Traumatic Cataract and Mydriasis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Albinism Terminology
Albinism Terminology Oculocutaneous Albinism (OCA): Oculocutaneous (pronounced ock-you-low-kew- TAIN-ee-us) Albinism is an inherited genetic condition characterized by the lack of or diminished pigment in the hair, skin, and eyes. Implications of this condition include eye and skin sensitivities to light and visual impairment. Ocular Albinism (OA): Ocular Albinism is an inherited genetic condition, diagnosed predominantly in males, characterized by the lack of pigment in the eyes. Implications of this condition include eye sensitivities to light and visual impairment. Hermansky Pudlak Syndrome (HPS): Hermansky-Pudlak Syndrome is a type of albinism which includes a bleeding tendency and lung disease. HPS may also include inflammatory bowel disease or kidney disease. The severity of these problems varies much from person to person, and the condition can be difficult to diagnose with traditional blood tests Chediak Higashi Syndrome: Chediak Higashi Syndrome is a type of albinism in which the immune system is affected. Illnesses and infections are common from infancy and can be severe. Issues also arise with blood clotting and severe bleeding. Melanin: Melanin is pigment found in a group of cells called melanocytes in most organisms. In albinism, the production of melanin is impaired or completely lacking. Nystagmus: Nystagmus is an involuntary movement of the eyes in either a vertical, horizontal, pendular, or circular pattern caused by a problem with the visual pathway from the eye to the brain. As a result, both eyes are unable to hold steady on objects being viewed. Nystagmus may be accompanied by unusual head positions and head nodding in an attempt to compensate for the condition. -

Partial Albinism (Heterochromia Irides) in Black Angus Cattle
Partial Albinism (Heterochromia irides) in Black Angus Cattle C. A. Strasia, Ph.D.1 2 J. L. Johnson, D. V.M., Ph.D.3 D. Cole, D. V.M.4 H. W. Leipold, D.M.V., Ph.D.5 Introduction Various types of albinism have been reported in many Pathological changes in ocular anomalies of incomplete breeds of cattle throughout the world.4 We describe in this albino cattle showed iridal heterochromia grossly. paper a new coat and eye color defect (partial albinism, Histopathological findings of irides showed only the heterochromia irides) in purebred Black Angus cattle. In posterior layer fairly pigmented and usually no pigment in addition, the results of a breeding trial using a homozygous the stroma nor the anterior layer. The ciliary body showed affected bull on normal Hereford cows are reported. reduced amount of pigmentation and absence of corpora Albinism has been described in a number of breeds of nigra. Choroid lacked pigmentation. The Retina showed cattle.1,3-8,12,16,17 An albino herd from Holstein parentage disorganization. Fundus anomalies included colobomata of was described and no pigment was evident in the skin, eyes, varying sizes at the ventral aspect of the optic disc and the horns, and hooves; in addition, the cattle exhibited photo tapetum fibrosum was hypoplastic.12 In albino humans, the phobia. A heifer of black pied parentage exhibited a fundus is depigmented and the choroidal vessels stand out complete lack of pigment in the skin, iris and hair; however, strikingly. Nystagmus, head nodding and impaired vision at sexual maturity some pigment was present and referred to also may occur. -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -
Wavelength of Light and Photophobia in Inherited Retinal Dystrophy
www.nature.com/scientificreports OPEN Wavelength of light and photophobia in inherited retinal dystrophy Yuki Otsuka1, Akio Oishi1,2*, Manabu Miyata1, Maho Oishi1, Tomoko Hasegawa1, Shogo Numa1, Hanako Ohashi Ikeda1 & Akitaka Tsujikawa1 Inherited retinal dystrophy (IRD) patients often experience photophobia. However, its mechanism has not been elucidated. This study aimed to investigate the main wavelength of light causing photophobia in IRD and diference among patients with diferent phenotypes. Forty-seven retinitis pigmentosa (RP) and 22 cone-rod dystrophy (CRD) patients were prospectively recruited. We designed two tinted glasses: short wavelength fltering (SWF) glasses and middle wavelength fltering (MWF) glasses. We classifed photophobia into three types: (A) white out, (B) bright glare, and (C) ocular pain. Patients were asked to assign scores between one (not at all) and fve (totally applicable) for each symptom with and without glasses. In patients with RP, photophobia was better relieved with SWF glasses {“white out” (p < 0.01) and “ocular pain” (p = 0.013)}. In CRD patients, there was no signifcant diference in the improvement wearing two glasses (p = 0.247–1.0). All RP patients who preferred MWF glasses had Bull’s eye maculopathy. Meanwhile, only 15% of patients who preferred SWF glasses had the fnding (p < 0.001). Photophobia is primarily caused by short wavelength light in many patients with IRD. However, the wavelength responsible for photophobia vary depending on the disease and probably vary according to the pathological condition. Inherited retinal degenerations (IRDs) represent a diverse group of diseases characterized by progressive photo- receptor cell death that can lead to blindness 1. -
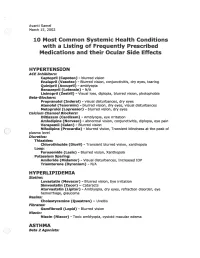
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

What Is Hermansky-Pudlak Syndrome?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What is Hermansky-Pudlak Syndrome? Hermansky-Pudlak Syndrome (HPS) is a rare inherited disease, named after two doctors in Czechoslovakia who, in 1959, recognized similar health conditions in two unrelated adults. Since the discovery of HPS, the condition has occurred all over the world but is most often seen in Puerto Rico. The most common health conditions with HPS are albinism, the tendency to Journal of Hematology bleed easily, and pulmonary fibrosis. A Figure 1. Normal platelet with dense bodies growing number of gene mutations have visualized by electron microscopy. been identified causing HPS (including numbers HPS1 to HPS10). What is albinism? Albinism is an inherited condition in which CLIP AND COPY AND CLIP reduced pigmentation (coloring) is present in the body. As a result, people with albinism are often fair-skinned with light hair. However, skin, hair, and eye color may vary, as some people with albinism may have dark brown hair and green or hazel/brown eyes. Journal of Hematology People with albinism all have low vision and Figure 2. Patient’s platelet with virtually absent dense bodies visualized by electron microscopy. varying degrees of nystagmus. All people who have HPS have albinism, but not all circulate in the blood stream and help the people with albinism have HPS. blood to clot. HPS patients have normal Skin problems—The reduction of numbers of platelets, but they are not pigmentation in the skin from albinism made correctly and do not function well, so results in an increased chance of developing the blood does not clot properly. -
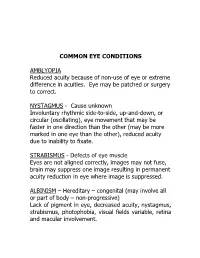
Common Eye Conditions
COMMON EYE CONDITIONS AMBLYOPIA Reduced acuity because of non-use of eye or extreme difference in acuities. Eye may be patched or surgery to correct. NYSTAGMUS - Cause unknown Involuntary rhythmic side-to-side, up-and-down, or circular (oscillating), eye movement that may be faster in one direction than the other (may be more marked in one eye than the other), reduced acuity due to inability to fixate. STRABISMUS - Defects of eye muscle Eyes are not aligned correctly, images may not fuse, brain may suppress one image resulting in permanent acuity reduction in eye where image is suppressed. ALBINISM – Hereditary – congenital (may involve all or part of body – non-progressive) Lack of pigment in eye, decreased acuity, nystagmus, strabismus, photophobia, visual fields variable, retina and macular involvement. ANIRIDIA – Hereditary Underdeveloped or absent iris. Decreased acuity, photophobia, nystagmus, cataracts, under developed retina. Visual fields normal unless glaucoma develops. CATARACTS – Congenital, hereditary, traumatic, disease, or age related (normal part of aging process) Lens opacity (chemical change in lens protein), decreased visual acuity, nystagmus, photophobia (light sensitivity). DIABETIC RETINOPATHY – Pathologic Retinal changes, proliferative – growth of abnormal new blood vessels, hemorrhage, fluctuating visual acuity, loss of color vision, field loss, retinal detachment, total blindness. GLAUCOMA (Congenital or adult) – “SNEAK THIEF OF SIGHT” hereditary, traumatic, surgery High intraocular pressure (above 20-21 mm of mercury) – (in children often accompanied by hazy corneas and large eyes), often due to obstructions that prevent fluid drainage, resulting in damage to optic nerve. Excessive tearing, photophobia, uncontrolled blinking, decreased acuity, constricted fields. HEMIANOPSIA – (Half-vision) optic pathway malfunction pathologic or trauma (brain injury, stroke or tumor) Macular vision may or may not be affected. -
Guidelines for Universal Eye Screening in Newborns Including RETINOPATHY of Prematurity
GUIDELINES FOR UNIVERSAL EYE SCREENING IN NEWBORNS INCLUDING RETINOPATHY OF PREMATURITY RASHTRIYA BAL SWASthYA KARYAKRAM Ministry of Health & Family Welfare Government of India June 2017 MESSAGE The Ministry of Health & Family Welfare, Government of India, under the National Health Mission launched the Rashtriya Bal Swasthya Karyakram (RBSK), an innovative and ambitious initiative, which envisages Child Health Screening and Early Intervention Services. The main focus of the RBSK program is to improve the quality of life of our children from the time of birth till 18 years through timely screening and early management of 4 ‘D’s namely Defects at birth, Development delays including disability, childhood Deficiencies and Diseases. To provide a healthy start to our newborns, RBSK screening begins at birth at delivery points through comprehensive screening of all newborns for various defects including eye and vision related problems. Some of these problems are present at birth like congenital cataract and some may present later like Retinopathy of prematurity which is found especially in preterm children and if missed, can lead to complete blindness. Early Newborn Eye examination is an integral part of RBSK comprehensive screening which would prevent childhood blindness and reduce visual and scholastic disabilities among children. Universal newborn eye screening at delivery points and at SNCUs provides a unique opportunity to identify and manage significant eye diseases in babies who would otherwise appear healthy to their parents. I wish that State and UTs would benefit from the ‘Guidelines for Universal Eye Screening in Newborns including Retinopathy of Prematurity’ and in supporting our future generation by providing them with disease free eyes and good quality vision to help them in their overall growth including scholastic achievement. -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Idiopathic Intracranial Hypertension
IDIOPATHIC INTRACRANIAL HYPERTENSION William L Hills, MD Neuro-ophthalmology Oregon Neurology Associates Affiliated Assistant Professor Ophthalmology and Neurology Casey Eye Institute, OHSU No disclosures CASE - 19 YO WOMAN WITH HEADACHES X 3 MONTHS Headaches frontal PMHx: obesity Worse lying down Meds: takes ibuprofen for headaches Wake from sleep Pulsatile tinnitus x 1 month. Vision blacks out transiently when she bends over or sits down EXAMINATION Vision: 20/20 R eye, 20/25 L eye. Neuro: PERRL, no APD, EOMI, VF full to confrontation. Dilated fundoscopic exam: 360 degree blurring of disc margins in both eyes, absent SVP. Formal visual field testing: Enlargement of the blind spot, generalized constriction both eyes. MRI brain: Lumbar puncture: Posterior flattening of Opening pressure 39 the globes cm H20 Empty sella Normal CSF studies otherwise normal Headache improved after LP IDIOPATHIC INTRACRANIAL HYPERTENSION SYNDROME: Increased intracranial pressure without ventriculomegaly or mass lesion Normal CSF composition NOMENCLATURE Idiopathic intracranial hypertension (IIH) Benign intracranial hypertension Pseudotumor cerebri Intracranial hypertension secondary to… DIAGNOSTIC CRITERIA Original criteria have been updated to reflect new imaging modalities: 1492 Friedman and Jacobsen. Neurology 2002; 59: Symptoms and signs reflect only those of - increased ICP or papilledema 1495 Documented increased ICP during LP in lateral decubitus position Normal CSF composition No evidence of mass, hydrocephalus, structural -

Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Eye (2018) 32, 457–459 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2 2 2 Intermittent mydriasis PD Chamberlain , A Sadaka , S Berry CASE SERIES 1,2,3,4,5,6 associated with carotid and AG Lee vascular occlusion Abstract the literature as benign episodic pupillary dilation or BEUM. We report two patients with Purpose To describe two cases of 1 stereotyped, intermittent, neurologically acquired occlusive disease of the ipsilateral ICA Department of Ophthalmology, Blanton isolated, unilateral mydriasis in patients who developed multiple, stereotyped, neurologically isolated, transient episodes of Eye Institute, Houston with a history of acquired internal carotid Methodist Hospital, artery (ICA) occlusive disease on the mydriasis consistent with BEUM. We discuss the Houston, TX, USA ipsilateral side. possible mechanisms, differential diagnosis and 2 Patients Two patients with intermittent recommended evaluation for atypical cases for Department of episodic mydriasis. Ophthalmology, Baylor mydriasis. College of Medicine, Methods Case Series. Houston, TX, USA Results Case one: A 78-year-old man Case one 3 experienced 10 episodes of intermittent, Departments of Ophthalmology, Neurology, unilateral, and painless mydriasis in the left A 78-year-old man presented with 10 episodes of and Neurosurgery, Weill stereotyped, intermittent, unilateral, painless eye and had 100% occlusion of the left ICA Cornell Medical College, artery due to atherosclerotic disease. Case two: pupillary dilation of the left eye (OS) lasting New York, NY, USA A 26-year-old woman with history of migraine minutes to hours at a time without diplopia or fi 4Department of developed new painless, intermittent episodes ptosis.