Anisocoria Secondary to Inadvertent Contact with Scopolamine Patch Janki Shah,1 Alice Jiang,1 Zoltan Fekete2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -

URGENT/EMERGENT When to Refer Financial Disclosure
URGENT/EMERGENT When to Refer Financial Disclosure Speaker, Amy Eston, M.D. has a financial interest/agreement or affiliation with Lansing Ophthalmology, where she is employed as a ophthalmologist. 58 yr old WF with 6 month history of decreased vision left eye. Ache behind the left eye for 2-3 months. Using husband’s contact lens solution made it feel better. Seen by two eye care professionals. Given glasses & told eye exam was normal. No past ocular history Medical history of depression Takes only aspirin and vitamins 20/20 OD 20/30 OS Eye Pressure 15 OD 16 OS – normal Dilated fundus exam & slit lamp were normal Pupillary exam was normal Extraocular movements were full Confrontation visual fields were full No red desaturation Color vision was slightly decreased but the same in both eyes Amsler grid testing was normal OCT disc – OD normal OS slight decreased RNFL OCT of the macula was normal Most common diagnoses: Dry Eye Optic Neuritis Treatment - copious amount of artificial tears. Return to recheck refraction Visual field testing Visual Field testing - Small defect in the right eye Large nasal defect in the left eye Visual Field - Right Hemianopsia. MRI which showed a subacute parietal and occipital lobe infarct. ANISOCORIA Size of the Pupil Constrictor muscles innervated by the Parasympathetic system & Dilating muscles innervated by the Sympathetic system The Sympathetic System Begins in the hypothalamus, travels through the brainstem. Then through the upper chest, up through the neck and to the eye. The Sympathetic System innervates Mueller’s muscle which helps to elevate the upper eyelid. -

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Antiemetics/Antivertigo Agents
Antiemetic Agents Therapeutic Class Review (TCR) May 1, 2019 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. May 2019 Proprietary Information. Restricted Access – Do not disseminate or copy without approval. © 2004-2019 Magellan Rx Management. All Rights Reserved. 3 FDA-APPROVED INDICATIONS Drug Manufacturer Indication(s) NK1 receptor antagonists aprepitant capsules generic, Merck In combination with other antiemetic agents for: (Emend®)1 . -

Scopolamine As a Potential Treatment Option in Major Depressive Disorder - a Literature Review
Isr J Psychiatry - Vol. 58 - No 1 (2021) Scopolamine as a Potential Treatment Option in Major Depressive Disorder - A Literature Review Dusan Kolar, MD, MSc, PhD, FRCPC Department of Psychiatry, Queen’s University, Mood Disorders Research and Treatment Service, Kingston, Ontario, Canada as selective serotonin reuptake inhibitors (SSRIs) and ABSTRACT serotonin norepinephrine reuptake inhibitors (SNRIs), are currently used as first-line pharmacological treat- Introduction: Slow onset response to antidepressants ments for major depressive disorder (MDD). Despite the and partial response is a common problem in mood availability of a comprehensive list of antidepressants, disorders psychiatry. There is an ongoing need for rapid- approximately 50% of the patients on an antidepressant acting antidepressants, particularly after introducing regimen experience non-response to treatment (3, 4). ketamine in the treatment of depression. Scopolamine Furthermore, the mood elevating effects of antidepres- may have promise as an antidepressant. sant medication is often delayed (5). It is recommended Methods: The author conducted a literature review to that the patient be treated for at least six weeks with identify available treatment trials of scopolamine in the adequate dosage of the given antidepressant before unipolar and bipolar depression in PubMed, the Cochrane considering making changes to the treatment (5). Partial database, Ovid Medline and Google Scholar. to no response to treatment with antidepressants and delayed onset of action indicate that there is a need for Results: There have been eight treatment trials of the development of novel and improved medications scopolamine in MDD and bipolar depression. Seven for the treatment of depression. Many studies in recent studies confirmed significant antidepressant effects years have recognised two different classes of drugs with of scopolamine used as monotherapy and as an rapid and robust antidepressant effects. -

The Promise of Ketamine
Neuropsychopharmacology (2015) 40, 257–258 & 2015 American College of Neuropsychopharmacology. All rights reserved 0893-133X/15 www.neuropsychopharmacology.org Editorial Circumspectives: The Promise of Ketamine William A Carlezon*,1 and Tony P George2 1 2 Department of Psychiatry, Harvard Medical School, McLean Hospital, Belmont, MA, USA; Department of Psychiatry, University of Toronto, Toronto, Ontario, Canada Neuropsychopharmacology (2015) 40, 257–258; doi:10.1038/npp.2014.270 In this issue we reprise a Feature called Circumspectives. offering hope that fast-acting but safe antidepressants are The general format of a Circumspectives article is similar to possible. a debate, with separate sections in which two thought Despite growing enthusiasm for ketamine and its leaders articulate their individual positions on a topic of promise, Dr Schatzberg describes some sobering details great importance to our community of researchers. The and gaps in knowledge. Ketamine is a drug of abuse and, distinguishing element, however, is that the piece ends with despite some exceptionally elegant studies on the mechan- a ‘reconciliation’ that is co-authored by both and includes ism (eg, Li et al, 2010; Autry et al, 2011), there is no ideas or experiments that will move the field forward. consensus on how it produces therapeutic effects. As one The current Circumspectives (Sanacora and Schatzberg, example, Dr Schatzberg points out similarities in some of 2015) is entitled ‘Ketamine: Promising Path or False the molecular actions of ketamine and scopolamine, Prophecy in the Development of Novel Therapeutics for another familiar and long-standing member of our phama- Mood Disorders?’. It is co-authored by Gerard Sanacora and copea shown to produce rapid antidepressant effects (Furey Alan F Schatzberg, who are leaders in this field. -

The Anticholinergic Toxidrome
Poison HOTLINE Partnership between Iowa Health System and University of Iowa Hospitals and Clinics July 2011 The Anticholinergic Toxidrome A toxidrome is a group of symptoms associated with poisoning by a particular class of agents. One example is the opiate toxidrome, the triad of CNS depression, respiratory depression, and pinpoint pupils, and which usually responds to naloxone. The anticholinergic toxidrome is most frequently associated with overdoses of diphenhydramine, a very common OTC medication. However, many drugs and plants can produce the anticholinergic toxidrome. A partial list includes: tricyclic antidepressants (amitriptyline), older antihistamines (chlorpheniramine), Did you know …… phenothiazines (promethazine) and plants containing the anticholinergic alkaloids atropine, hyoscyamine and scopolamine (Jimson Weed). Each summer, the ISPCC receives approximately 10-20 The mnemonic used to help remember the symptoms and signs of this snake bite calls, some being toxidrome are derived from the Alice in Wonderland story: from poisonous snakes (both Blind as a Bat (mydriasis and inability to focus on near objects) local and exotic). Red as a Beet (flushed skin color) Four poisonous snakes can be Hot as Hades (elevated temperature) found in Iowa: the prairie These patients can sometimes die of agitation-induced hyperthermia. rattlesnake, the massasauga, Dry as a Bone (dry mouth and dry skin) the copperhead, and the Mad as a Hatter (hallucinations and delirium) timber rattlesnake. Each Bowel and bladder lose their tone (urinary retention and constipation) snake has specific territories Heart races on alone (tachycardia) within the state. ISPCC A patient who has ingested only an anticholinergic substance and is not specialists have access to tachycardic argues against a serious anticholinergic overdose. -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -

Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com
Hallucinogens And Dissociative Drug Use And Addiction Introduction Hallucinogens are a diverse group of drugs that cause alterations in perception, thought, or mood. This heterogeneous group has compounds with different chemical structures, different mechanisms of action, and different adverse effects. Despite their description, most hallucinogens do not consistently cause hallucinations. The drugs are more likely to cause changes in mood or in thought than actual hallucinations. Hallucinogenic substances that form naturally have been used worldwide for millennia to induce altered states for religious or spiritual purposes. While these practices still exist, the more common use of hallucinogens today involves the recreational use of synthetic hallucinogens. Hallucinogen And Dissociative Drug Toxicity Hallucinogens comprise a collection of compounds that are used to induce hallucinations or alterations of consciousness. Hallucinogens are drugs that cause alteration of visual, auditory, or tactile perceptions; they are also referred to as a class of drugs that cause alteration of thought and emotion. Hallucinogens disrupt a person’s ability to think and communicate effectively. Hallucinations are defined as false sensations that have no basis in reality: The sensory experience is not actually there. The term “hallucinogen” is slightly misleading because hallucinogens do not consistently cause hallucinations. 1 ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com How hallucinogens cause alterations in a person’s sensory experience is not entirely understood. Hallucinogens work, at least in part, by disrupting communication between neurotransmitter systems throughout the body including those that regulate sleep, hunger, sexual behavior and muscle control. Patients under the influence of hallucinogens may show a wide range of unusual and often sudden, volatile behaviors with the potential to rapidly fluctuate from a relaxed, euphoric state to one of extreme agitation and aggression. -
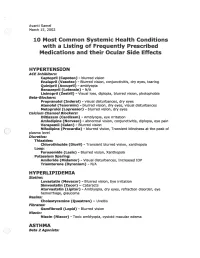
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Eye (2018) 32, 457–459 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2 2 2 Intermittent mydriasis PD Chamberlain , A Sadaka , S Berry CASE SERIES 1,2,3,4,5,6 associated with carotid and AG Lee vascular occlusion Abstract the literature as benign episodic pupillary dilation or BEUM. We report two patients with Purpose To describe two cases of 1 stereotyped, intermittent, neurologically acquired occlusive disease of the ipsilateral ICA Department of Ophthalmology, Blanton isolated, unilateral mydriasis in patients who developed multiple, stereotyped, neurologically isolated, transient episodes of Eye Institute, Houston with a history of acquired internal carotid Methodist Hospital, artery (ICA) occlusive disease on the mydriasis consistent with BEUM. We discuss the Houston, TX, USA ipsilateral side. possible mechanisms, differential diagnosis and 2 Patients Two patients with intermittent recommended evaluation for atypical cases for Department of episodic mydriasis. Ophthalmology, Baylor mydriasis. College of Medicine, Methods Case Series. Houston, TX, USA Results Case one: A 78-year-old man Case one 3 experienced 10 episodes of intermittent, Departments of Ophthalmology, Neurology, unilateral, and painless mydriasis in the left A 78-year-old man presented with 10 episodes of and Neurosurgery, Weill stereotyped, intermittent, unilateral, painless eye and had 100% occlusion of the left ICA Cornell Medical College, artery due to atherosclerotic disease. Case two: pupillary dilation of the left eye (OS) lasting New York, NY, USA A 26-year-old woman with history of migraine minutes to hours at a time without diplopia or fi 4Department of developed new painless, intermittent episodes ptosis.