Treating Burning Mouth Syndrome Constance R
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

VOLUME 7 2 . No. 4 . AUGUST 2 0
VOLUME 72 . No.4 . AUGUST 2020 © 2020 EDIZIONI MINERVA MEDICA Minerva Pediatrica 2020 August;72(4):288-311 Online version at http://www.minervamedica.it DOI: 10.23736/S0026-4946.20.05861-2 REVIEW MANAGEMENT OF THE MAIN ENDOCRINE AND DIABETIC DISORDERS IN CHILDREN Current treatment for polycystic ovary syndrome: focus on adolescence Maria E. STREET 1 *, Francesca CIRILLO 1, Cecilia CATELLANI 1, 2, Marco DAURIZ 3, 4, Pietro LAZZERONI 1, Chiara SARTORI 1, Paolo MOGHETTI 4 1Division of Pediatric Endocrinology and Diabetology, Department of Mother and Child, Azienda USL – IRCCS di Reggio Emilia, Reggio Emilia, Italy; 2Clinical and Experimental Medicine PhD Program, University of Modena and Reggio Emilia, Modena, Italy; 3Section of Endocrinology and Diabetes, Department of Internal Medicine, Bolzano General Hospital, Bolzano, Italy; 4Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University and Hospital Trust of Verona, Verona, Italy *Corresponding author: Maria E. Street, Division of Pediatric Endocrinology and Diabetology, Department of Mother and Child, Azienda USL – IRCCS di Reggio Emilia, Viale Risorgimento 80, 42123 Reggio Emilia, Italy. E-mail: [email protected] ABSTRACT Polycystic ovary syndrome (PCOS) is the most frequent endocrine disorder in women and it is associated with an in- creased rate of infertility. Its etiology remains largely unknown, although both genetic and environmental factors play a role. PCOS is characterized by insulin resistance, metabolic disorders and low-grade chronic inflammation. To date, the treatment of PCOS is mainly symptomatic and aimed at reducing clinical signs of hyperandrogenism (hirsutism and acne), at improving menstrual cyclicity and at favoring ovulation. Since PCOS pathophysiology is still largely unknown, the therapeutic interventions currently in place are rarely cause-specific. -

Zeroing in on the Cause of Your Patient's Facial Pain
Feras Ghazal, DDS; Mohammed Ahmad, Zeroing in on the cause MD; Hussein Elrawy, DDS; Tamer Said, MD Department of Oral Health of your patient's facial pain (Drs. Ghazal and Elrawy) and Department of Family Medicine/Geriatrics (Drs. Ahmad and Said), The overlapping characteristics of facial pain can make it MetroHealth Medical Center, Cleveland, Ohio difficult to pinpoint the cause. This article, with a handy at-a-glance table, can help. [email protected] The authors reported no potential conflict of interest relevant to this article. acial pain is a common complaint: Up to 22% of adults PracticE in the United States experience orofacial pain during recommendationS F any 6-month period.1 Yet this type of pain can be dif- › Advise patients who have a ficult to diagnose due to the many structures of the face and temporomandibular mouth, pain referral patterns, and insufficient diagnostic tools. disorder that in addition to Specifically, extraoral facial pain can be the result of tem- taking their medication as poromandibular disorders, neuropathic disorders, vascular prescribed, they should limit disorders, or atypical causes, whereas facial pain stemming activities that require moving their jaw, modify their diet, from inside the mouth can have a dental or nondental cause and minimize stress; they (FIGURE). Overlapping characteristics can make it difficult to may require physical therapy distinguish these disorders. To help you to better diagnose and and therapeutic exercises. C manage facial pain, we describe the most common causes and underlying pathological processes. › Consider prescribing a tricyclic antidepressant for patients with persistent idiopathic facial pain. C Extraoral facial pain Extraoral pain refers to the pain that occurs on the face out- 2-15 Strength of recommendation (SoR) side of the oral cavity. -

Oral Lesions in Sjögren's Syndrome
Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Oral lesions in Sjögren’s syndrome patients Journal section: Oral Medicine and Pathology doi:10.4317/medoral.22286 Publication Types: Review http://dx.doi.org/doi:10.4317/medoral.22286 Oral lesions in Sjögren’s syndrome: A systematic review Julia Serrano 1, Rosa-María López-Pintor 1, José González-Serrano 1, Mónica Fernández-Castro 2, Elisabeth Casañas 1, Gonzalo Hernández 1 1 Department of Oral Medicine and Surgery, School of Dentistry, Complutense University, Madrid, Spain 2 Rheumatology Service, Hospital Infanta Sofía, Madrid, Spain Correspondence: Departamento de Especialidades Clínicas Odontológicas Facultad de Odontología Universidad Complutense de Madrid Plaza Ramón y Cajal s/n, 28040 Madrid. Spain [email protected] Serrano J, López-Pintor RM, González-Serrano J, Fernández-Castro M, Casañas E, Hernández G. Oral lesions in Sjögren’s syndrome: A system- atic review. Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Received: 18/11/2017 http://www.medicinaoral.com/medoralfree01/v23i4/medoralv23i4p391.pdf Accepted: 09/05/2018 Article Number: 22291 http://www.medicinaoral.com/ © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: [email protected] Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Médico Español Abstract Background: Sjögren’s syndrome (SS) is an autoimmune disease related to two common symptoms: dry mouth and eyes. Although, xerostomia and hyposialia have been frequently reported in these patients, not many studies have evaluated other oral manifestations. -
Benign Migratory Glossitis: Case Report and Literature Review
Volume 1- Issue 5 : 2017 DOI: 10.26717/BJSTR.2017.01.000482 Sarfaraz Khan. Biomed J Sci & Tech Res ISSN: 2574-1241 Case Report Open Access Benign Migratory Glossitis: Case Report and Literature Review Sarfaraz Khan1*, Syed AsifHaider Shah2, Tanveer Ahmed Mujahid3 and Muhammad Ishaq4 1Consultant Oral and Maxillofacial Surgeon, Pak Field Hospital Darfur, Sudan 2MDC Gujranwala, Pakistan 3Consultant Dermatologist, Pak Field Hospital Darfur, Sudan 4Registrar Dermatologist, Pak Field Hospital Darfur, Sudan Received: October 25, 2017; Published: October 31, 2017 *Corresponding author: Sarfaraz Khan, Consultant Oral and Maxillofacial Surgeon, Pakistan Field Hospital Darfur, Sudan, Tel: ; Email: Abstract Benign migratory Glossitis (BMG) is a benign, usually asymptomatic mucosal lesion of dorsal surface of the tongue, characterized by depapillated erythematous patches separated by white irregular borders. Etiology of BMG is unknown. Risk factors include psoriasis, fissured tongue, diabetes mellitus, hypersensitivity and psychological factors. We report BMG in an Egyptian soldier of UN peace keeping force, with stressKeywords: as a possible Geographic etiological tongue; factor Benign and migratory provide literature Glossitis; reviewErythema of this migrans disorder. Introduction Benign migratory Glossitis (BMG) is a benign, immune- spicy/salty food and/or alcoholic drinks [4,5].The lesion typically usually characterized by asymptomatic erythematous patches changes its shape with time owing to the change in pattern of mediated, chronic inflammatory lesion of unknown etiology, depapillation.Similar lesions may also be seen in atrophic candidiasis, local chemical or mechanical trauma, drug induced reactions, psoriasis with whitish margins across the surface of the tongue. This condition is also known as geographic tongue, erythema migrans, Treatment of symptomatic BMG aims at provision of symptomatic Glossitis exfoliativa and wandering rash of the tongue. -

Case Report Treatment of Geographic Tongue
Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2015; 2(7):409-413 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Treatment of Geographic Tongue Superimposing Fissured Tongue: A literature review with case report Jalaleddin H Hamissi1, Mahsa EsFehani2, Zahra Hamissi3 1Associate Professor in periodontics and Dental Caries Prevention Research Center, Qazvin University Medical Sciences, Qazvin, Iran. 2Assistant Professor, Department of Oral Medicine & Diagnosis, college dentistry, Qazvin University Medical Sciences, Qazvin, Iran. 3Dental Student, College of Dentistry, Shahied Behesti University of Medical Sciences, Teheran, Iran *Corresponding author Dr Jalaleddin H Hamissi Email: [email protected] ; [email protected] Abstract: Tongue is a most sensitive part of the oral cavity. It is responsible for many functions in the mouth like swallowing, speech, mastication, speaking and breathing. Geographic tongue (Benign migratory glossitis, erythema migrans) is an asymptomatic inflammatory disorder of tongue with controversial etiology. This disease is characterized by erythematous areas showing raised greyish or white circinate lines or bands with irregular pattern on the dorsal surface of the tongue and depapillation. The objective in presenting the case report and literature review is to discuss the clinical presentation, associated causative factors and management strategies of geographic tongue. Keywords: Asymptomatic; Characteristics; Fissured tongue; Geographic tongue; Migratory INTRODUCTION in approximately three percent (3%) majority of female Geographic tongue is an asymptomatic population [9]. On other aspects of oral mucosa, such as inflammatory condition of the dorsum of tongue on commissure of lip, floor of mouth, cheek etc., which occasionally extending towards the lateral borders. -

An Open-Label Pilot Trial of Alpha-Lipoic Acid for Weight Loss in Patients with Schizophrenia Without Diabetes Joseph C
Case Reports An Open-Label Pilot Trial of Alpha-Lipoic Acid for Weight Loss in Patients with Schizophrenia without Diabetes Joseph C. Ratliff1 , Laura B. Palmese 1, Erin L. Reutenauer 1, Cenk Tek 1 Abstract A possible mechanism of antipsychotic-induced weight gain is activation of hypothalamic monophosphate-dependent kinase (AMPK) mediated by histamine 1 receptors. Alpha-lipoic acid (ALA), a potent antioxidant, counteracts this ef- fect and may be helpful in reducing weight for patients taking antipsychotics. The objective of this open-label study was to assess the efficacy of ALA (1,200 mg) on twelve non-diabetic schizophrenia patients over ten weeks. Participants lost significant weight during the intervention (-2.2 kg±2.5 kg). ALA was well tolerated and was particularly effective for individuals taking strongly antihistaminic antipsychotics (-2.9 kg±2.6 kg vs. -0.5 kg±1.0 kg). Clinical Trial Registra- tion: NCT01355952. Key Words: Schizophrenia, Obesity, Schizoaffective Disorder, Alpha-Lipoic Acid Introduction dependent protein kinase (AMPK) in the hypothalamus Antipsychotic medications appear to induce weight (4). In the periphery, AMPK increases energy utilization; gain, which results in increased rates of obesity in schizo- AMPK activity in the hypothalamus increases appetite. phrenia (1). Schizophrenia patients have significantly short- Several highly orexigenic (stimulates appetite) antipsy- er life expectancy than the general population (2); most of chotics such as clozapine, olanzapine, and quetiapine are this excess mortality is attributed to diabetes and cardiovas- shown to activate AMPK in the hypothalamus in animal cular disease (3); weight gain is a significant contributor to studies whereas other antipsychotic medications do not (4). -

Burning Mouth Syndrome 25/03/13 11:36
Burning Mouth Syndrome 25/03/13 11:36 Medscape Reference Reference News Reference Education MEDLINE Burning Mouth Syndrome Author: Vincent D Eusterman, MD, DDS; Chief Editor: Arlen D Meyers, MD, MBA more... Updated: Jan 26, 2012 Background Burning mouth syndrome (BMS) is an idiopathic condition characterized by a continuous burning sensation of the mucosa of the mouth, typically involving the tongue, with or without extension to the lips and oral mucosa. Classically, burning mouth syndrome (BMS) is accompanied by gustatory disturbances (dysgeusia, parageusia) and subjective xerostomia. By definition, no macroscopic alterations in oral mucosa are apparent. Burning mouth syndrome (BMS) occurs most frequently, but not exclusively, in peri-menopausal and postmenopausal women. See the following illustration. A 29-year-old female presents with tongue irritation. A diagnosis of benign migratory glossitis (geographic tongue) is made by the appearance. The portions of the tongue with atrophic filiform papilla are symptomatic to acidic foods. Burning mouth syndrome (BMS) is a clinical diagnosis made via the exclusion of all other causes. No universally accepted diagnostic criteria, laboratory tests, imaging studies or other modalities definitively diagnose or exclude burning mouth syndrome (BMS). Various attempts to classify burning mouth syndrome (BMS) based on etiology and symptoms have been made. In a classification by etiology or cause, idiopathic burning mouth syndrome (BMS) is considered “primary BMS” (or "true BMS"), whereas “secondary BMS” has an identifiable cause. For the purposes of this article, we will use these terms. Another classification of burning mouth syndrome (BMS) is based on symptoms, stratifying cases into 3 types, as follows:[1] Type 1 burning mouth syndrome (BMS): Patients have no symptoms upon waking, with progression throughout the day. -

Chronic Orofacial Pain: Burning Mouth Syndrome and Other Neuropathic
anagem n M e ai n t P & f o M l e Journal of a d n i c r i u n o e J Pain Management & Medicine Tait et al., J Pain Manage Med 2017, 3:1 Review Article Open Access Chronic Orofacial Pain: Burning Mouth Syndrome and Other Neuropathic Disorders Raymond C Tait1, McKenzie Ferguson2 and Christopher M Herndon2 1Saint Louis University School of Medicine, St. Louis, USA 2Southern Illinois University Edwardsville School of Pharmacy, Edwardsville, USA *Corresponding author: RC Tait, Department of Psychiatry, Saint Louis University School of Medicine,1438 SouthGrand, Boulevard, St Louis, MO-63104, USA, Tel: 3149774817; Fax: 3149774879; E-mail: [email protected] Recevied date: October 4, 2016; Accepted date: January 17, 2017, Published date: January 30, 2017 Copyright: © 2017 Raymond C Tait, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Chronic orofacial pain is a symptom associated with a wide range of neuropathic, neurovascular, idiopathic, and myofascial conditions that affect a significant proportion of the population. While the collective impact of the subset of the orofacial pain disorders involving neurogenic and idiopathic mechanisms is substantial, some of these are relatively uncommon. Hence, patients with these disorders can be vulnerable to misdiagnosis, sometimes for years, increasing the symptom burden and delaying effective treatment. This manuscript first reviews the decision tree to be followed in diagnosing any neuropathic pain condition, as well as the levels of evidence needed to make a diagnosis with each of several levels of confidence: definite, probable, or possible. -

Oral Pathology Unmasking Gastrointestinal Disease
Journal of Dental Health Oral Disorders & Therapy Review Article Open Access Oral pathology unmasking gastrointestinal disease Abstract Volume 5 Issue 5 - 2016 Different ggastrointestinal disorders, such as Gastroesophageal Reflux Disease (GERD), Celiac Disease (CD) and Crohn’s disease, may manifest with alterations of the oral cavity Fumagalli LA, Gatti H, Armano C, Caruggi S, but are often under and misdiagnosed both by physicians and dentists. GERD can cause Salvatore S dental erosions, which are the main oral manifestation of this disease, or other multiple Department of Pediatric, Università dell’Insubria, Italy affections involving both hard and soft tissues such as burning mouth, aphtous oral ulcers, Correspondence: Silvia Salvatore, Pediatric Department of erythema of soft palate and uvula, stomatitis, epithelial atrophy, increased fibroblast number Pediatric, Università dell’Insubria, Via F. Del Ponte 19, 21100 in chorion, xerostomia and drooling. CD may be responsible of recurrent aphthous stomatitis Varese, Italy, Tel 0039 0332 299247, Fax 0039 0332 235904, (RAS), dental enamel defects, delayed eruption of teeth, atrophic glossitis and angular Email chelitis. Crohn’s disease can occur with several oral manifestations like indurated tag-like lesions, clobbestoning, mucogingivitis or, less specifically, with RAS, angular cheilitis, Received: October 30, 2016 | Published: December 12, 2016 reduced salivation, halitosis, dental caries and periodontal involvement, candidiasis, odynophagia, minor salivary gland enlargement, perioral -

(12) Patent Application Publication (10) Pub. No.: US 2011/0236506 A1 SCHWARTZ Et Al
US 2011 0236506A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0236506 A1 SCHWARTZ et al. (43) Pub. Date: Sep. 29, 2011 (54) PHARMACEUTICAL ASSOCIATION Publication Classification CONTAINING LIPOCACID AND (51) Int. Cl. HYDROXYCTRIC ACIDAS ACTIVE A633/24 (2006.01) INGREDIENTS A63L/385 (2006.01) A63/685 (2006.01) (75) Inventors: Laurent SCHWARTZ, Paris (FR): A63/4985 (2006.01) Adeline GUAIS-VERGNE, A63L/7056 (2006.01) Draveil (FR) A6IP35/00 (2006.01) (73) Assignees: Laurent SCHWARTZ, Paris (FR): (52) U.S. Cl. ........... 424/649; 514/440; 514/77: 514/249; BIOREBUS, Paris (FR) 514/52 (21) Appl. No.: 13/099,897 (57) ABSTRACT Pharmaceutical combination containing lipoic acid and (22) Filed: May 3, 2011 hydroxycitric acid as active ingredients. The present inven tion relates to a novel pharmaceutical combination and to the Related U.S. Application Data use thereof for producing a medicament having an antitumor (63) Continuation of application No. PCT/FR2009/ activity. According to the invention, this combination com 052110, filed on Nov. 2, 2009. prises, as active ingredients: lipoic acid or one of the pharma ceutically acceptable salts thereof, and hydroxycitric acid or (30) Foreign Application Priority Data one of the pharmaceutically acceptable salts thereof. Said active ingredients being formulated together or separately for Nov. 3, 2008 (FR) ....................................... O8574.48 a conjugated, simultaneous or separate use. Patent Application Publication Sep. 29, 2011 Sheet 1 of 9 US 2011/023650.6 A1 lipoic acid alone -29 f2 f Niger of ces i{t} v s 6 g i w 4. 6 8 i 2 Concentrations tumoi.i. -

Philadelphia
Saturday, April 18th, 2015 PCOS Awareness Symposium 2015 Philadelphia Polycystic Ovary Syndrome: Creating a Treatment Plan Katherine Sherif, MD Professor & Vice Chair, Department of Medicine Director, Jefferson Women’s Primary Care Thomas Jefferson University The Canary in the Coalmine . PCOS seems to accelerate the aging process . It is possible to reverse the aging process . Be scrupulous in your commitment to be healthy Multiple Systems . Reproductive . Endocrinologic . Cardiac . Renal (kidney) . Hepatic (liver) . Brain (mood) . Dermatologic Multiple Signs & Symptoms Irregular periods, Bleeding too much, Bleeding too little, Anxiety, Depression, Eating disorders, Weight gain, Acanthosis nigricans, Skin tags, Follicular keratitis, Hirsutism, Acne, Alopecia, Excess sweating, Seborrheic dermatitis, Hidradenitis supparativa, Fatty liver, High triglycerides, low HDL-cholesterol, Elevated glucose, Infertility, Breastfeeding problems, Poor sleep, Miscarriages, Fatigue, Endometrial cancer Multiple Pathways GnRH pulsatility Theca cell LH Progesterone 17 - OH P testosterone estrone androstenedione & TGranulosa A* Estradiol X Follicle Peripheral conversion A* = aromatase More Pathways! GnRH Insulin pulsatility Theca cell LH Progesterone 17 - OH P testosterone estrone androstenedione testosterone estradiol X ↓ SHBG Free T X Follicle Peripheral conversion The Magic Bullet The oral contraceptive pill . High doses of estrogen (ethinyl estradiol) . Increase SHBG and lower free testosterone* . Improve skin symptoms in most: . Alopecia . -
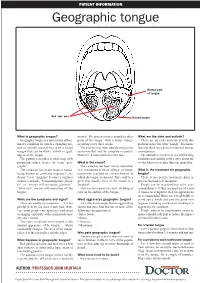
Geographic Tongue
PATIENT INFORMATION Geographic tongue Normal part of tongue Red ‘raw’ area Raised border What is geographic tongue? normal. The process moves around to other What are the risks and outlook? Geographic tongue is a non-serious inflam- parts of the tongue with a major change There are no risks associated with this matory condition in which a changing pat- occurring every three weeks. problem, hence the term “benign”. It is harm- tern of smooth red patches, with a raised The process may then subside and go into less and there have been no reported serious margin that can be white, yellow or grey, remission that may be complete or partial. consequences. appear on the tongue. However, it may return at a later time. The outlook is excellent. It is a self-limiting The pattern resembles a relief map with condition and usually settles after about six mountain ridges, hence the term “geo- What is the cause? weeks. However, it may flare up again later. graphic”. The cause has not been clearly identified. The condition has many medical names, It is considered to be an allergic or hyper- What is the treatment for geographic being known as erythema migrans (“ery- sensitivity reaction to certain factors to tongue? thema” = red, “migrans” because it migrates which the tongue is exposed. This could be a There is no specific treatment, drug or or moves around), “benign migratory glossi- germ that usually lives in the mouth or a process that makes it disappear. tis” or “benign inflammatory glossitis”. foodstuff. People can be reassured not to be con- “Glossitis” means inflammation of the This reaction causes excessive shedding of cerned about it.