyelids (2 Lec.)
Eyelids (2 lec.) Dr Abdulmelik shallal Anatomy: Eyelids are thin movable curtains composed of skin on their anterior surface and mucus membrane (conjunctiva) on the posterior surface, they contain: 1- Smooth muscles (Müller's muscles). 2- Striated muscles (Orbicularis oculi and Levator palpebrae superioris "LPS"). 3- Dense fibrous plates (Tarsal plates). 4- Glands. 5- Nerves and blood vessels. 1 The contents of the lid are distributed as follows: the anterior surface is made of skin which has a round edge with the lid margin, the subcutaneous tissue, muscular layer, the submuscular (areolar tissue) layer, the orbital septum which end as a tarsal plate (that forms the architecture of lid) and finally the conjunctiva (palpebral) which is situated most posterior. The free margin of the eyelids contains: 1- The lashes (Cilia). 2- Grey line. 3- Orifices of Meibomian glands. 4- Mucocutaneous junction 5- Superior and inferior puncti of Naso-Lacrimal System (NLS). Muscles of the eyelids: 1- Orbicularis oculi muscle: It is a thin oval sheet of concentric striated muscle surrounding the palpebral fissure. It can be divided into: a- Peripheral (orbital) part: This is involved in forceful closure of lids. b- Central (palpebral) part: This is involved in involuntary blinking, voluntary nonforceful closure and participates in forceful closure with the orbital part. c- Muscle of Rioland's: this part is represented by the gray line of lid margin. d- lacrimalis muscle: that attached to the fundus of lacrimal sac. This part is involved in pumping action of lacrimal drainage system. Nerve supply: Sensory: Ophthalmic branch of trigeminal nerve Motor: Facial nerve.