On the Tip of the Tongue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Lesions in Sjögren's Syndrome
Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Oral lesions in Sjögren’s syndrome patients Journal section: Oral Medicine and Pathology doi:10.4317/medoral.22286 Publication Types: Review http://dx.doi.org/doi:10.4317/medoral.22286 Oral lesions in Sjögren’s syndrome: A systematic review Julia Serrano 1, Rosa-María López-Pintor 1, José González-Serrano 1, Mónica Fernández-Castro 2, Elisabeth Casañas 1, Gonzalo Hernández 1 1 Department of Oral Medicine and Surgery, School of Dentistry, Complutense University, Madrid, Spain 2 Rheumatology Service, Hospital Infanta Sofía, Madrid, Spain Correspondence: Departamento de Especialidades Clínicas Odontológicas Facultad de Odontología Universidad Complutense de Madrid Plaza Ramón y Cajal s/n, 28040 Madrid. Spain [email protected] Serrano J, López-Pintor RM, González-Serrano J, Fernández-Castro M, Casañas E, Hernández G. Oral lesions in Sjögren’s syndrome: A system- atic review. Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Received: 18/11/2017 http://www.medicinaoral.com/medoralfree01/v23i4/medoralv23i4p391.pdf Accepted: 09/05/2018 Article Number: 22291 http://www.medicinaoral.com/ © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: [email protected] Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Médico Español Abstract Background: Sjögren’s syndrome (SS) is an autoimmune disease related to two common symptoms: dry mouth and eyes. Although, xerostomia and hyposialia have been frequently reported in these patients, not many studies have evaluated other oral manifestations. -
Benign Migratory Glossitis: Case Report and Literature Review
Volume 1- Issue 5 : 2017 DOI: 10.26717/BJSTR.2017.01.000482 Sarfaraz Khan. Biomed J Sci & Tech Res ISSN: 2574-1241 Case Report Open Access Benign Migratory Glossitis: Case Report and Literature Review Sarfaraz Khan1*, Syed AsifHaider Shah2, Tanveer Ahmed Mujahid3 and Muhammad Ishaq4 1Consultant Oral and Maxillofacial Surgeon, Pak Field Hospital Darfur, Sudan 2MDC Gujranwala, Pakistan 3Consultant Dermatologist, Pak Field Hospital Darfur, Sudan 4Registrar Dermatologist, Pak Field Hospital Darfur, Sudan Received: October 25, 2017; Published: October 31, 2017 *Corresponding author: Sarfaraz Khan, Consultant Oral and Maxillofacial Surgeon, Pakistan Field Hospital Darfur, Sudan, Tel: ; Email: Abstract Benign migratory Glossitis (BMG) is a benign, usually asymptomatic mucosal lesion of dorsal surface of the tongue, characterized by depapillated erythematous patches separated by white irregular borders. Etiology of BMG is unknown. Risk factors include psoriasis, fissured tongue, diabetes mellitus, hypersensitivity and psychological factors. We report BMG in an Egyptian soldier of UN peace keeping force, with stressKeywords: as a possible Geographic etiological tongue; factor Benign and migratory provide literature Glossitis; reviewErythema of this migrans disorder. Introduction Benign migratory Glossitis (BMG) is a benign, immune- spicy/salty food and/or alcoholic drinks [4,5].The lesion typically usually characterized by asymptomatic erythematous patches changes its shape with time owing to the change in pattern of mediated, chronic inflammatory lesion of unknown etiology, depapillation.Similar lesions may also be seen in atrophic candidiasis, local chemical or mechanical trauma, drug induced reactions, psoriasis with whitish margins across the surface of the tongue. This condition is also known as geographic tongue, erythema migrans, Treatment of symptomatic BMG aims at provision of symptomatic Glossitis exfoliativa and wandering rash of the tongue. -

Case Report Treatment of Geographic Tongue
Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2015; 2(7):409-413 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Treatment of Geographic Tongue Superimposing Fissured Tongue: A literature review with case report Jalaleddin H Hamissi1, Mahsa EsFehani2, Zahra Hamissi3 1Associate Professor in periodontics and Dental Caries Prevention Research Center, Qazvin University Medical Sciences, Qazvin, Iran. 2Assistant Professor, Department of Oral Medicine & Diagnosis, college dentistry, Qazvin University Medical Sciences, Qazvin, Iran. 3Dental Student, College of Dentistry, Shahied Behesti University of Medical Sciences, Teheran, Iran *Corresponding author Dr Jalaleddin H Hamissi Email: [email protected] ; [email protected] Abstract: Tongue is a most sensitive part of the oral cavity. It is responsible for many functions in the mouth like swallowing, speech, mastication, speaking and breathing. Geographic tongue (Benign migratory glossitis, erythema migrans) is an asymptomatic inflammatory disorder of tongue with controversial etiology. This disease is characterized by erythematous areas showing raised greyish or white circinate lines or bands with irregular pattern on the dorsal surface of the tongue and depapillation. The objective in presenting the case report and literature review is to discuss the clinical presentation, associated causative factors and management strategies of geographic tongue. Keywords: Asymptomatic; Characteristics; Fissured tongue; Geographic tongue; Migratory INTRODUCTION in approximately three percent (3%) majority of female Geographic tongue is an asymptomatic population [9]. On other aspects of oral mucosa, such as inflammatory condition of the dorsum of tongue on commissure of lip, floor of mouth, cheek etc., which occasionally extending towards the lateral borders. -
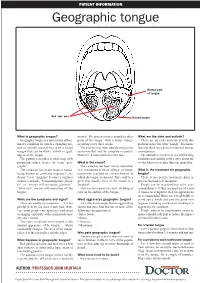
Geographic Tongue
PATIENT INFORMATION Geographic tongue Normal part of tongue Red ‘raw’ area Raised border What is geographic tongue? normal. The process moves around to other What are the risks and outlook? Geographic tongue is a non-serious inflam- parts of the tongue with a major change There are no risks associated with this matory condition in which a changing pat- occurring every three weeks. problem, hence the term “benign”. It is harm- tern of smooth red patches, with a raised The process may then subside and go into less and there have been no reported serious margin that can be white, yellow or grey, remission that may be complete or partial. consequences. appear on the tongue. However, it may return at a later time. The outlook is excellent. It is a self-limiting The pattern resembles a relief map with condition and usually settles after about six mountain ridges, hence the term “geo- What is the cause? weeks. However, it may flare up again later. graphic”. The cause has not been clearly identified. The condition has many medical names, It is considered to be an allergic or hyper- What is the treatment for geographic being known as erythema migrans (“ery- sensitivity reaction to certain factors to tongue? thema” = red, “migrans” because it migrates which the tongue is exposed. This could be a There is no specific treatment, drug or or moves around), “benign migratory glossi- germ that usually lives in the mouth or a process that makes it disappear. tis” or “benign inflammatory glossitis”. foodstuff. People can be reassured not to be con- “Glossitis” means inflammation of the This reaction causes excessive shedding of cerned about it. -

On the Tip of the Tongue
KNOWLEDGE TO PRACTICE DES CONNAISSANCES ÀLA PRATIQUE Diagnostic Challenge On the tip of the tongue . Rachel Orchard, MD*; Sheena Belisle, MD†; Rodrick Lim, MD†‡ Keywords: pediatric, rash, tongue, vesicle right-sided wheeze. Cardiovascular, abdominal, and neurological (including cranial nerve) examinations were unremarkable. CASE HISTORY What is the most likely diagnosis? A 14-year-old male presented to the pediatric emer- a) Drug eruption gency department (ED) with a chief complaint of b) Varicella zoster virus (VZV) changes to his tongue. He described a 3-day history of a c) Oral candidiasis gradually worsening sore, swollen tongue associated with a white plaque. This was accompanied by a 3-day d) Epstein-Barr virus history of a gradually worsening left-sided facial rash e) Oral lichen planus that had an intermittent mild tingling sensation. He also had a 1-week history of a productive cough with yellow mucus and generalized malaise. He had been seen at a walk-in clinic 2 days prior to presentation and was prescribed amoxicillin for presumed pneumo- nia, which he began the same day. He denied any history of fevers, facial weakness, neck stiffness, or eye symptoms. He was an otherwise well child, with up-to-date immunizations and a past medical history of chickenpox and recurrent furuncles as a younger child. On examination, he appeared well with the following vital signs: blood pressure 122/64 mm Hg, heart rate 73 beats per minute, respiratory rate 18 breaths per minute, temperature 36.8°C, and oxygen saturation of 99% on room air. Examination of his tongue revealed a symmetric white plaque along with ulcerative lesions on the left tongue and buccal mucosa (Figure 1). -

Oral Manifestations of a Possible New Periodic Fever Syndrome Soraya Beiraghi, DDS, MSD, MS, MSD1 • Sandra L
PEDIATRIC DENTISTRY V 29 / NO 4 JUL / AUG 07 Case Report Oral Manifestations of a Possible New Periodic Fever Syndrome Soraya Beiraghi, DDS, MSD, MS, MSD1 • Sandra L. Myers, DMD2 • Warren E. Regelmann, MD3 • Scott Baker, MD, MS4 Abstract: Periodic fever syndrome is composed of a group of disorders that present with recurrent predictable episodes of fever, which may be accompanied by: (1) lymphadenopathy; (2) malaise; (3) gastrointestinal disturbances; (4) arthralgia; (5) stomatitis; and (6) skin lesions. These signs and symptoms occur in distinct intervals every 4 to 6 weeks and resolve without any residual effect, and the patient remains healthy between attacks. The evaluation must exclude: (1) infections; (2) neoplasms; and (3) autoimmune conditions. The purpose of this paper is to report the case of a 4½- year-old white female who presented with a history of periodic fevers accompanied by: (1) joint pain; (2) skin lesions; (3) rhinitis; (4) vomiting; (5) diarrhea; and (6) an unusual asymptomatic, marked, fi ery red glossitis with features evolving to resemble geographic tongue and then resolving completely between episodes. This may represent the fi rst known reported case in the literature of a periodic fever syndrome presenting with such unusual recurring oral fi ndings. (Pediatr Dent 2007;29:323-6) KEYWORDS: PERIODIC FEVER, MOUTH LESIONS, GEOGRAPHIC TONGUE, STOMATITIS The diagnosis of periodic fever syndrome is often challeng- low, mildly painful ulcerations, which vary in number, and ing in children. Periodic fever syndrome is composed -

Burning Mouth Syndrome
Burning Mouth Syndrome Burning Mouth Syndrome Burning mouth syndrome (BMS) is a benign condition that presents as a burning sensation in the absence of any obvious findings in the mouth and in the absence of abnormal blood tests. BMS affects around 2% of the population with women being up to seven times more likely to be diagnosed than men. Female patients are predominately post-menopausal, although men and pre/peri-menopausal women may also be affected. For most patients, burning is experienced on the tip and sides of the tongue, top of the tongue, roof of the mouth, and the inside surface of the lips, although the pattern is highly variable and burning may occur anywhere in the mouth. A patient may feel he/she has burnt the mouth with hot food and there may be a sour, bitter, or metallic taste in the mouth. The mouth may also feel dry and food may have less flavor. Some patients may also report a “draining” or “crawling” sensation in the mouth. The onset of BMS is usually gradual with no known precipitating factor or event. Three clinical patterns have been well characterized: 1. No or little burning upon waking in the morning, with burning developing as the day progresses, and worst by evening. 2. Continuous symptoms throughout the day from the time one awakens. 3. Intermittent symptoms with some symptom-free days, least commonly observed presentation QUESTIONS AND ANSWERS ABOUT BURNING MOUTH SYNDROME Q: What causes BMS? A: No one really knows what causes BMS. However, it is believed to be a form of neuropathic pain. -

Oral Signs of Systemic Disease CDA 2015 Lecture Notes
2015-08-28 Oral Signs of Oral Signs of Systemic Disease Systemic Disease Why do you need to know? ! AHA! I diagnosed your systemic disease – less likely ! Helping your patients with known Karen Burgess, DDS, MSc, FRCDC systemic diseases - more likely Oral Pathology and Oral Medicine, Faculty of Dentistry, University of Toronto Department of Dentistry, Princess Margaret Hospital Department of Dentistry, Mt Sinai Hospital 2015-08-29 2015-08-29 2015-08-29 2015-08-29 2015-08-29 2015-08-29 Normal or Abnormal? Clinical description ! Type of abnormality (shape) ! The hardest part of oral pathology ! Number ! Colour ! Consistency ! Size - measure accurately ! Surface texture ! Location 2015-08-29 2015-08-29 2015-08-29 1 2015-08-28 Vocabulary Clinical description ! Ulcer ! Type of abnormality (shape) ! Vesicle/Bulla ! Number ! Macule ! Colour ! Patch ! Consistency ! Plaque ! Size - measure accurately ! Polyp- sessile or pedunculated ! Surface texture ! Location 2015-08-29 2015-08-29 2015-08-29 Description 2015-08-29 2015-08-29 2015-08-29 Differential Diagnosis Differential Diagnosis Differential Diagnosis ! Erythema multiforme ! Mucous membrane pemphigoid ! Primary herpes ! Erythema multiforme –"Any genital or eye lesions –"How long has it been present? ! Mucous membrane pemphigoid –"Any blisters? –"Any skin lesions? ! Pemphigus vulgaris ! Pemphigus vulgaris –"any skin lesions? ! Lichen planus ! Primary herpes –"Any blisters? –"How long has it been present? ! Lichen planus What information will help you narrow down –"Any other symptoms – malaise, -

Oral and Maxillo-Facial Manifestations of Systemic Diseases: an Overview
medicina Review Oral and Maxillo-Facial Manifestations of Systemic Diseases: An Overview Saverio Capodiferro *,† , Luisa Limongelli *,† and Gianfranco Favia Department of Interdisciplinary Medicine, University of Bari Aldo Moro, Piazza G. Cesare, 11, 70124 Bari, Italy; [email protected] * Correspondence: [email protected] (S.C.); [email protected] (L.L.) † These authors contributed equally to the paper. Abstract: Many systemic (infective, genetic, autoimmune, neoplastic) diseases may involve the oral cavity and, more generally, the soft and hard tissues of the head and neck as primary or secondary localization. Primary onset in the oral cavity of both pediatric and adult diseases usually represents a true challenge for clinicians; their precocious detection is often difficult and requires a wide knowledge but surely results in the early diagnosis and therapy onset with an overall better prognosis and clinical outcomes. In the current paper, as for the topic of the current Special Issue, the authors present an overview on the most frequent clinical manifestations at the oral and maxillo-facial district of systemic disease. Keywords: oral cavity; head and neck; systemic disease; oral signs of systemic diseases; early diagnosis; differential diagnosis Citation: Capodiferro, S.; Limongelli, 1. Introduction L.; Favia, G. Oral and Maxillo-Facial Oral and maxillo-facial manifestations of systemic diseases represent an extensive and Manifestations of Systemic Diseases: fascinating study, which is mainly based on the knowledge that many signs and symptoms An Overview. Medicina 2021, 57, 271. as numerous systemic disorders may first present as or may be identified by head and https://doi.org/10.3390/ neck tissue changes. -

Treating Burning Mouth Syndrome Constance R
East Tennessee State University Digital Commons @ East Tennessee State University ETSU Faculty Works Faculty Works 1-1-2009 Treating Burning Mouth Syndrome Constance R. Sharuga East Tennessee State University Debra Dotson East Tennessee State University Tabitha Price East Tennessee State University, [email protected] Follow this and additional works at: https://dc.etsu.edu/etsu-works Part of the Dental Hygiene Commons Citation Information Sharuga, Constance R.; Dotson, Debra; and Price, Tabitha. 2009. Treating Burning Mouth Syndrome. Dimensions of Dental Hygiene. Vol.7(12). 36-39. http://www.dimensionsofdentalhygiene.com/2009/12_December/Features/ Treating_Burning_Mouth_Syndrome.aspx ISSN: 1542-7919 This Article is brought to you for free and open access by the Faculty Works at Digital Commons @ East Tennessee State University. It has been accepted for inclusion in ETSU Faculty Works by an authorized administrator of Digital Commons @ East Tennessee State University. For more information, please contact [email protected]. Treating Burning Mouth Syndrome Copyright Statement Reprinted with permission. Constance R. Sharuga, Deborah Dotson, and Tabitha Price. Treating burning mouth syndrome. Dimensions of Dental Hygiene, December 2009; 7(12):36-39. This article is available at Digital Commons @ East Tennessee State University: https://dc.etsu.edu/etsu-works/2529 7/16/2018 Dimensions of Dental Hygiene Burning mouth syndrome (BMS) is a chronic, painful condition with no clear etiology or specific, proven treatment. BMS is also known as burning tongue syndrome, glossodynia, glossopyrosis, stomatodynia, stomatopyrosis, and oral dysesthesia.1,2 The syndrome is characterized by burning and/or painful sensations of the mouth, usually in the absence of clinical or laboratory findings.3 It can occur anywhere in the mouth. -
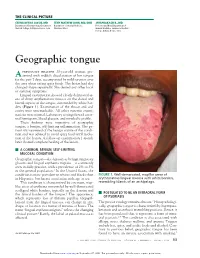
Geographic Tongue
THE CLINICAL PICTURE CEENA NEENA JACOB, MD TENY MATHEW JOHN, MD, DNB JAYAPRAKASH R., MD Department of Dermatology, Government Department of Internal Medicine, Professor and Head, Department of Medical College, Kottayam, Kerala, India Cleveland Clinic General Medicine, Travancore Medical College, Kollam, Kerala, India Geographic tongue previously healthy 35-year-old woman pre- A sented with reddish discoloration of her tongue for the past 7 days, accompanied by mild soreness over the area when eating spicy foods. The lesion had also changed shape repeatedly. She denied any other local or systemic symptoms. Lingual examination showed clearly delineated ar- eas of shiny, erythematous mucosa on the dorsal and lateral aspects of the tongue, surrounded by white bor- ders (Figure 1). Examination of the throat and oral cavity were unremarkable. All other systemic exami- nations were normal. Laboratory testing showed a nor- mal hemogram, blood glucose, and metabolic profi le. These fi ndings were suggestive of geographic tongue, a benign, self-limiting infl ammation. The pa- tient was reassured of the benign nature of the condi- tion and was advised to avoid spicy food until resolu- tion of the lesion. A follow-up examination 1 month later showed complete healing of the lesion. ■ A COMMON, BENIGN, SELF-LIMITING MUCOSAL CONDITION Geographic tongue—also known as benign migratory glossitis and lingual erythema migrans—is commonly seen in daily practice, with a prevalence of 2% to 3% in the general population.1 In the United States, the condition is more prevalent in whites and blacks than FIGURE 1. Well-demarcated, maplike areas of in Hispanics, but has no association with age or sex. -

Migratory Stomatitis – Case Presentation
Romanian Journal of Oral Rehabilitation Vol. 10, No. 4 October- December 2018 MIGRATORY STOMATITIS – CASE PRESENTATION Ana Maria Filioreanu¹, Cristina Popa¹*, George Alexandru Maftei¹,Ioanina Parlatescu², Carmen Larisa Nicolae², Eugenia Popescu³ 1Oral Medicine Discipline, Faculty of Dental Medicine, “Grigore T. Popa” University of Medicine and Pharmacy Iasi 2 Oral Medicine Discipline, Faculty of Dental Medicine, “Carol Davila” University of Medicine and Pharmacy Bucuresti 3 Oral Surgery Discipline, Faculty of Dental Medicine, “Grigore T. Popa” University of Medicine and Pharmacy Iasi *Corresponding author.Email: [email protected] Abstract Migratory stomatitis is a rare recurring condition of unknown etiology that mainly involves lingual mucosa, with a typical appearance of geographic tongue. Factors such as heredity, nutritional deficiencies or stress may be the contributing factors to the appearance of lesions. Clinically, they appear as circular, multiple, erythematous lesions with red spots surrounded by a white, narrow, hyperkeratotic aspect with irregular, slightly elevated appearance modifying its form in 24 hours.The condition may have spectacular clinical signs when the lesions are localised on the tongue, and may involve other areas of oral mucosa, such as labial or floor of mouth mucosa. The aim of this study is to present a clinical case of a patient with two localisations of lesions corresponding clinically to migratory stomatitis. The anatomopathological examination confirmed the migratory stomatitis diagnosis, so we could begin the specific treatment, to which the patient responded positively. Key words:migratory stomatitis, geographic tongue, geographic stomatitis Introduction through active and remission phases (geographic tongue - with no manifestations Migratory stomatitis is a tissue modification in other areas of oral mucosa); Type 2: of the oral mucosa that usually starts in geographic tongue, accompanied by lesions childhood, with autosomal dominant also located in other areas of oral mucosa; transmission and benign evolution[1, 2].