Oral Lesions in Sjögren's Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

Guideline # 18 ORAL HEALTH
Guideline # 18 ORAL HEALTH RATIONALE Dental caries, commonly referred to as “tooth decay” or “cavities,” is the most prevalent chronic health problem of children in California, and the largest single unmet health need afflicting children in the United States. A 2006 statewide oral health needs assessment of California kindergarten and third grade children conducted by the Dental Health Foundation (now called the Center for Oral Health) found that 54 percent of kindergartners and 71 percent of third graders had experienced dental caries, and that 28 percent and 29 percent, respectively, had untreated caries. Dental caries can affect children’s growth, lead to malocclusion, exacerbate certain systemic diseases, and result in significant pain and potentially life-threatening infections. Caries can impact a child’s speech development, learning ability (attention deficit due to pain), school attendance, social development, and self-esteem as well.1 Multiple studies have consistently shown that children with low socioeconomic status (SES) are at increased risk for dental caries.2,3,4 Child Health Disability and Prevention (CHDP) Program children are classified as low socioeconomic status and are likely at high risk for caries. With regular professional dental care and daily homecare, most oral disease is preventable. Almost one-half of the low-income population does not obtain regular dental care at least annually.5 California children covered by Medicaid (Medi-Cal), ages 1-20, rank 41 out of all 50 states and the District of Columbia in receiving any preventive dental service in FY2011.6 Dental examinations, oral prophylaxis, professional topical fluoride applications, and restorative treatment can help maintain oral health. -
Benign Migratory Glossitis: Case Report and Literature Review
Volume 1- Issue 5 : 2017 DOI: 10.26717/BJSTR.2017.01.000482 Sarfaraz Khan. Biomed J Sci & Tech Res ISSN: 2574-1241 Case Report Open Access Benign Migratory Glossitis: Case Report and Literature Review Sarfaraz Khan1*, Syed AsifHaider Shah2, Tanveer Ahmed Mujahid3 and Muhammad Ishaq4 1Consultant Oral and Maxillofacial Surgeon, Pak Field Hospital Darfur, Sudan 2MDC Gujranwala, Pakistan 3Consultant Dermatologist, Pak Field Hospital Darfur, Sudan 4Registrar Dermatologist, Pak Field Hospital Darfur, Sudan Received: October 25, 2017; Published: October 31, 2017 *Corresponding author: Sarfaraz Khan, Consultant Oral and Maxillofacial Surgeon, Pakistan Field Hospital Darfur, Sudan, Tel: ; Email: Abstract Benign migratory Glossitis (BMG) is a benign, usually asymptomatic mucosal lesion of dorsal surface of the tongue, characterized by depapillated erythematous patches separated by white irregular borders. Etiology of BMG is unknown. Risk factors include psoriasis, fissured tongue, diabetes mellitus, hypersensitivity and psychological factors. We report BMG in an Egyptian soldier of UN peace keeping force, with stressKeywords: as a possible Geographic etiological tongue; factor Benign and migratory provide literature Glossitis; reviewErythema of this migrans disorder. Introduction Benign migratory Glossitis (BMG) is a benign, immune- spicy/salty food and/or alcoholic drinks [4,5].The lesion typically usually characterized by asymptomatic erythematous patches changes its shape with time owing to the change in pattern of mediated, chronic inflammatory lesion of unknown etiology, depapillation.Similar lesions may also be seen in atrophic candidiasis, local chemical or mechanical trauma, drug induced reactions, psoriasis with whitish margins across the surface of the tongue. This condition is also known as geographic tongue, erythema migrans, Treatment of symptomatic BMG aims at provision of symptomatic Glossitis exfoliativa and wandering rash of the tongue. -

Case Report Treatment of Geographic Tongue
Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2015; 2(7):409-413 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Treatment of Geographic Tongue Superimposing Fissured Tongue: A literature review with case report Jalaleddin H Hamissi1, Mahsa EsFehani2, Zahra Hamissi3 1Associate Professor in periodontics and Dental Caries Prevention Research Center, Qazvin University Medical Sciences, Qazvin, Iran. 2Assistant Professor, Department of Oral Medicine & Diagnosis, college dentistry, Qazvin University Medical Sciences, Qazvin, Iran. 3Dental Student, College of Dentistry, Shahied Behesti University of Medical Sciences, Teheran, Iran *Corresponding author Dr Jalaleddin H Hamissi Email: [email protected] ; [email protected] Abstract: Tongue is a most sensitive part of the oral cavity. It is responsible for many functions in the mouth like swallowing, speech, mastication, speaking and breathing. Geographic tongue (Benign migratory glossitis, erythema migrans) is an asymptomatic inflammatory disorder of tongue with controversial etiology. This disease is characterized by erythematous areas showing raised greyish or white circinate lines or bands with irregular pattern on the dorsal surface of the tongue and depapillation. The objective in presenting the case report and literature review is to discuss the clinical presentation, associated causative factors and management strategies of geographic tongue. Keywords: Asymptomatic; Characteristics; Fissured tongue; Geographic tongue; Migratory INTRODUCTION in approximately three percent (3%) majority of female Geographic tongue is an asymptomatic population [9]. On other aspects of oral mucosa, such as inflammatory condition of the dorsum of tongue on commissure of lip, floor of mouth, cheek etc., which occasionally extending towards the lateral borders. -
Addisonian Pigmentation of the Oral Mucosa
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Addisonian Pigmentation of the Oral Mucosa Samir S. Shah, MD; Catherine H. Oh, MD; Susan E. Coffin, MD, MPH; Albert C. Yan, MD Cutaneous pigmentation is a hallmark of Addison Free thyroxine and thyrotropin levels were within disease. When present, the hyperpigmentation reference range. generally localizes to sun-exposed surfaces. This case highlights a less well-recognized Comment cutaneous feature that is pathognomonic for the Addison disease, a chronic primary insufficiency of disease: oral mucous membrane hyperpigmenta- the adrenal glands, results in both glucocorticoid and tion. We describe this unique type of discolor- mineralocorticoid deficiency. Historically, tuberculo- ation in detail and contrast it with other forms of sis accounted for most cases of Addison disease.1 oral pigmentation. Autoimmune destruction of the adrenal glands, also Cutis. 2005;76:97-99. known as autoimmune adrenalitis, is now the most common cause of Addison disease in both children and adults.2,3 Autoimmune destruction of other Case Report endocrine tissues can occur concurrently. These A 9-year-old girl presented with a 4-month history polyglandular autoimmune syndromes are associated of painless black patches on the tongue and gingiva. with hypoparathyroidism, pernicious anemia, and The patches had persisted despite treatment with chronic mucocutaneous candidiasis (type 1); diabetes oral fluconazole, which had been prescribed empiri- mellitus (type 2); or thyroiditis (type 3).4 Type 3, cally for presumed oral candidiasis. Results of a phys- however, consists of an autoimmune thyroiditis ical examination revealed scattered, asymptomatic, syndrome in the absence of Addison disease.5 bluish-black macules on the dorsal surface of the Although most children (75%) presenting with isolated tongue, the mucosal surface of the lower lip, and the Addison disease are boys,6 type 1 autoimmune poly- hard palate (Figure). -

The OHNEP Interprofessional Oral Health Faculty Toolkit
The OHNEP Interprofessional Oral Health Faculty Toolkit Adult-Gerontology Nurse Practitioner Program CURRICULUM INTEGRATION OF INTERPROFESSIONAL ORAL HEALTH CORE COMPETENCIES: • Adult-Gerontology Health Assessment • Adult-Gerontology Health Promotion • Adult-GerontologyPrimary Care • Resources © Oral Health Nursing Education and Practice (OHNEP) INTRODUCTION The Oral Health Nursing Education and Practice (OHNEP) program has developed an Interprofessional Oral Health Faculty Tool Kit to S! provide you with user friendly curriculum templates and teaching-learning resources to use when integrating oral health and its links to ! overall health in your Adult-Gerontology Nurse Practitioner program. ! Oral health and its relation to overall health has been identified as an important population health issue. Healthy People 2020 (2011), the IOM Reports, Advancing Oral Health in America (2011) and Building Workforce Capacity in Oral Health (2011), as well as the IPEC Competencies ! (2011), challenged HRSA to develop interprofessional oral health core competencies for primary care providers. Publication of the report, ! Integrating Oral Health in Primary Care Practice (2014), reflects those interprofessional oral health competencies that can be used by Adult- Gerontology Nurse Practitioners for faculty development, curriculum integration and establishment of “best practices” in clinical settings. ! The HRSA interprofessional oral health core competencies, the IPEC competencies and the NONPF core competencies provide the framework for the curriculum templates and resources. Exciting teaching-learning strategies that take students from Exposure to Immersion to Competence can begin in the classroom, link to simulated or live clinical experiences and involve community-based service learning, advocacy and policy initiatives as venues you can readily use to integrate oral health into your existing primary care curriculum. -

Adverse Effects of Medications on Oral Health
Adverse Effects of Medications on Oral Health Dr. James Krebs, BS Pharm, MS, PharmD Director of Experiential Education College of Pharmacy, University of New England Presented by: Rachel Foster PharmD Candidate, Class of 2014 University of New England October 2013 Objectives • Describe the pathophysiology of various medication-related oral reactions • Recognize the signs and symptoms associated with medication-related oral reactions • Identify the populations associated with various offending agents • Compare the treatment options for medication-related oral reactions Medication-related Oral Reactions • Stomatitis • Oral Candidiasis • Burning mouth • Gingival hyperplasia syndrome • Alterations in • Glossitis salivation • Erythema • Alterations in taste Multiforme • Halitosis • Oral pigmentation • Angioedema • Tooth discoloration • Black hairy tongue Medication-related Stomatitis • Clinical presentation – Aphthous-like ulcers, mucositis, fixed-drug eruption, lichen planus1,2 – Open sores in the mouth • Tongue, gum line, buccal membrane – Patient complaint of soreness or burning http://www.virtualmedicalcentre.com/diseases/oral-mucositis-om/92 0 http://www.virtualmedicalcentre.com/diseases/oral-mucositis-om/920 Medication-related Stomatitis • Offending agents1,2 Medication Indication Patient Population Aspirin •Heart health • >18 years old •Pain reliever • Cardiac patients NSAIDs (i.e. Ibuprofen, •Headache General population naproxen) •Pain reliever •Fever reducer Chemotherapy (i.e. •Breast cancer •Oncology patients methotrexate, 5FU, •Colon -
A Concise Guide to Treating Painful Oral Lesions
Drugs Used to Treat Osteoporosis and Bone Cancer Perio & Implant Centers The Team for of the Monterey Bay (831) 648-8800 Jochen P. Pechak, DDS, MSD in Silicon Valley (408) 738-3423 Which May Cause Osteonecrosis of the Jaws mobile: www.DrPechakapp.com he many bisphosphonates and monoclonal antibodies which are used to treat osteoporosis and bone cancer often web: GumsRus.com causeDrugsDrugs osteonecrosis Used Used of the to jaws.to Treat AsTreat dental clinicians,Osteoporosis Osteoporosis it is important that and andwe are Bone awareBone of this Cancers Cancers side effect before Ttreating our patients who are taking these drugs. The tables below summarize these drugs, the route these drugs are administered, andWhich Whichtheir likelihood May May of causing Cause Cause osteonecrosis Osteonecrosis Osteonecrosis of the jaws as reported byof of Dr. the theRobert Jaws JawsMarx at the University of Miami Division of Oral and Maxillofacial Surgery. PDL tm Osteoporosis Drugs Drugs Osteoporosis Used to Treat Drugs Osteoporosis PerioDontaLetter Jochen P. Pechak, DDS, MSD, Periodontics and Implant Dentistry Spring DrugDrug ClassificationClassification ActionAction DoseDose RouteRoute %% of of ReportedReported CasesCases of of OsteonecrosisOsteonecrosis AlendronateAlendronate BisphosphonateBisphosphonate OsteoclastOsteoclast 7070 mg/wk mg/wk OralOral 8282%% From Our Office A Concise Guide to Treating (Fosamax(Fosamax ToxicityToxicity to Yours... Generic)Generic) Painful Oral Lesions ResidronateResidronate BisphosphonateBisphosphonate OsteoclastOsteoclast 3535 mg/wk mg/wk OralOral 1%1% As dentists specializing in treat- (Actonel Toxicity (Actonel Toxicity ment of diseases of the oral cavity atients present frequently with Treating Cold Sores Atelvia)Atelvia) and associated structures, we are painful oral lesions. They are often also called upon to treat pain- IbandronateIbandronate BisphosphonateBisphosphonate OsteoclastOsteoclast 150150 mg/mos mg/mos OralOral 1%1% usually not serious, but patients And Canker Sores (Boniva) Toxicity IV ful oral lesions in the mouth. -
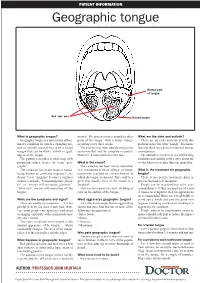
Geographic Tongue
PATIENT INFORMATION Geographic tongue Normal part of tongue Red ‘raw’ area Raised border What is geographic tongue? normal. The process moves around to other What are the risks and outlook? Geographic tongue is a non-serious inflam- parts of the tongue with a major change There are no risks associated with this matory condition in which a changing pat- occurring every three weeks. problem, hence the term “benign”. It is harm- tern of smooth red patches, with a raised The process may then subside and go into less and there have been no reported serious margin that can be white, yellow or grey, remission that may be complete or partial. consequences. appear on the tongue. However, it may return at a later time. The outlook is excellent. It is a self-limiting The pattern resembles a relief map with condition and usually settles after about six mountain ridges, hence the term “geo- What is the cause? weeks. However, it may flare up again later. graphic”. The cause has not been clearly identified. The condition has many medical names, It is considered to be an allergic or hyper- What is the treatment for geographic being known as erythema migrans (“ery- sensitivity reaction to certain factors to tongue? thema” = red, “migrans” because it migrates which the tongue is exposed. This could be a There is no specific treatment, drug or or moves around), “benign migratory glossi- germ that usually lives in the mouth or a process that makes it disappear. tis” or “benign inflammatory glossitis”. foodstuff. People can be reassured not to be con- “Glossitis” means inflammation of the This reaction causes excessive shedding of cerned about it. -

On the Tip of the Tongue
KNOWLEDGE TO PRACTICE DES CONNAISSANCES ÀLA PRATIQUE Diagnostic Challenge On the tip of the tongue . Rachel Orchard, MD*; Sheena Belisle, MD†; Rodrick Lim, MD†‡ Keywords: pediatric, rash, tongue, vesicle right-sided wheeze. Cardiovascular, abdominal, and neurological (including cranial nerve) examinations were unremarkable. CASE HISTORY What is the most likely diagnosis? A 14-year-old male presented to the pediatric emer- a) Drug eruption gency department (ED) with a chief complaint of b) Varicella zoster virus (VZV) changes to his tongue. He described a 3-day history of a c) Oral candidiasis gradually worsening sore, swollen tongue associated with a white plaque. This was accompanied by a 3-day d) Epstein-Barr virus history of a gradually worsening left-sided facial rash e) Oral lichen planus that had an intermittent mild tingling sensation. He also had a 1-week history of a productive cough with yellow mucus and generalized malaise. He had been seen at a walk-in clinic 2 days prior to presentation and was prescribed amoxicillin for presumed pneumo- nia, which he began the same day. He denied any history of fevers, facial weakness, neck stiffness, or eye symptoms. He was an otherwise well child, with up-to-date immunizations and a past medical history of chickenpox and recurrent furuncles as a younger child. On examination, he appeared well with the following vital signs: blood pressure 122/64 mm Hg, heart rate 73 beats per minute, respiratory rate 18 breaths per minute, temperature 36.8°C, and oxygen saturation of 99% on room air. Examination of his tongue revealed a symmetric white plaque along with ulcerative lesions on the left tongue and buccal mucosa (Figure 1). -

Oral Manifestations of a Possible New Periodic Fever Syndrome Soraya Beiraghi, DDS, MSD, MS, MSD1 • Sandra L
PEDIATRIC DENTISTRY V 29 / NO 4 JUL / AUG 07 Case Report Oral Manifestations of a Possible New Periodic Fever Syndrome Soraya Beiraghi, DDS, MSD, MS, MSD1 • Sandra L. Myers, DMD2 • Warren E. Regelmann, MD3 • Scott Baker, MD, MS4 Abstract: Periodic fever syndrome is composed of a group of disorders that present with recurrent predictable episodes of fever, which may be accompanied by: (1) lymphadenopathy; (2) malaise; (3) gastrointestinal disturbances; (4) arthralgia; (5) stomatitis; and (6) skin lesions. These signs and symptoms occur in distinct intervals every 4 to 6 weeks and resolve without any residual effect, and the patient remains healthy between attacks. The evaluation must exclude: (1) infections; (2) neoplasms; and (3) autoimmune conditions. The purpose of this paper is to report the case of a 4½- year-old white female who presented with a history of periodic fevers accompanied by: (1) joint pain; (2) skin lesions; (3) rhinitis; (4) vomiting; (5) diarrhea; and (6) an unusual asymptomatic, marked, fi ery red glossitis with features evolving to resemble geographic tongue and then resolving completely between episodes. This may represent the fi rst known reported case in the literature of a periodic fever syndrome presenting with such unusual recurring oral fi ndings. (Pediatr Dent 2007;29:323-6) KEYWORDS: PERIODIC FEVER, MOUTH LESIONS, GEOGRAPHIC TONGUE, STOMATITIS The diagnosis of periodic fever syndrome is often challeng- low, mildly painful ulcerations, which vary in number, and ing in children. Periodic fever syndrome is composed -

Hairy Tongue, Geographic Tongue, Scrotal Tongue and Systemic Connections: Clinical Images and an Overview
CASE REPORT Hairy tongue, geographic tongue, scrotal tongue and systemic connections: clinical images and an overview Cinzia Casu, DDS1, Maria Giulia Nosotti, RDH2, Antonia Sinesi, RDH2, Giovanna Mosaico, RDH2 Casu C, Nosotti MG, Sinesi A, et al. Hairy tongue, geographic tongue, condition, predominantly asymptomatic. Clinically, it is characterized by scrotal tongue and systemic connections: clinical images and an overview. fissures with a depth of up to 6 mm that extend along the dorsal and/or Dentist Case Rep. 2019;3(1):01-03. lateral sides of the tongue. These benign entities are connected with systemic disease (psoriasis, diabetes, hypertension and GT; tumors, radiant therapies ABSTRACT and BHT; fungal infections and Merkesson-Rosenthal syndrome and ST). Black Hairy Tongue (BHT) is a benign condition, caused by a defect of keratin Although an association between elevated IgE and migrant glossitis has desquamation over lingual papillae and its discoloration is caused by the been documented, associations between the three lingual conditions and the presence of porphyrin-producing chromogenic bacteria or yeast. Geographic presence of allergy are unclear. We would like to present a case in which the Tongue (GT) is characterized by a central erythematous zone consisting of 3 conditions were present in the same tongue of a female patient with allergic atrophy of the filiform papillae, whereas the white zone shows regenerating rhinitis and calcium deficiency. filiform papillae along with keratin. Scrotal Tongue (ST) is a common Key Words: Geographic tongue; scrotal tongue; black hairy tongue he tongue is considered the most complex organ of the body and a very Scrotal Tongue (ST) is a frequent condition in the population, Timportant structure in the oral cavity.