Clinical and Molecular Genetic Aspects of Leber's Congenital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multipurpose Conical Orbital Implant in Evisceration
Ophthalmic Plastic and Reconstructive Surgery Vol. 21, No. 5, pp 376–378 ©2005 The American Society of Ophthalmic Plastic and Reconstructive Surgery, Inc. Multipurpose Conical Orbital Implant in Evisceration Harry Marshak, M.D., and Steven C. Dresner, M.D. Doheny Eye Institute, Keck School of Medicine, University of Southern California, Los Angeles, California, U.S.A. Purpose: To evaluate the safety and efficacy of the porous polyethylene multipurpose conical orbital implant for use in evisceration. Methods: A retrospective review of 31 eyes that underwent evisceration and received the multipurpose conical orbital implant. The orbits were evaluated at 1 week, 1 month, and 6 months after final prosthetic fitting for implant exposure, superior sulcus deformity, and prosthetic motility. Results: There were no cases of extrusion, migration, or infection. All patients had a good cosmetic result after final prosthetic fitting. Prosthetic motility was good in all patients. Exposure developed in one eye (3%) and a superior sulcus deformity developed in one eye (3%). Conclusions: Placement of an multipurpose conical orbital implant in conjunction with evisceration is a safe and effective treatment for blind painful eye that achieves good motility and a good cosmetic result. visceration has proved to be effective for the treat- forms anteriorly to the sclera to be closed over it, without Ement of blind painful eye from phthisis bulbi or crowding the fornices, and extends posteriorly through endophthalmitis. By retaining the sclera in its anatomic the posterior sclerotomies, providing needed volume to natural position, evisceration has the advantage of allow- the posterior orbit. ing the insertions of the extraocular muscles to remain intact, promoting better motility. -

Treatment of Congenital Ptosis
13 Review Article Page 1 of 13 Treatment of congenital ptosis Vladimir Kratky1,2^ 1Department of Ophthalmology, Queen’s University, Kingston, Canada; 21st Medical Faculty, Charles University, Prague, Czech Republic Correspondence to: Vladimir Kratky, BSc, MD, FRCSC, DABO. Associate Professor of Ophthalmology, Director of Ophthalmic Plastic and Orbital Surgery, Oculoplastics Fellowship Director, Queen’s University, Kingston, Canada; 1st Medical Faculty, Charles University, Prague, Czech Republic. Email: [email protected]. Abstract: Congenital ptosis is an abnormally low position of the upper eyelid, with respect to the visual axis in the primary gaze. It can be present at birth or manifest itself during the first year of life and can be bilateral or unilateral. Additionally, it may be an isolated finding or part of a constellation of signs of a specific syndrome or systemic associations. Depending on how much it interferes with the visual axis, it may be considered as a functional or a cosmetic condition. In childhood, functional ptosis can lead to deprivation amblyopia and astigmatism and needs to be treated. However, even mild ptosis with normal vision can lead to psychosocial problems and correction is also advised, albeit on a less urgent basis. Although, patching and glasses can be prescribed to treat the amblyopia, the mainstay of management is surgical. There are several types of surgical procedure available depending on the severity and etiology of the droopy eyelid. The first part of this paper will review the different categories of congenital ptosis, including more common associated syndromes. The latter part will briefly cover the different surgical approaches, with emphasis on how to choose the correct condition. -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Albinism Terminology
Albinism Terminology Oculocutaneous Albinism (OCA): Oculocutaneous (pronounced ock-you-low-kew- TAIN-ee-us) Albinism is an inherited genetic condition characterized by the lack of or diminished pigment in the hair, skin, and eyes. Implications of this condition include eye and skin sensitivities to light and visual impairment. Ocular Albinism (OA): Ocular Albinism is an inherited genetic condition, diagnosed predominantly in males, characterized by the lack of pigment in the eyes. Implications of this condition include eye sensitivities to light and visual impairment. Hermansky Pudlak Syndrome (HPS): Hermansky-Pudlak Syndrome is a type of albinism which includes a bleeding tendency and lung disease. HPS may also include inflammatory bowel disease or kidney disease. The severity of these problems varies much from person to person, and the condition can be difficult to diagnose with traditional blood tests Chediak Higashi Syndrome: Chediak Higashi Syndrome is a type of albinism in which the immune system is affected. Illnesses and infections are common from infancy and can be severe. Issues also arise with blood clotting and severe bleeding. Melanin: Melanin is pigment found in a group of cells called melanocytes in most organisms. In albinism, the production of melanin is impaired or completely lacking. Nystagmus: Nystagmus is an involuntary movement of the eyes in either a vertical, horizontal, pendular, or circular pattern caused by a problem with the visual pathway from the eye to the brain. As a result, both eyes are unable to hold steady on objects being viewed. Nystagmus may be accompanied by unusual head positions and head nodding in an attempt to compensate for the condition. -

Partial Albinism (Heterochromia Irides) in Black Angus Cattle
Partial Albinism (Heterochromia irides) in Black Angus Cattle C. A. Strasia, Ph.D.1 2 J. L. Johnson, D. V.M., Ph.D.3 D. Cole, D. V.M.4 H. W. Leipold, D.M.V., Ph.D.5 Introduction Various types of albinism have been reported in many Pathological changes in ocular anomalies of incomplete breeds of cattle throughout the world.4 We describe in this albino cattle showed iridal heterochromia grossly. paper a new coat and eye color defect (partial albinism, Histopathological findings of irides showed only the heterochromia irides) in purebred Black Angus cattle. In posterior layer fairly pigmented and usually no pigment in addition, the results of a breeding trial using a homozygous the stroma nor the anterior layer. The ciliary body showed affected bull on normal Hereford cows are reported. reduced amount of pigmentation and absence of corpora Albinism has been described in a number of breeds of nigra. Choroid lacked pigmentation. The Retina showed cattle.1,3-8,12,16,17 An albino herd from Holstein parentage disorganization. Fundus anomalies included colobomata of was described and no pigment was evident in the skin, eyes, varying sizes at the ventral aspect of the optic disc and the horns, and hooves; in addition, the cattle exhibited photo tapetum fibrosum was hypoplastic.12 In albino humans, the phobia. A heifer of black pied parentage exhibited a fundus is depigmented and the choroidal vessels stand out complete lack of pigment in the skin, iris and hair; however, strikingly. Nystagmus, head nodding and impaired vision at sexual maturity some pigment was present and referred to also may occur. -
Wavelength of Light and Photophobia in Inherited Retinal Dystrophy
www.nature.com/scientificreports OPEN Wavelength of light and photophobia in inherited retinal dystrophy Yuki Otsuka1, Akio Oishi1,2*, Manabu Miyata1, Maho Oishi1, Tomoko Hasegawa1, Shogo Numa1, Hanako Ohashi Ikeda1 & Akitaka Tsujikawa1 Inherited retinal dystrophy (IRD) patients often experience photophobia. However, its mechanism has not been elucidated. This study aimed to investigate the main wavelength of light causing photophobia in IRD and diference among patients with diferent phenotypes. Forty-seven retinitis pigmentosa (RP) and 22 cone-rod dystrophy (CRD) patients were prospectively recruited. We designed two tinted glasses: short wavelength fltering (SWF) glasses and middle wavelength fltering (MWF) glasses. We classifed photophobia into three types: (A) white out, (B) bright glare, and (C) ocular pain. Patients were asked to assign scores between one (not at all) and fve (totally applicable) for each symptom with and without glasses. In patients with RP, photophobia was better relieved with SWF glasses {“white out” (p < 0.01) and “ocular pain” (p = 0.013)}. In CRD patients, there was no signifcant diference in the improvement wearing two glasses (p = 0.247–1.0). All RP patients who preferred MWF glasses had Bull’s eye maculopathy. Meanwhile, only 15% of patients who preferred SWF glasses had the fnding (p < 0.001). Photophobia is primarily caused by short wavelength light in many patients with IRD. However, the wavelength responsible for photophobia vary depending on the disease and probably vary according to the pathological condition. Inherited retinal degenerations (IRDs) represent a diverse group of diseases characterized by progressive photo- receptor cell death that can lead to blindness 1. -

Mouse Mutants As Models for Congenital Retinal Disorders
Experimental Eye Research 81 (2005) 503–512 www.elsevier.com/locate/yexer Review Mouse mutants as models for congenital retinal disorders Claudia Dalke*, Jochen Graw GSF-National Research Center for Environment and Health, Institute of Developmental Genetics, D-85764 Neuherberg, Germany Received 1 February 2005; accepted in revised form 1 June 2005 Available online 18 July 2005 Abstract Animal models provide a valuable tool for investigating the genetic basis and the pathophysiology of human diseases, and to evaluate therapeutic treatments. To study congenital retinal disorders, mouse mutants have become the most important model organism. Here we review some mouse models, which are related to hereditary disorders (mostly congenital) including retinitis pigmentosa, Leber’s congenital amaurosis, macular disorders and optic atrophy. q 2005 Elsevier Ltd. All rights reserved. Keywords: animal model; retina; mouse; gene mutation; retinal degeneration 1. Introduction Although mouse models are a good tool to investigate retinal disorders, one should keep in mind that the mouse Mice suffering from hereditary eye defects (and in retina is somehow different from a human retina, particular from retinal degenerations) have been collected particularly with respect to the number and distribution of since decades (Keeler, 1924). They allow the study of the photoreceptor cells. The mouse as a nocturnal animal molecular and histological development of retinal degener- has a retina dominated by rods; in contrast, cones are small ations and to characterize the genetic basis underlying in size and represent only 3–5% of the photoreceptors. Mice retinal dysfunction and degeneration. The recent progress of do not form cone-rich areas like the human fovea. -

What Is Hermansky-Pudlak Syndrome?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What is Hermansky-Pudlak Syndrome? Hermansky-Pudlak Syndrome (HPS) is a rare inherited disease, named after two doctors in Czechoslovakia who, in 1959, recognized similar health conditions in two unrelated adults. Since the discovery of HPS, the condition has occurred all over the world but is most often seen in Puerto Rico. The most common health conditions with HPS are albinism, the tendency to Journal of Hematology bleed easily, and pulmonary fibrosis. A Figure 1. Normal platelet with dense bodies growing number of gene mutations have visualized by electron microscopy. been identified causing HPS (including numbers HPS1 to HPS10). What is albinism? Albinism is an inherited condition in which CLIP AND COPY AND CLIP reduced pigmentation (coloring) is present in the body. As a result, people with albinism are often fair-skinned with light hair. However, skin, hair, and eye color may vary, as some people with albinism may have dark brown hair and green or hazel/brown eyes. Journal of Hematology People with albinism all have low vision and Figure 2. Patient’s platelet with virtually absent dense bodies visualized by electron microscopy. varying degrees of nystagmus. All people who have HPS have albinism, but not all circulate in the blood stream and help the people with albinism have HPS. blood to clot. HPS patients have normal Skin problems—The reduction of numbers of platelets, but they are not pigmentation in the skin from albinism made correctly and do not function well, so results in an increased chance of developing the blood does not clot properly. -

The Management of Congenital Malpositions of Eyelids, Eyes and Orbits
Eye (\988) 2, 207-219 The Management of Congenital Malpositions of Eyelids, Eyes and Orbits S. MORAX AND T. HURBLl Paris Summary Congenital malformations of the eye and its adnexa which are multiple and varied can affect the whole eyeball or any part of it, as well as the orbit, eyelids, lacrimal ducts, extra-ocular muscles and conjunctiva. A classification of these malformations is presented together with the general principles of treatment, age of operating and surgical tactics. The authors give some examples of the anatomo-clinical forms, eyelid malpositions such as entropion, ectropion, ptosis, levator eyelid retraction, medial canthus malposition, congenital eyelid colobomas, and congenital orbital abnormalities (Craniofacial stenosis, orbi tal plagiocephalies, hypertelorism, anophthalmos, microphthalmos and cryptophthalmos) . Congenital malformations of the eye and its as echography, CT-scan and NMR, enzymatic adnexa are multiple and varied. They can work-up or genetic studies (Table I). affect the whole eyeball or any part of it, as Surgical treatment when feasible will well as the orbit, eyelids, lacrimal ducts extra encounter numerous problems; age will play a ocular muscles and conjunctiva. role, choice of a surgical protocol directly From the anatomical point of view, the fol related to the existing complaints, and coop lowing can be considered. eration between several surgical teams Position abnormalities (malpositions) of (ophthalmologic, plastic, cranio-maxillo-fac one or more elements and formation abnor ial and neurosurgical), the ideal being to treat malities (malformations) of the same organs. Some of these abnormalities are limited to Table I The manag ement of cong enital rna/positions one organ and can be subjected to a relatively of eyelid s, eyes and orbits simple and well recognised surgical treat Ocular Findings: ment. -

TULP1 Mutations Causing Early-Onset Retinal Degeneration: Preserved but Insensitive Macular Cones
Retina TULP1 Mutations Causing Early-Onset Retinal Degeneration: Preserved but Insensitive Macular Cones Samuel G. Jacobson,1 Artur V. Cideciyan,1 Wei Chieh Huang,1 Alexander Sumaroka,1 Alejandro J. Roman,1 Sharon B. Schwartz,1 Xunda Luo,1 Rebecca Sheplock,1 Joanna M. Dauber,1 Malgorzata Swider,1 and Edwin M. Stone2,3 1Scheie Eye Institute, Department of Ophthalmology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, United States 2Department of Ophthalmology, University of Iowa Carver College of Medicine, Iowa City, Iowa, United States 3Howard Hughes Medical Institute, Iowa City, Iowa, United States Correspondence: Samuel G. Jacob- PURPOSE. To investigate visual function and outer and inner retinal structure in the rare form of son, Scheie Eye Institute, University retinal degeneration (RD) caused by TULP1 (tubby-like protein 1) mutations. of Pennsylvania, 51 N. 39th Street, Philadelphia, PA 19104, USA; METHODS. Retinal degeneration patients with TULP1 mutations (n ¼ 5; age range, 5–36 years) [email protected]. were studied by kinetic and chromatic static perimetry, en face autofluorescence imaging, and spectral-domain optical coherence tomography (OCT) scans. Outer and inner retinal Submitted: April 10, 2014 Accepted: July 13, 2014 laminar thickness were measured and mapped across the central retina. Comparisons were made with results from patients with RD associated with four ciliopathy genotypes (MAK, Citation: Jacobson SG, Cideciyan AV, RPGR, BBS1, and USH2A). Huang WC, et al. TULP1 mutations causing early-onset retinal degenera- RESULTS. The TULP1-RD patients were severely affected already in the first decade of life and tion: preserved but insensitive macu- there was rapidly progressive visual loss. -
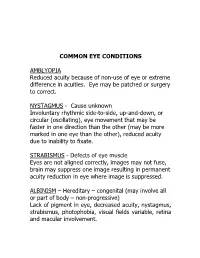
Common Eye Conditions
COMMON EYE CONDITIONS AMBLYOPIA Reduced acuity because of non-use of eye or extreme difference in acuities. Eye may be patched or surgery to correct. NYSTAGMUS - Cause unknown Involuntary rhythmic side-to-side, up-and-down, or circular (oscillating), eye movement that may be faster in one direction than the other (may be more marked in one eye than the other), reduced acuity due to inability to fixate. STRABISMUS - Defects of eye muscle Eyes are not aligned correctly, images may not fuse, brain may suppress one image resulting in permanent acuity reduction in eye where image is suppressed. ALBINISM – Hereditary – congenital (may involve all or part of body – non-progressive) Lack of pigment in eye, decreased acuity, nystagmus, strabismus, photophobia, visual fields variable, retina and macular involvement. ANIRIDIA – Hereditary Underdeveloped or absent iris. Decreased acuity, photophobia, nystagmus, cataracts, under developed retina. Visual fields normal unless glaucoma develops. CATARACTS – Congenital, hereditary, traumatic, disease, or age related (normal part of aging process) Lens opacity (chemical change in lens protein), decreased visual acuity, nystagmus, photophobia (light sensitivity). DIABETIC RETINOPATHY – Pathologic Retinal changes, proliferative – growth of abnormal new blood vessels, hemorrhage, fluctuating visual acuity, loss of color vision, field loss, retinal detachment, total blindness. GLAUCOMA (Congenital or adult) – “SNEAK THIEF OF SIGHT” hereditary, traumatic, surgery High intraocular pressure (above 20-21 mm of mercury) – (in children often accompanied by hazy corneas and large eyes), often due to obstructions that prevent fluid drainage, resulting in damage to optic nerve. Excessive tearing, photophobia, uncontrolled blinking, decreased acuity, constricted fields. HEMIANOPSIA – (Half-vision) optic pathway malfunction pathologic or trauma (brain injury, stroke or tumor) Macular vision may or may not be affected. -

Guidelines for Universal Eye Screening in Newborns Including RETINOPATHY of Prematurity
GUIDELINES FOR UNIVERSAL EYE SCREENING IN NEWBORNS INCLUDING RETINOPATHY OF PREMATURITY RASHTRIYA BAL SWASthYA KARYAKRAM Ministry of Health & Family Welfare Government of India June 2017 MESSAGE The Ministry of Health & Family Welfare, Government of India, under the National Health Mission launched the Rashtriya Bal Swasthya Karyakram (RBSK), an innovative and ambitious initiative, which envisages Child Health Screening and Early Intervention Services. The main focus of the RBSK program is to improve the quality of life of our children from the time of birth till 18 years through timely screening and early management of 4 ‘D’s namely Defects at birth, Development delays including disability, childhood Deficiencies and Diseases. To provide a healthy start to our newborns, RBSK screening begins at birth at delivery points through comprehensive screening of all newborns for various defects including eye and vision related problems. Some of these problems are present at birth like congenital cataract and some may present later like Retinopathy of prematurity which is found especially in preterm children and if missed, can lead to complete blindness. Early Newborn Eye examination is an integral part of RBSK comprehensive screening which would prevent childhood blindness and reduce visual and scholastic disabilities among children. Universal newborn eye screening at delivery points and at SNCUs provides a unique opportunity to identify and manage significant eye diseases in babies who would otherwise appear healthy to their parents. I wish that State and UTs would benefit from the ‘Guidelines for Universal Eye Screening in Newborns including Retinopathy of Prematurity’ and in supporting our future generation by providing them with disease free eyes and good quality vision to help them in their overall growth including scholastic achievement.