A Concise Guide to Treating Painful Oral Lesions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

Guideline # 18 ORAL HEALTH
Guideline # 18 ORAL HEALTH RATIONALE Dental caries, commonly referred to as “tooth decay” or “cavities,” is the most prevalent chronic health problem of children in California, and the largest single unmet health need afflicting children in the United States. A 2006 statewide oral health needs assessment of California kindergarten and third grade children conducted by the Dental Health Foundation (now called the Center for Oral Health) found that 54 percent of kindergartners and 71 percent of third graders had experienced dental caries, and that 28 percent and 29 percent, respectively, had untreated caries. Dental caries can affect children’s growth, lead to malocclusion, exacerbate certain systemic diseases, and result in significant pain and potentially life-threatening infections. Caries can impact a child’s speech development, learning ability (attention deficit due to pain), school attendance, social development, and self-esteem as well.1 Multiple studies have consistently shown that children with low socioeconomic status (SES) are at increased risk for dental caries.2,3,4 Child Health Disability and Prevention (CHDP) Program children are classified as low socioeconomic status and are likely at high risk for caries. With regular professional dental care and daily homecare, most oral disease is preventable. Almost one-half of the low-income population does not obtain regular dental care at least annually.5 California children covered by Medicaid (Medi-Cal), ages 1-20, rank 41 out of all 50 states and the District of Columbia in receiving any preventive dental service in FY2011.6 Dental examinations, oral prophylaxis, professional topical fluoride applications, and restorative treatment can help maintain oral health. -

ABC of Oral Health Periodontal Disease John Coventry, Gareth Griffiths, Crispian Scully, Maurizio Tonetti
Clinical review ABC of oral health Periodontal disease John Coventry, Gareth Griffiths, Crispian Scully, Maurizio Tonetti Most periodontal disease arises from, or is aggravated by, accumulation of plaque, and periodontitis is associated particularly with anaerobes such as Porphyromonas gingivalis, Bacteroides forsythus, and Actinobacillus actinomycetemcomitans. Calculus (tartar) may form from calcification of plaque above or below the gum line, and the plaque that collects on calculus exacerbates the inflammation. The inflammatory reaction is associated with progressive loss of periodontal ligament and alveolar bone and, eventually, with mobility and loss of teeth. Periodontal diseases are ecogenetic in the sense that, in subjects rendered susceptible by genetic or environmental factors (such as polymorphisms in the gene for interleukin 1, cigarette smoking, immune depression, and diabetes), the infection leads to more rapidly progressive disease. Osteoporosis also seems to have some effect on periodontal bone loss. The possible effects of periodontal disease on systemic Chronic marginal gingivitis showing erythematous oedematous appearance health, via pro-inflammatory cytokines, have been the focus of much attention. Studies to test the strength of associations with atherosclerosis, hypertension, coronary heart disease, cerebrovascular disease, and low birth weight, and any effects on diabetic control, are ongoing. Gingivitis Chronic gingivitis to some degree affects over 90% of the population. If treated, the prognosis is good, but otherwise it may progress to periodontitis and tooth mobility and loss. Marginal gingivitis is painless but may manifest with bleeding from the gingival crevice, particularly when brushing the teeth. The gingival margins are slightly red and swollen, eventually with mild gingival hyperplasia. Management—Unless plaque is assiduously removed and Gingivitis with hyperplasia kept under control by tooth brushing and flossing and, where necessary, by removal of calculus by scaling and polishing by dental staff, the condition will recur. -

Oral Lesions in Sjögren's Syndrome
Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Oral lesions in Sjögren’s syndrome patients Journal section: Oral Medicine and Pathology doi:10.4317/medoral.22286 Publication Types: Review http://dx.doi.org/doi:10.4317/medoral.22286 Oral lesions in Sjögren’s syndrome: A systematic review Julia Serrano 1, Rosa-María López-Pintor 1, José González-Serrano 1, Mónica Fernández-Castro 2, Elisabeth Casañas 1, Gonzalo Hernández 1 1 Department of Oral Medicine and Surgery, School of Dentistry, Complutense University, Madrid, Spain 2 Rheumatology Service, Hospital Infanta Sofía, Madrid, Spain Correspondence: Departamento de Especialidades Clínicas Odontológicas Facultad de Odontología Universidad Complutense de Madrid Plaza Ramón y Cajal s/n, 28040 Madrid. Spain [email protected] Serrano J, López-Pintor RM, González-Serrano J, Fernández-Castro M, Casañas E, Hernández G. Oral lesions in Sjögren’s syndrome: A system- atic review. Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Received: 18/11/2017 http://www.medicinaoral.com/medoralfree01/v23i4/medoralv23i4p391.pdf Accepted: 09/05/2018 Article Number: 22291 http://www.medicinaoral.com/ © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: [email protected] Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Médico Español Abstract Background: Sjögren’s syndrome (SS) is an autoimmune disease related to two common symptoms: dry mouth and eyes. Although, xerostomia and hyposialia have been frequently reported in these patients, not many studies have evaluated other oral manifestations. -
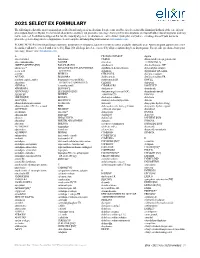
2021 SELECT EX FORMULARY the Following Is a List of the Most Commonly Prescribed Brand and Generic Medications
2021 SELECT EX FORMULARY The following is a list of the most commonly prescribed brand and generic medications. It represents an abbreviated version of the formulary list that is at the core of your prescription drug benefit plan. The list is not all-inclusive and does not guarantee coverage. Some preferred medications overlap with other clinical programs and may not be covered. In addition to drugs on this list, the majority of generic medications are covered under your plan and you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. Search complete formulary drug information at elixirsolutions.com. PLEASE NOTE: Preferred brand drugs may move to non-preferred status if a generic version becomes available during the year. Any medication approved to enter the market will not be covered until reviewed by Elixir. Not all drugs listed are covered by all prescription drug benefit programs. For specific questions about your coverage, please visit elixirsolutions.com. A B CILOXAN OINTMENT digoxin abacavir tablet balsalazide CIMDUO diltiazem ER (except generics for abacavir-lamivudine BAQSIMI cinacalcet CARDIZEM LA) ABILIFY MAINTENA [INJ] BASAGLAR [INJ] ciprofloxacin dimethyl fumarate DR* abiraterone* BD ULTRAFINE INSULIN SYRINGES ciprofloxacin-dexamethasone diphenoxylate-atropine acetic acid & NEEDLES citalopram dipyridamole ER-aspirin acitretin BELBUCA CITRANATAL divalproex sodium ACUVAIL BELSOMRA clarithromycin divalproex sodium ER acyclovir capsule, tablet benzonatate (except NDCs: clarithromycin ER DIVIGEL -
Addisonian Pigmentation of the Oral Mucosa
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Addisonian Pigmentation of the Oral Mucosa Samir S. Shah, MD; Catherine H. Oh, MD; Susan E. Coffin, MD, MPH; Albert C. Yan, MD Cutaneous pigmentation is a hallmark of Addison Free thyroxine and thyrotropin levels were within disease. When present, the hyperpigmentation reference range. generally localizes to sun-exposed surfaces. This case highlights a less well-recognized Comment cutaneous feature that is pathognomonic for the Addison disease, a chronic primary insufficiency of disease: oral mucous membrane hyperpigmenta- the adrenal glands, results in both glucocorticoid and tion. We describe this unique type of discolor- mineralocorticoid deficiency. Historically, tuberculo- ation in detail and contrast it with other forms of sis accounted for most cases of Addison disease.1 oral pigmentation. Autoimmune destruction of the adrenal glands, also Cutis. 2005;76:97-99. known as autoimmune adrenalitis, is now the most common cause of Addison disease in both children and adults.2,3 Autoimmune destruction of other Case Report endocrine tissues can occur concurrently. These A 9-year-old girl presented with a 4-month history polyglandular autoimmune syndromes are associated of painless black patches on the tongue and gingiva. with hypoparathyroidism, pernicious anemia, and The patches had persisted despite treatment with chronic mucocutaneous candidiasis (type 1); diabetes oral fluconazole, which had been prescribed empiri- mellitus (type 2); or thyroiditis (type 3).4 Type 3, cally for presumed oral candidiasis. Results of a phys- however, consists of an autoimmune thyroiditis ical examination revealed scattered, asymptomatic, syndrome in the absence of Addison disease.5 bluish-black macules on the dorsal surface of the Although most children (75%) presenting with isolated tongue, the mucosal surface of the lower lip, and the Addison disease are boys,6 type 1 autoimmune poly- hard palate (Figure). -

Generalized Aggressive Periodontitis Associated with Plasma Cell Gingivitis Lesion: a Case Report and Non-Surgical Treatment
Clinical Advances in Periodontics; Copyright 2013 DOI: 10.1902/cap.2013.130050 Generalized Aggressive Periodontitis Associated With Plasma Cell Gingivitis Lesion: A Case Report and Non-Surgical Treatment * Andreas O. Parashis, Emmanouil Vardas, † Konstantinos Tosios, ‡ * Private practice limited to Periodontics, Athens, Greece; and, Department of Periodontology, School of Dental Medicine, Tufts University, Boston, MA, United States of America. †Clinic of Hospital Dentistry, Dental Oncology Unit, University of Athens, Greece. ‡ Private practice limited to Oral Pathology, Athens, Greece. Introduction: Plasma cell gingivitis (PCG) is an unusual inflammatory condition characterized by dense, band-like polyclonal plasmacytic infiltration of the lamina propria. Clinically, appears as gingival enlargement with erythema and swelling of the attached and free gingiva, and is not associated with any loss of attachment. The aim of this report is to present a rare case of severe generalized aggressive periodontitis (GAP) associated with a PCG lesion that was successfully treated and maintained non-surgically. Case presentation: A 32-year-old white male with a non-contributory medical history presented with gingival enlargement with diffuse erythema and edematous swelling, predominantly around teeth #5-8. Clinical and radiographic examination revealed generalized severe periodontal destruction. A complete blood count and biochemical tests were within normal limits. Histological and immunohistochemical examination were consistent with PCG. A diagnosis of severe GAP associated with a PCG lesion was assigned. Treatment included elimination of possible allergens and non- surgical periodontal treatment in combination with azithromycin. Clinical examination at re-evaluation revealed complete resolution of gingival enlargement, erythema and edema and localized residual probing depths 5 mm. One year post-treatment the clinical condition was stable. -

The OHNEP Interprofessional Oral Health Faculty Toolkit
The OHNEP Interprofessional Oral Health Faculty Toolkit Adult-Gerontology Nurse Practitioner Program CURRICULUM INTEGRATION OF INTERPROFESSIONAL ORAL HEALTH CORE COMPETENCIES: • Adult-Gerontology Health Assessment • Adult-Gerontology Health Promotion • Adult-GerontologyPrimary Care • Resources © Oral Health Nursing Education and Practice (OHNEP) INTRODUCTION The Oral Health Nursing Education and Practice (OHNEP) program has developed an Interprofessional Oral Health Faculty Tool Kit to S! provide you with user friendly curriculum templates and teaching-learning resources to use when integrating oral health and its links to ! overall health in your Adult-Gerontology Nurse Practitioner program. ! Oral health and its relation to overall health has been identified as an important population health issue. Healthy People 2020 (2011), the IOM Reports, Advancing Oral Health in America (2011) and Building Workforce Capacity in Oral Health (2011), as well as the IPEC Competencies ! (2011), challenged HRSA to develop interprofessional oral health core competencies for primary care providers. Publication of the report, ! Integrating Oral Health in Primary Care Practice (2014), reflects those interprofessional oral health competencies that can be used by Adult- Gerontology Nurse Practitioners for faculty development, curriculum integration and establishment of “best practices” in clinical settings. ! The HRSA interprofessional oral health core competencies, the IPEC competencies and the NONPF core competencies provide the framework for the curriculum templates and resources. Exciting teaching-learning strategies that take students from Exposure to Immersion to Competence can begin in the classroom, link to simulated or live clinical experiences and involve community-based service learning, advocacy and policy initiatives as venues you can readily use to integrate oral health into your existing primary care curriculum. -

Adverse Effects of Medications on Oral Health
Adverse Effects of Medications on Oral Health Dr. James Krebs, BS Pharm, MS, PharmD Director of Experiential Education College of Pharmacy, University of New England Presented by: Rachel Foster PharmD Candidate, Class of 2014 University of New England October 2013 Objectives • Describe the pathophysiology of various medication-related oral reactions • Recognize the signs and symptoms associated with medication-related oral reactions • Identify the populations associated with various offending agents • Compare the treatment options for medication-related oral reactions Medication-related Oral Reactions • Stomatitis • Oral Candidiasis • Burning mouth • Gingival hyperplasia syndrome • Alterations in • Glossitis salivation • Erythema • Alterations in taste Multiforme • Halitosis • Oral pigmentation • Angioedema • Tooth discoloration • Black hairy tongue Medication-related Stomatitis • Clinical presentation – Aphthous-like ulcers, mucositis, fixed-drug eruption, lichen planus1,2 – Open sores in the mouth • Tongue, gum line, buccal membrane – Patient complaint of soreness or burning http://www.virtualmedicalcentre.com/diseases/oral-mucositis-om/92 0 http://www.virtualmedicalcentre.com/diseases/oral-mucositis-om/920 Medication-related Stomatitis • Offending agents1,2 Medication Indication Patient Population Aspirin •Heart health • >18 years old •Pain reliever • Cardiac patients NSAIDs (i.e. Ibuprofen, •Headache General population naproxen) •Pain reliever •Fever reducer Chemotherapy (i.e. •Breast cancer •Oncology patients methotrexate, 5FU, •Colon -

Making an Elderberry Syrup Or Elixir
Making an Elderberry Syrup or Elixir Herbal syrups are water extractions of herbs (usually decoctions—see below) that are concentrated with a sweetener (preferably organic white sugar or raw honey). This sweetener provides a bit of nutritional support as a carbohydrate and also acts as a preservative. The concentration of sugar is particularly important when making syrups and elixirs; when in water, sugar acts as a food source for micro-organisms (especially molds and yeasts). However, at a high enough concentration, the sugar actually restricts the growth ability of micro-organisms. So we are aiming to get our syrup to be saturated enough to preserve, but not so saturated that the sugar overwhelms the liquid and causes crystallization. When preparing a syrup, one of the following ratios should be used: 1 part decoction : 1 part sweetener 1 part decoction : 2 parts sweetener I tend to follow the 1 part water : 1 part sweetener suggestion, as the 1 : 2 ratio is too sweet for me. But I have access to a refrigerator, which will also help with preservation. If you are keeping your syrup at room temperature, the 1:2 ratio is best. Syrups are a great, palatable method for delivery of herbal medicines (especially for children), and are also a great way to mask the flavor of less tasty tinctures--just combine the tincture and the syrup and you get the medicinal benefits of both. Preserving syrups with honey is also a great way to combine the medicinal benefits of the honey with the herbs that are being used. Do not give syrups preserved with honey to children under the age of one. -

Desquamative Gingivitis Desquamative Gingivitis
DOI: 10.5772/intechopen.69268 Provisional chapter Chapter 1 Desquamative Gingivitis Desquamative Gingivitis Hiroyasu Endo, Terry D. Rees, Hideo Niwa, HiroyasuKayo Kuyama, Endo, Morio Terry D.Iijima, Rees, Ryuuichi Hideo Niwa, KayoImamura, Kuyama, Takao Morio Kato, Iijima, Kenji Doi,Ryuuichi Hirotsugu Imamura, TakaoYamamoto Kato, and Kenji Takanori Doi, Hirotsugu Ito Yamamoto and TakanoriAdditional information Ito is available at the end of the chapter Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.69268 Abstract Desquamative gingivitis (DG) is characterized by erythematous, epithelial desquama‐ tion, erosion of the gingival epithelium, and blister formation on the gingiva. DG is a clinical feature of a variety of diseases or disorders. Most cases of DG are associated with mucocutaneous diseases, the most common ones being lichen planus, mucous membrane pemphigoid, and pemphigus vulgaris. Proper diagnosis of the underlying cause is important because the prognosis varies, depending on the disease. This chapter presents the underlying etiology that is most commonly associated with DG. The current literature on the diagnostic and management modalities of patients with DG is reviewed. Keywords: gingival diseases/pemphigus/pemphigoid, benign mucous membrane/lichen planus, oral/hypersensitivity/autoimmune diseases 1. Introduction Manifestations of desquamative gingivitis (DG) include erythematous gingiva, epithelial des‐ quamation, and erosion of the gingival epithelium, as well as blister formation on the gingiva [1, 2] (Figure 1). The DG lesions may be localized or generalized and may extend into the alveolar mucosa. Similar lesions are often found on the buccal mucosa, tongue, and palate in the oral cavity. The signs of DG are clearly different from those of dental plaque‐induced gingivitis. -

Slang Terms and Jargon Can Cause Medication Errors
Volume 19, Number 10 November/December 2005 Drugs & Therapy B � U � L � L � E � T � I � N MEDICATION SAFETY FORMULARY UPDATE The Pharmacy and Therapeutics Slang terms and jargon can Committee met October 18, 2005. 4 products were added in the Formulary cause medication errors and 2 were deleted. 1 dosage form was evaluated and designated nonformu- his month “Magic Mouthwash” ents. An allergy screen would not be lary and not available, and 2 drugs T was deleted from the Formulary done, unless the individual ingredients were evaluated, but not added. Criteria (see Formulary Update). The P&T are appreciated. for use were modifi ed for 3 drugs. Committee took this action for medica- Magic Mouthwash will no longer be tion safety reasons. This continues the dispensed at Shands UF because there ◆ ADDED policy of not allowing the use of non- is no evidence that it works better than specifi c terms for mixtures that have a plain saline rinse. Clozapine Tablets traditionally been used. This action follows the banning of (generic by IVAX) Terms like “Magic Mouthwash” are the term “Butt Paste” several years Glutaraldehyde 0.6% Solution slang, jargon, or coined phrases for ago. Like Magic Mouthwash, Butt Paste (compounded) mixtures that have a specifi c purpose. is a nonspecifi c mixture of ingredients. Levofl oxacin In this instance, the “magic” is pain The “Butt Paste” mixture contained (Levaquin® by Ortho McNeil)* reduction in patients who have muco- Questran Light® (cholestyramine) in sitis of the mouth. Mucositis is a very Aquaphor®. The theory is that the cho- Ondansetron Tablets ® painful condition in patients receiving lestyramine binds bile acids that may (Zofran by GlaxoSmithKline) aggressive cytotoxic chemotherapy.