2020-2021 Follow up After ED for Dental Specifications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Lesions in Sjögren's Syndrome
Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Oral lesions in Sjögren’s syndrome patients Journal section: Oral Medicine and Pathology doi:10.4317/medoral.22286 Publication Types: Review http://dx.doi.org/doi:10.4317/medoral.22286 Oral lesions in Sjögren’s syndrome: A systematic review Julia Serrano 1, Rosa-María López-Pintor 1, José González-Serrano 1, Mónica Fernández-Castro 2, Elisabeth Casañas 1, Gonzalo Hernández 1 1 Department of Oral Medicine and Surgery, School of Dentistry, Complutense University, Madrid, Spain 2 Rheumatology Service, Hospital Infanta Sofía, Madrid, Spain Correspondence: Departamento de Especialidades Clínicas Odontológicas Facultad de Odontología Universidad Complutense de Madrid Plaza Ramón y Cajal s/n, 28040 Madrid. Spain [email protected] Serrano J, López-Pintor RM, González-Serrano J, Fernández-Castro M, Casañas E, Hernández G. Oral lesions in Sjögren’s syndrome: A system- atic review. Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e391-400. Received: 18/11/2017 http://www.medicinaoral.com/medoralfree01/v23i4/medoralv23i4p391.pdf Accepted: 09/05/2018 Article Number: 22291 http://www.medicinaoral.com/ © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: [email protected] Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Médico Español Abstract Background: Sjögren’s syndrome (SS) is an autoimmune disease related to two common symptoms: dry mouth and eyes. Although, xerostomia and hyposialia have been frequently reported in these patients, not many studies have evaluated other oral manifestations. -
Benign Migratory Glossitis: Case Report and Literature Review
Volume 1- Issue 5 : 2017 DOI: 10.26717/BJSTR.2017.01.000482 Sarfaraz Khan. Biomed J Sci & Tech Res ISSN: 2574-1241 Case Report Open Access Benign Migratory Glossitis: Case Report and Literature Review Sarfaraz Khan1*, Syed AsifHaider Shah2, Tanveer Ahmed Mujahid3 and Muhammad Ishaq4 1Consultant Oral and Maxillofacial Surgeon, Pak Field Hospital Darfur, Sudan 2MDC Gujranwala, Pakistan 3Consultant Dermatologist, Pak Field Hospital Darfur, Sudan 4Registrar Dermatologist, Pak Field Hospital Darfur, Sudan Received: October 25, 2017; Published: October 31, 2017 *Corresponding author: Sarfaraz Khan, Consultant Oral and Maxillofacial Surgeon, Pakistan Field Hospital Darfur, Sudan, Tel: ; Email: Abstract Benign migratory Glossitis (BMG) is a benign, usually asymptomatic mucosal lesion of dorsal surface of the tongue, characterized by depapillated erythematous patches separated by white irregular borders. Etiology of BMG is unknown. Risk factors include psoriasis, fissured tongue, diabetes mellitus, hypersensitivity and psychological factors. We report BMG in an Egyptian soldier of UN peace keeping force, with stressKeywords: as a possible Geographic etiological tongue; factor Benign and migratory provide literature Glossitis; reviewErythema of this migrans disorder. Introduction Benign migratory Glossitis (BMG) is a benign, immune- spicy/salty food and/or alcoholic drinks [4,5].The lesion typically usually characterized by asymptomatic erythematous patches changes its shape with time owing to the change in pattern of mediated, chronic inflammatory lesion of unknown etiology, depapillation.Similar lesions may also be seen in atrophic candidiasis, local chemical or mechanical trauma, drug induced reactions, psoriasis with whitish margins across the surface of the tongue. This condition is also known as geographic tongue, erythema migrans, Treatment of symptomatic BMG aims at provision of symptomatic Glossitis exfoliativa and wandering rash of the tongue. -

Case Report Treatment of Geographic Tongue
Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2015; 2(7):409-413 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Treatment of Geographic Tongue Superimposing Fissured Tongue: A literature review with case report Jalaleddin H Hamissi1, Mahsa EsFehani2, Zahra Hamissi3 1Associate Professor in periodontics and Dental Caries Prevention Research Center, Qazvin University Medical Sciences, Qazvin, Iran. 2Assistant Professor, Department of Oral Medicine & Diagnosis, college dentistry, Qazvin University Medical Sciences, Qazvin, Iran. 3Dental Student, College of Dentistry, Shahied Behesti University of Medical Sciences, Teheran, Iran *Corresponding author Dr Jalaleddin H Hamissi Email: [email protected] ; [email protected] Abstract: Tongue is a most sensitive part of the oral cavity. It is responsible for many functions in the mouth like swallowing, speech, mastication, speaking and breathing. Geographic tongue (Benign migratory glossitis, erythema migrans) is an asymptomatic inflammatory disorder of tongue with controversial etiology. This disease is characterized by erythematous areas showing raised greyish or white circinate lines or bands with irregular pattern on the dorsal surface of the tongue and depapillation. The objective in presenting the case report and literature review is to discuss the clinical presentation, associated causative factors and management strategies of geographic tongue. Keywords: Asymptomatic; Characteristics; Fissured tongue; Geographic tongue; Migratory INTRODUCTION in approximately three percent (3%) majority of female Geographic tongue is an asymptomatic population [9]. On other aspects of oral mucosa, such as inflammatory condition of the dorsum of tongue on commissure of lip, floor of mouth, cheek etc., which occasionally extending towards the lateral borders. -

Vertical Perspective Medical Assistance Program
Kansas Vertical Perspective Medical Assistance Program December 2006 Provider Bulletin Number 688 General Providers Emergent and Nonemergent Diagnosis Code List Attached is a list of diagnosis codes and whether the Kansas Medical Assistance Program (KMAP) considers the code to be emergent or nonemergent. Providers are responsible for validating whether a particular diagnosis code is covered by KMAP under the beneficiary’s benefit plan and that all program requirements are met. This list does not imply or guarantee payment for listed diagnosis codes. Information about the Kansas Medical Assistance Program as well as provider manuals and other publications are on the KMAP Web site at https://www.kmap-state-ks.us. If you have any questions, please contact the KMAP Customer Service Center at 1-800-933-6593 (in-state providers) or (785) 274-5990 between 7:30 a.m. and 5:30 p.m., Monday through Friday. EDS is the fiscal agent and administrator of the Kansas Medical Assistance Program for the Kansas Health Policy Authority. Page 1 of 347 Emergency Indicators as noted by KMAP: N – Never considered emergent S – Sometimes considered emergent (through supporting medical documentation) Y – Always considered emergent Diagnosis Emergency Diagnosis Code Description Code Indicator 0010 Cholera due to Vibrio Cholerae S 0011 Cholera due to Vibrio Cholerae El Tor S 0019 Unspecified Cholera S 019 Late Effects of Tuberculosis N 0020 Typhoid Fever S 0021 Paratyphoid Fever A S 0022 Paratyphoid Fever B S 0023 Paratyphoid Fever C S 024 Glanders Y 025 Melioidosis -

MICHIGAN BIRTH DEFECTS REGISTRY Cytogenetics Laboratory Reporting Instructions 2002
MICHIGAN BIRTH DEFECTS REGISTRY Cytogenetics Laboratory Reporting Instructions 2002 Michigan Department of Community Health Community Public Health Agency and Center for Health Statistics 3423 N. Martin Luther King Jr. Blvd. P. O. Box 30691 Lansing, Michigan 48909 Michigan Department of Community Health James K. Haveman, Jr., Director B-274a (March, 2002) Authority: P.A. 236 of 1988 BIRTH DEFECTS REGISTRY MICHIGAN DEPARTMENT OF COMMUNITY HEALTH BIRTH DEFECTS REGISTRY STAFF The Michigan Birth Defects Registry staff prepared this manual to provide the information needed to submit reports. The manual contains copies of the legislation mandating the Registry, the Rules for reporting birth defects, information about reportable and non reportable birth defects, and methods of reporting. Changes in the manual will be sent to each hospital contact to assist in complete and accurate reporting. We are interested in your comments about the manual and any suggestions about information you would like to receive. The Michigan Birth Defects Registry is located in the Office of the State Registrar and Division of Health Statistics. Registry staff can be reached at the following address: Michigan Birth Defects Registry 3423 N. Martin Luther King Jr. Blvd. P.O. Box 30691 Lansing MI 48909 Telephone number (517) 335-8678 FAX (517) 335-9513 FOR ASSISTANCE WITH SPECIFIC QUESTIONS PLEASE CONTACT Glenn E. Copeland (517) 335-8677 Cytogenetics Laboratory Reporting Instructions I. INTRODUCTION This manual provides detailed instructions on the proper reporting of diagnosed birth defects by cytogenetics laboratories. A report is required from cytogenetics laboratories whenever a reportable condition is diagnosed for patients under the age of two years. -

Oral Hard Tissue Lesions: a Radiographic Diagnostic Decision Tree
Scientific Foundation SPIROSKI, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2020 Aug 25; 8(F):180-196. https://doi.org/10.3889/oamjms.2020.4722 eISSN: 1857-9655 Category: F - Review Articles Section: Narrative Review Article Oral Hard Tissue Lesions: A Radiographic Diagnostic Decision Tree Hamed Mortazavi1*, Yaser Safi2, Somayeh Rahmani1, Kosar Rezaiefar3 1Department of Oral Medicine, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 2Department of Oral and Maxillofacial Radiology, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 3Department of Oral Medicine, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran Abstract Edited by: Filip Koneski BACKGROUND: Focusing on history taking and an analytical approach to patient’s radiographs, help to narrow the Citation: Mortazavi H , Safi Y, Rahmani S, Rezaiefar K. Oral Hard Tissue Lesions: A Radiographic Diagnostic differential diagnoses. Decision Tree. Open Access Maced J Med Sci. 2020 Aug 25; 8(F):180-196. AIM: This narrative review article aimed to introduce an updated radiographical diagnostic decision tree for oral hard https://doi.org/10.3889/oamjms.2020.4722 tissue lesions according to their radiographic features. Keywords: Radiolucent; Radiopaque; Maxilla; Mandible; Odontogenic; Nonodontogenic METHODS: General search engines and specialized databases including PubMed, PubMed Central, Scopus, *Correspondence: Hamed Mortazavi, Department of Oral Medicine, -

Periapical Radiopacities
2016 self-study course two course The Ohio State University College of Dentistry is a recognized provider for ADA CERP credit. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to the Commission for Continuing Education Provider Recognition at www.ada.org/cerp. The Ohio State University College of Dentistry is approved by the Ohio State Dental Board as a permanent sponsor of continuing dental education. This continuing education activity has been planned and implemented in accordance with the standards of the ADA Continuing Education Recognition Program (ADA CERP) through joint efforts between The Ohio State University College of Dentistry Office of Continuing Dental Education and the Sterilization Monitoring Service (SMS). ABOUT this COURSE… FREQUENTLY asked QUESTIONS… . READ the MATERIALS. Read and Q: Who can earn FREE CE credits? review the course materials. COMPLETE the TEST. Answer the A: EVERYONE - All dental professionals eight question test. A total of 6/8 in your office may earn free CE questions must be answered correctly credits. Each person must read the contact for credit. course materials and submit an online answer form independently. SUBMIT the ANSWER FORM ONLINE. You MUST submit your answers ONLINE at: Q: What if I did not receive a confirmation ID? us http://dentistry.osu.edu/sms-continuing-education A: Once you have fully completed your . -
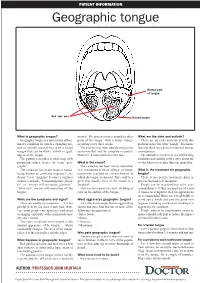
Geographic Tongue
PATIENT INFORMATION Geographic tongue Normal part of tongue Red ‘raw’ area Raised border What is geographic tongue? normal. The process moves around to other What are the risks and outlook? Geographic tongue is a non-serious inflam- parts of the tongue with a major change There are no risks associated with this matory condition in which a changing pat- occurring every three weeks. problem, hence the term “benign”. It is harm- tern of smooth red patches, with a raised The process may then subside and go into less and there have been no reported serious margin that can be white, yellow or grey, remission that may be complete or partial. consequences. appear on the tongue. However, it may return at a later time. The outlook is excellent. It is a self-limiting The pattern resembles a relief map with condition and usually settles after about six mountain ridges, hence the term “geo- What is the cause? weeks. However, it may flare up again later. graphic”. The cause has not been clearly identified. The condition has many medical names, It is considered to be an allergic or hyper- What is the treatment for geographic being known as erythema migrans (“ery- sensitivity reaction to certain factors to tongue? thema” = red, “migrans” because it migrates which the tongue is exposed. This could be a There is no specific treatment, drug or or moves around), “benign migratory glossi- germ that usually lives in the mouth or a process that makes it disappear. tis” or “benign inflammatory glossitis”. foodstuff. People can be reassured not to be con- “Glossitis” means inflammation of the This reaction causes excessive shedding of cerned about it. -

On the Tip of the Tongue
KNOWLEDGE TO PRACTICE DES CONNAISSANCES ÀLA PRATIQUE Diagnostic Challenge On the tip of the tongue . Rachel Orchard, MD*; Sheena Belisle, MD†; Rodrick Lim, MD†‡ Keywords: pediatric, rash, tongue, vesicle right-sided wheeze. Cardiovascular, abdominal, and neurological (including cranial nerve) examinations were unremarkable. CASE HISTORY What is the most likely diagnosis? A 14-year-old male presented to the pediatric emer- a) Drug eruption gency department (ED) with a chief complaint of b) Varicella zoster virus (VZV) changes to his tongue. He described a 3-day history of a c) Oral candidiasis gradually worsening sore, swollen tongue associated with a white plaque. This was accompanied by a 3-day d) Epstein-Barr virus history of a gradually worsening left-sided facial rash e) Oral lichen planus that had an intermittent mild tingling sensation. He also had a 1-week history of a productive cough with yellow mucus and generalized malaise. He had been seen at a walk-in clinic 2 days prior to presentation and was prescribed amoxicillin for presumed pneumo- nia, which he began the same day. He denied any history of fevers, facial weakness, neck stiffness, or eye symptoms. He was an otherwise well child, with up-to-date immunizations and a past medical history of chickenpox and recurrent furuncles as a younger child. On examination, he appeared well with the following vital signs: blood pressure 122/64 mm Hg, heart rate 73 beats per minute, respiratory rate 18 breaths per minute, temperature 36.8°C, and oxygen saturation of 99% on room air. Examination of his tongue revealed a symmetric white plaque along with ulcerative lesions on the left tongue and buccal mucosa (Figure 1). -

Dental ICD-10 Information
317:30-5-705. Billing Billing for dental services may be submitted on the currently-approved version of the American Dental Association (ADA) claim form. Diagnosis codes are requested to be listed in box 34 of ADA form 2012. To assist with your learning, the following codes are listed from International Classification of Disease, 10th revision, Clinical Modification (ICD-10-CM), Chapter 11: Diseases of the Digestive System (K00-K95). Most dental disorders are included in section K00- K14 - Diseases of oral cavity and salivary glands. ICD-10-CM 2016 K00 Disorders of tooth development and eruption K00.0 Anodontia K00.1 Supernumerary teeth K00.2 Abnormalities of size and form of teeth K00.3 Mottled teeth K00.4 Disturbances in tooth formation K00.5 Hereditary disturbances in tooth structure, not elsewhere classified K00.6 Disturbances in tooth eruption K00.7 Teething syndrome K00.8 Other disorders of tooth development K01 Embedded and impacted teeth K01.0 Embedded teeth K01.1 Impacted teeth K02 Dental caries K02.3 Arrested dental caries K02.5 Dental caries on pit and fissure surface o K02.51 limited to enamel o K02.52 penetrating into dentin o K02.53 penetrating into pulp K02.6 Dental caries on smooth surface o K02.61 limited to enamel o K02.62 penetrating into dentin o K02.63 penetrating into pulp K02.7 Dental root caries K03 other diseases of hard tissues of teeth K03.0 Excessive attrition of teeth K03.1 Abrasion of teeth K03.2 Erosion of teeth Last updated 7/2016 1 K03.3 Pathological resorption of teeth K03.4 Hypercementosis -

Oral Manifestations of a Possible New Periodic Fever Syndrome Soraya Beiraghi, DDS, MSD, MS, MSD1 • Sandra L
PEDIATRIC DENTISTRY V 29 / NO 4 JUL / AUG 07 Case Report Oral Manifestations of a Possible New Periodic Fever Syndrome Soraya Beiraghi, DDS, MSD, MS, MSD1 • Sandra L. Myers, DMD2 • Warren E. Regelmann, MD3 • Scott Baker, MD, MS4 Abstract: Periodic fever syndrome is composed of a group of disorders that present with recurrent predictable episodes of fever, which may be accompanied by: (1) lymphadenopathy; (2) malaise; (3) gastrointestinal disturbances; (4) arthralgia; (5) stomatitis; and (6) skin lesions. These signs and symptoms occur in distinct intervals every 4 to 6 weeks and resolve without any residual effect, and the patient remains healthy between attacks. The evaluation must exclude: (1) infections; (2) neoplasms; and (3) autoimmune conditions. The purpose of this paper is to report the case of a 4½- year-old white female who presented with a history of periodic fevers accompanied by: (1) joint pain; (2) skin lesions; (3) rhinitis; (4) vomiting; (5) diarrhea; and (6) an unusual asymptomatic, marked, fi ery red glossitis with features evolving to resemble geographic tongue and then resolving completely between episodes. This may represent the fi rst known reported case in the literature of a periodic fever syndrome presenting with such unusual recurring oral fi ndings. (Pediatr Dent 2007;29:323-6) KEYWORDS: PERIODIC FEVER, MOUTH LESIONS, GEOGRAPHIC TONGUE, STOMATITIS The diagnosis of periodic fever syndrome is often challeng- low, mildly painful ulcerations, which vary in number, and ing in children. Periodic fever syndrome is composed -

Chin and Malar Augmentation
CHIN AND MALAR AUGMENTATION SOROUSH ZAGHI, MD INTRODUCTION EVALUATION OF CHIN PROJECTION Chin projection should approach a line perpendicular to the Frankfurt horizontal at vermilion border of lower lip. ZERO MERIDIAN OF GONZALES-ULLOA A line perpendicular to the Frankfort horizontal line is projected through the nasion. Legan’s angle Contained by lines from the glabella to the subnasale and the subnasale to the soft-tissue pogonion. This should be 12 ± 4 degrees for appropriate chin projection. MERRIFIELD Z ANGLE Contained by the Frankfort horizontal line and a line connecting the soft-tissue pogonion to the most anterior part of the lip. The Z angle should be 80 ± 5 degrees. PRE-OPERATIVE CONSIDERATIONS • Skin texture • Anatomic proportions • Prior facial trauma • Emotional stability • Aging face: Soft tissue ptosis, jowls, Marionette lines • Occlusal relationship: Microgenia, Micrognathia, Retrognathia. PATIENT WITH JOWLS • 35 F – Before and 4 months after chin implant with liposuction from jowls and submental area. PATIENT WITH RETROGNATHIA • Patient with retrognathia, voluntary protrusion of jaw (better candidate for mandibular advancement) • Patient with retrognathia and chin implant (deepened labiomental fold). Lower lip analysis- Labiomental fold • Position of the labiomental fold determines the chin pad percentage of the lower facial height. • High labiomental fold Poor candidate. Augmentation will enlarge the entire lower face. • Low labiomental fold Good candidate. Augmentation will accentuate the chin only. LOW LABIOMENTAL FOLD • Patient with low labiomental fold • Before and after chin augmentation. CHIN PAD THICKNESS • Soft tissue thickness: normal= 8 to 11 mm. • Cephalogram demonstrating a very thick chin pad. • Avoid setting back jaws with thick pads; leads to bony irregularities, soft tissue pad ptosis and an unsupported chin pad.