On the Tip of the Tongue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NIH Medlineplus Magazine Winter 2010
Trusted Health Information from the National Institutes of Health ® NIHMedlineWINTER 2010 Plusthe magazine Plus, in this issue! • Treating “ Keep diverticulitis the beat” Healthy blood Pressure • Protecting Helps Prevent Heart disease Yourself from Shingles • Progress against Prostate cancer • Preventing Suicide in Young Adults • relieving the Model Heidi Klum joins The Heart Truth Pain of tMJ Campaign for women’s heart health. • The Real Benefits of Personalized Prevent Heart Medicine Disease Now! You can lower your risk. A publication of the NatioNal Institutes of HealtH and the frieNds of the NatioNal library of MediciNe FRIENDS OF THE NATIONAL LIBRARY OF MEDICINE Saying “Yes!” to Careers in Health Care ecently, the Friends of NLM was delighted to co-sponsor the fourth annual “Yes, I Can Be a Healthcare Professional” conference at Frederick Douglass Academy in Harlem. More than 2,300 students and parents from socioeconomically disadvantaged communities throughout the entire New York City metropolitan area convened for Rthe daylong session. It featured practical skills workshops, discussion groups, and exhibits from local educational institutions, health professional societies, community health services, and health information providers, including the National Library of Medicine (NLM). If you’ll pardon the expression, the enthusiasm among the attendees—current and future Photo: NLM Photo: healthcare professionals—was infectious! donald West King, M.d. fNlM chairman It was especially exciting to mix with some of the students from six public and charter high schools in Harlem and the South Bronx enrolled in the Science and Health Career Exploration Program. The program was created by Mentoring in Medicine, Inc., funded by the NLM and Let Us Hear co-sponsored by the Friends. -

Oral Lesions in Sjögren's Syndrome
Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Oral lesions in Sjögren’s syndrome patients Journal section: Oral Medicine and Pathology doi:10.4317/medoral.22286 Publication Types: Review http://dx.doi.org/doi:10.4317/medoral.22286 Oral lesions in Sjögren’s syndrome: A systematic review Julia Serrano 1, Rosa-María López-Pintor 1, José González-Serrano 1, Mónica Fernández-Castro 2, Elisabeth Casañas 1, Gonzalo Hernández 1 1 Department of Oral Medicine and Surgery, School of Dentistry, Complutense University, Madrid, Spain 2 Rheumatology Service, Hospital Infanta Sofía, Madrid, Spain Correspondence: Departamento de Especialidades Clínicas Odontológicas Facultad de Odontología Universidad Complutense de Madrid Plaza Ramón y Cajal s/n, 28040 Madrid. Spain [email protected] Serrano J, López-Pintor RM, González-Serrano J, Fernández-Castro M, Casañas E, Hernández G. Oral lesions in Sjögren’s syndrome: A system- atic review. Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Received: 18/11/2017 http://www.medicinaoral.com/medoralfree01/v23i4/medoralv23i4p391.pdf Accepted: 09/05/2018 Article Number: 22291 http://www.medicinaoral.com/ © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: [email protected] Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Médico Español Abstract Background: Sjögren’s syndrome (SS) is an autoimmune disease related to two common symptoms: dry mouth and eyes. Although, xerostomia and hyposialia have been frequently reported in these patients, not many studies have evaluated other oral manifestations. -
Benign Migratory Glossitis: Case Report and Literature Review
Volume 1- Issue 5 : 2017 DOI: 10.26717/BJSTR.2017.01.000482 Sarfaraz Khan. Biomed J Sci & Tech Res ISSN: 2574-1241 Case Report Open Access Benign Migratory Glossitis: Case Report and Literature Review Sarfaraz Khan1*, Syed AsifHaider Shah2, Tanveer Ahmed Mujahid3 and Muhammad Ishaq4 1Consultant Oral and Maxillofacial Surgeon, Pak Field Hospital Darfur, Sudan 2MDC Gujranwala, Pakistan 3Consultant Dermatologist, Pak Field Hospital Darfur, Sudan 4Registrar Dermatologist, Pak Field Hospital Darfur, Sudan Received: October 25, 2017; Published: October 31, 2017 *Corresponding author: Sarfaraz Khan, Consultant Oral and Maxillofacial Surgeon, Pakistan Field Hospital Darfur, Sudan, Tel: ; Email: Abstract Benign migratory Glossitis (BMG) is a benign, usually asymptomatic mucosal lesion of dorsal surface of the tongue, characterized by depapillated erythematous patches separated by white irregular borders. Etiology of BMG is unknown. Risk factors include psoriasis, fissured tongue, diabetes mellitus, hypersensitivity and psychological factors. We report BMG in an Egyptian soldier of UN peace keeping force, with stressKeywords: as a possible Geographic etiological tongue; factor Benign and migratory provide literature Glossitis; reviewErythema of this migrans disorder. Introduction Benign migratory Glossitis (BMG) is a benign, immune- spicy/salty food and/or alcoholic drinks [4,5].The lesion typically usually characterized by asymptomatic erythematous patches changes its shape with time owing to the change in pattern of mediated, chronic inflammatory lesion of unknown etiology, depapillation.Similar lesions may also be seen in atrophic candidiasis, local chemical or mechanical trauma, drug induced reactions, psoriasis with whitish margins across the surface of the tongue. This condition is also known as geographic tongue, erythema migrans, Treatment of symptomatic BMG aims at provision of symptomatic Glossitis exfoliativa and wandering rash of the tongue. -

Case Report Treatment of Geographic Tongue
Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2015; 2(7):409-413 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Treatment of Geographic Tongue Superimposing Fissured Tongue: A literature review with case report Jalaleddin H Hamissi1, Mahsa EsFehani2, Zahra Hamissi3 1Associate Professor in periodontics and Dental Caries Prevention Research Center, Qazvin University Medical Sciences, Qazvin, Iran. 2Assistant Professor, Department of Oral Medicine & Diagnosis, college dentistry, Qazvin University Medical Sciences, Qazvin, Iran. 3Dental Student, College of Dentistry, Shahied Behesti University of Medical Sciences, Teheran, Iran *Corresponding author Dr Jalaleddin H Hamissi Email: [email protected] ; [email protected] Abstract: Tongue is a most sensitive part of the oral cavity. It is responsible for many functions in the mouth like swallowing, speech, mastication, speaking and breathing. Geographic tongue (Benign migratory glossitis, erythema migrans) is an asymptomatic inflammatory disorder of tongue with controversial etiology. This disease is characterized by erythematous areas showing raised greyish or white circinate lines or bands with irregular pattern on the dorsal surface of the tongue and depapillation. The objective in presenting the case report and literature review is to discuss the clinical presentation, associated causative factors and management strategies of geographic tongue. Keywords: Asymptomatic; Characteristics; Fissured tongue; Geographic tongue; Migratory INTRODUCTION in approximately three percent (3%) majority of female Geographic tongue is an asymptomatic population [9]. On other aspects of oral mucosa, such as inflammatory condition of the dorsum of tongue on commissure of lip, floor of mouth, cheek etc., which occasionally extending towards the lateral borders. -

Oral Candidosis: Aetiology, Clinical Manifestations, Diagnosis and Management Birsay Gümrü Tarçın
MÜSBED 2011;1(2):140-148 Derleme / Review Oral Candidosis: Aetiology, Clinical Manifestations, Diagnosis and Management Birsay Gümrü Tarçın Marmara University Faculty of Dentistry, Department of Oral Diagnosis and Radiology, Istanbul-Turkey Ya zış ma Ad re si / Add ress rep rint re qu ests to: Birsay Gümrü Tarçın Marmara University Faculty of Dentistry, Department of Oral Diagnosis and Radiology, Büyükçiftlik Sok. No: 6 34365 Nişantaşı, Şişli, İstanbul-Turkey Telefon / Phone: +90-212-231-9120 Faks / Fax: +90-212-246-5247 Elekt ro nik pos ta ad re si / E-ma il add ress: [email protected] Ka bul ta ri hi / Da te of ac cep tan ce: 22 Ağustos 2011 / August 22, 2011 ÖZET ABS TRACT Oral kandidozis: Etiyoloji, klinik özellikler, tanı Oral candidosis: aetiology, clinical ve tedavi manifestations, diagnosis and management Oral kandidozis dişhekimliği pratiğinde en sık karşılaşılan fungal Oral candidosis is the most common fungal infection encountered enfeksiyondur. Birçok farklı klinik görünümde ortaya çıkabildi- in dental practice. Clinical diagnosis and management of oral ğinden, klinik tanı ve tedavisi genellikle zordur. Hastalık sıklıkla candidosis is usually complicated, because it is encountered in a sistemik rahatsızlığı olan spesifik hasta gruplarında ortaya çık- wide variety of clinical presentations. The disease often manifests maktadır. Bu nedenle, oral kandidozis tedavisi öncelikle predis- in specific patient groups that are systemically compromised. pozisyon yaratan durumların kapsamlı tetkikini içermelidir. Bu Therefore, the management should always cover a thorough derlemede sık karşılaşılan oral kandidal lezyonların etiyolojisi, investigation of underlying predisposing conditions. This klinik görünümü, tanı ve tedavi stratejileri kapsamlı bir şekilde review provides a comprehensive overview of the aetiology, gözden geçirilmektedir. -

HIV Infection and AIDS
G Maartens 12 HIV infection and AIDS Clinical examination in HIV disease 306 Prevention of opportunistic infections 323 Epidemiology 308 Preventing exposure 323 Global and regional epidemics 308 Chemoprophylaxis 323 Modes of transmission 308 Immunisation 324 Virology and immunology 309 Antiretroviral therapy 324 ART complications 325 Diagnosis and investigations 310 ART in special situations 326 Diagnosing HIV infection 310 Prevention of HIV 327 Viral load and CD4 counts 311 Clinical manifestations of HIV 311 Presenting problems in HIV infection 312 Lymphadenopathy 313 Weight loss 313 Fever 313 Mucocutaneous disease 314 Gastrointestinal disease 316 Hepatobiliary disease 317 Respiratory disease 318 Nervous system and eye disease 319 Rheumatological disease 321 Haematological abnormalities 322 Renal disease 322 Cardiac disease 322 HIV-related cancers 322 306 • HIV INFECTION AND AIDS Clinical examination in HIV disease 2 Oropharynx 34Neck Eyes Mucous membranes Lymph node enlargement Retina Tuberculosis Toxoplasmosis Lymphoma HIV retinopathy Kaposi’s sarcoma Progressive outer retinal Persistent generalised necrosis lymphadenopathy Parotidomegaly Oropharyngeal candidiasis Cytomegalovirus retinitis Cervical lymphadenopathy 3 Oral hairy leucoplakia 5 Central nervous system Herpes simplex Higher mental function Aphthous ulcers 4 HIV dementia Kaposi’s sarcoma Progressive multifocal leucoencephalopathy Teeth Focal signs 5 Toxoplasmosis Primary CNS lymphoma Neck stiffness Cryptococcal meningitis 2 Tuberculous meningitis Pneumococcal meningitis 6 -

Adverse Effects of Medications on Oral Health
Adverse Effects of Medications on Oral Health Dr. James Krebs, BS Pharm, MS, PharmD Director of Experiential Education College of Pharmacy, University of New England Presented by: Rachel Foster PharmD Candidate, Class of 2014 University of New England October 2013 Objectives • Describe the pathophysiology of various medication-related oral reactions • Recognize the signs and symptoms associated with medication-related oral reactions • Identify the populations associated with various offending agents • Compare the treatment options for medication-related oral reactions Medication-related Oral Reactions • Stomatitis • Oral Candidiasis • Burning mouth • Gingival hyperplasia syndrome • Alterations in • Glossitis salivation • Erythema • Alterations in taste Multiforme • Halitosis • Oral pigmentation • Angioedema • Tooth discoloration • Black hairy tongue Medication-related Stomatitis • Clinical presentation – Aphthous-like ulcers, mucositis, fixed-drug eruption, lichen planus1,2 – Open sores in the mouth • Tongue, gum line, buccal membrane – Patient complaint of soreness or burning http://www.virtualmedicalcentre.com/diseases/oral-mucositis-om/92 0 http://www.virtualmedicalcentre.com/diseases/oral-mucositis-om/920 Medication-related Stomatitis • Offending agents1,2 Medication Indication Patient Population Aspirin •Heart health • >18 years old •Pain reliever • Cardiac patients NSAIDs (i.e. Ibuprofen, •Headache General population naproxen) •Pain reliever •Fever reducer Chemotherapy (i.e. •Breast cancer •Oncology patients methotrexate, 5FU, •Colon -

Varicella (Chickenpox): Questions and Answers Q&A Information About the Disease and Vaccines
Varicella (Chickenpox): Questions and Answers Q&A information about the disease and vaccines What causes chickenpox? more common in infants, adults, and people with Chickenpox is caused by a virus, the varicella-zoster weakened immune systems. virus. How do I know if my child has chickenpox? How does chickenpox spread? Usually chickenpox can be diagnosed by disease his- Chickenpox spreads from person to person by direct tory and appearance alone. Adults who need to contact or through the air by coughing or sneezing. know if they’ve had chickenpox in the past can have It is highly contagious. It can also be spread through this determined by a laboratory test. Chickenpox is direct contact with the fluid from a blister of a per- much less common now than it was before a vaccine son infected with chickenpox, or from direct contact became available, so parents, doctors, and nurses with a sore from a person with shingles. are less familiar with it. It may be necessary to perform laboratory testing for children to confirm chickenpox. How long does it take to show signs of chickenpox after being exposed? How long is a person with chickenpox contagious? It takes from 10 to 21 days to develop symptoms after Patients with chickenpox are contagious for 1–2 days being exposed to a person infected with chickenpox. before the rash appears and continue to be conta- The usual time period is 14–16 days. gious through the first 4–5 days or until all the blisters are crusted over. What are the symptoms of chickenpox? Is there a treatment for chickenpox? The most common symptoms of chickenpox are rash, fever, coughing, fussiness, headache, and loss of appe- Most cases of chickenpox in otherwise healthy children tite. -

Oral Manifestations of Pemphigus Vulgaris
Journal of Clinical & Experimental Dermatology Research - Open Access Research Article OPEN ACCESS Freely available online doi:10.4172/2155-9554.1000112 Oral Manifestations of Pemphigus Vulgaris: Clinical Presentation, Differential Diagnosis and Management Antonio Bascones-Martinez1*, Marta Munoz-Corcuera2, Cristina Bascones-Ilundain1 and German Esparza-Gómez1 1DDS, PhD, Medicine and Bucofacial Surgery Department, Dental School, Complutense University of Madrid, Spain 2DDS, PhD Student, Medicine and Bucofacial Surgery Department, Dental School, Complutense University of Madrid, Spain Abstract Pemphigus vulgaris is a chronic autoimmune mucocutaneous disease characterized by the formation of intraepithelial blisters. It results from an autoimmune process in which antibodies are produced against desmoglein 1 and desmoglein 3, normal components of the cell membrane of keratinocytes. The first manifestations of pemphigus vulgaris appear in the oral mucosa in the majority of patients, followed at a later date by cutaneous lesions. The diagnosis is based on clinical findings and laboratory analyses, and it is usually treated by the combined administration of corticosteroids and immunosuppressants. Detection of the oral lesions can result in an earlier diagnosis. We review the oral manifestations of pemphigus vulgaris as well as the differential diagnosis, treatment, and prognosis of oral lesions in this uncommon disease. Keywords: Pemphigus; Oral mucosa; Autoimmune bullous disease and have a molecular weight of 130 and 160 KDa, respectively [1,7,9,13]. The binding of antibodies to desmoglein at mucosal or Introduction cutaneous level gives rise to the loss of cell adhesion, with separation of epithelial layers (acantholysis) and the consequent appearance of Pemphigus vulgaris (PV) is the most frequently observed blisters on skin or mucosae [1,3]. -

Hairy Leukoplakia James E
Marquette University e-Publications@Marquette School of Dentistry Faculty Research and Dentistry, School of Publications 5-5-2017 Hairy Leukoplakia James E. Cade Meharry Medical College School of Dentistry Richard P. Vinson Paul L Foster School of Medicine Jeff urB gess University of Washington School of Dental Medicine Sanjiv S. Agarwala Temple University Shool of Medicine Denis P. Lynch Marquette University, [email protected] See next page for additional authors Published version. Medscape Drugs & Diseases (May 5, 2017). Publisher link. © 2017 by WebMD LLC. Used with permission. Authors James E. Cade, Richard P. Vinson, Jeff urB gess, Sanjiv S. Agarwala, Denis P. Lynch, and Gary L. Stafford This blog post/website is available at e-Publications@Marquette: https://epublications.marquette.edu/dentistry_fac/252 Overview Background Oral hairy leukoplakia (OHL) is a disease of the mucosa first described in 1984. This pathology is associated with Epstein-Barr virus (EBV) and occurs mostly in people with HIV infection, both immunocompromised and immunocompetent, and can affect patients who are HIV negative.{ref1}{ref2} The first case in an HIV-negative patient was reported in 1999 in a 56-year-old patient with acute lymphocytic leukemia. Later, many cases were reported in heart, kidney, and bone marrow transplant recipients and patients with hematological malignancies.{ref3}{ref4} Pathophysiology The Epstein-Barr virus (EBV), a ubiquitous herpesvirus estimated to infect 90% of the world's population, is linked to a growing number of diseases, especially in immunocompromised hosts. Like all herpesviruses, EBV establishes a life-long, persistent infection of its host. The pathogenesis of hairy leukoplakia is clearly complex, potentially requiring a convergence of factors including EBV co-infection, productive EBV replication, EBV genetic evolution, expression of specific EBV "latent" genes, and immune escape. -
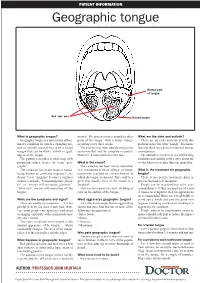
Geographic Tongue
PATIENT INFORMATION Geographic tongue Normal part of tongue Red ‘raw’ area Raised border What is geographic tongue? normal. The process moves around to other What are the risks and outlook? Geographic tongue is a non-serious inflam- parts of the tongue with a major change There are no risks associated with this matory condition in which a changing pat- occurring every three weeks. problem, hence the term “benign”. It is harm- tern of smooth red patches, with a raised The process may then subside and go into less and there have been no reported serious margin that can be white, yellow or grey, remission that may be complete or partial. consequences. appear on the tongue. However, it may return at a later time. The outlook is excellent. It is a self-limiting The pattern resembles a relief map with condition and usually settles after about six mountain ridges, hence the term “geo- What is the cause? weeks. However, it may flare up again later. graphic”. The cause has not been clearly identified. The condition has many medical names, It is considered to be an allergic or hyper- What is the treatment for geographic being known as erythema migrans (“ery- sensitivity reaction to certain factors to tongue? thema” = red, “migrans” because it migrates which the tongue is exposed. This could be a There is no specific treatment, drug or or moves around), “benign migratory glossi- germ that usually lives in the mouth or a process that makes it disappear. tis” or “benign inflammatory glossitis”. foodstuff. People can be reassured not to be con- “Glossitis” means inflammation of the This reaction causes excessive shedding of cerned about it. -

First-Line Treatment of Oral Candidiasis in Adults
No. 628017 First-line Treatment of Oral Candidiasis in Adults Developed in collaboration with an advisory committee consisting of Québec clinicians and experts. Validated by the Comité d’excellence clinique en usage optimal du médicament, des protocoles médicaux nationaux et ordonnances of the Institut national d’excellence en santé et en services sociaux (INESSS). CLINICAL SITUATION OR TARGET POPULATION Person aged 18 years and older with one or several of the following clinical signs and symptoms: ► Sensation of burning, discomfort or general pain in the mouth or at the corners of the mouth, which worsens when eating food1 ► White patches that can be scraped away more or less easily; redness on the mucous membranes of the mouth. ► Cracked skin or slight bleeding at the corners of the mouth, which may extend to marionette lines. ► Total or partial loss of papillae on the surface of the tongue. CONTRAINDICATIONS TO THE APPLICATION OF THIS PROTOCOL ► Contraindication or history of allergic reaction to the recommended medication. ► Known case of refractory oral candidiasis. ► Oral candidiasis recurrence within one month of initial treatment. ► White patches that appear unilaterally on the tongue or cannot be scraped away. ► Bite or sore marks on the inside of the cheeks or on the tongue. ► Gum or submaxillary swelling. ► Surgery, injury, trauma, cut, burns in the mouth, or oral health problems (e.g. viral, bacterial or fungal infections) within the past two (2) weeks. ► Oral pain, localized or unilateral. ► Difficulty in swallowing, pain or burning sensation in the sternum or chest (suggesting esophageal candidiasis). ► Constant burning sensation that lessens when eating food (suggesting stomatopyrosis).