Tricks and Techniques to Maximize Success with Nerve Transfers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
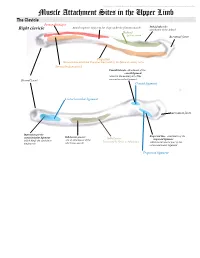
Muscle Attachment Sites in the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Muscle Attachment Sites in the Upper Limb The Clavicle Pectoralis major Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: Right clavicle attachment of the deltoid Deltoid Axillary nerve Acromial facet Trapezius Sternocleidomastoid and Trapezius innervated by the Spinal Accessory nerve Sternocleidomastoid Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Conoid ligament Costoclavicular ligament Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Subclavian groove: Subclavius trapezoid ligament which binds the clavicle to site of attachment of the Innervated by Nerve to Subclavius which is the lateral part of the the first rib subclavius muscle coracoclavicular ligament Trapezoid ligament This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. The Scapula Trapezius Right scapula: posterior Levator scapulae Supraspinatus Deltoid Deltoid and Teres Minor are innervated by the Axillary nerve Rhomboid minor Levator Scapulae, Rhomboid minor and Rhomboid Major are innervated by the Dorsal Scapular Nerve Supraspinatus and Infraspinatus innervated by the Suprascapular nerve Infraspinatus Long head of triceps Rhomboid major Teres Minor Teres Major Teres Major -

Examination of the Shoulder Bruce S
Examination of the Shoulder Bruce S. Wolock, MD Towson Orthopaedic Associates 3 Joints, 1 Articulation 1. Sternoclavicular 2. Acromioclavicular 3. Glenohumeral 4. Scapulothoracic AC Separation Bony Landmarks 1. Suprasternal notch 2. Sternoclavicular joint 3. Coracoid 4. Acromioclavicular joint 5. Acromion 6. Greater tuberosity of the humerus 7. Bicipital groove 8. Scapular spine 9. Scapular borders-vertebral and lateral Sternoclavicular Dislocation Soft Tissues 1. Rotator Cuff 2. Subacromial bursa 3. Axilla 4. Muscles: a. Sternocleidomastoid b. Pectoralis major c. Biceps d. Deltoid Congenital Absence of Pectoralis Major Pectoralis Major Rupture Soft Tissues (con’t) e. Trapezius f. Rhomboid major and minor g. Latissimus dorsi h. Serratus anterior Range of Motion: Active and Passive 1. Abduction - 90 degrees 2. Adduction - 45 degrees 3. Extension - 45 degrees 4. Flexion - 180 degrees 5. Internal rotation – 90 degrees 6. External rotation – 45 degrees Muscle Testing 1. Flexion a. Primary - Anterior deltoid (axillary nerve, C5) - Coracobrachialis (musculocutaneous nerve, C5/6 b. Secondary - Pectoralis major - Biceps Biceps Rupture- Longhead Muscle Testing 2. Extension a. Primary - Latissimus dorsi (thoracodorsal nerve, C6/8) - Teres major (lower subscapular nerve, C5/6) - Posterior deltoid (axillary nerve, C5/6) b. Secondary - Teres minor - Triceps Abduction Primary a. Middle deltoid (axillary nerve, C5/6) b. Supraspinatus (suprascapular nerve, C5/6) Secondary a. Anterior and posterior deltoid b. Serratus anterior Deltoid Ruputure Axillary Nerve Palsy Adduction Primary a. Pectoralis major (medial and lateral pectoral nerves, C5-T1 b. Latissimus dorsi (thoracodorsal nerve, C6/8) Secondary a. Teres major b. Anterior deltoid External Rotation Primary a. Infraspinatus (suprascapular nerve, C5/6) b. Teres minor (axillary nerve, C5) Secondary a. -

Brachial Plexus Posterior Cord Variability: a Case Report and Review
CASE REPORT Brachial plexus posterior cord variability: a case report and review Edward O, Arachchi A, Christopher B Edward O, Arachchi A, Christopher B. Brachial plexus posterior cord anatomical variability. This case report details the anatomical variants discovered variability: a case report and review. Int J Anat Var. 2017;10(3):49-50. in the posterior cord of the brachial plexus in a routine cadaveric dissection at the University of Melbourne, Australia. Similar findings in the literature are reviewed ABSTRACT and the clinical significance of these findings is discussed. The formation and distribution of the brachial plexus is a source of great Key Words: Brachial plexus; Posterior cord; Axillary nerve; Anatomical variation INTRODUCTION he brachial plexus is the neural network that supplies motor and sensory Tinnervation to the upper limb. It is typically composed of anterior rami from C5 to T1 spinal segments, which subsequently unite to form superior, middle and inferior trunks. These trunks divide and reunite to form cords 1 surrounding the axillary artery, which terminate in branches of the plexus. The posterior cord is classically described as a union of the posterior divisions from the superior, middle and inferior trunks of the brachial plexus, with fibres from all five spinal segments. The upper subscapular, thoracodorsal and lower subscapular nerves propagate from the cord prior to the axillary and radial nerves forming terminal branches. Variability in the brachial plexus is frequently reported in the literature. It is C5 nerve root Suprascapular nerve important for clinicians to be aware of possible variations when considering Posterior division of C5-C6 injuries or disease of the upper limb. -

Supply Distribution of the Brachial Plexus
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. SUPPLY DISTRIBUTION OF THE BRACHIAL PLEXUS Lateral pectoral nerve Pectoralis major Lateral cord Anterior compartment of the arm: MUSCULOCUTANEOUS NERVE Biceps, coracobrachialis, brachialis Skin over the lateral forearm, once it becomes cutaneous in the cubital fossa Anterior compartment of the forearm: EXCEPT for the ulnar part of flexor digitorum profundis MEDIAN NERVE Thenar muscles: EXCEPT adductor pollicis and the deep part of flexor pollicis brevis First and second lumbricals Skin on the medial surface of arm up to the elbow MedialLateral cutaneous cord: nerve of arm lateral pectoral nerve Medial cord Skin on the medial surface of forearm up to the elbow Medial cutaneous MUSCULOCUTANEOUS nerve of forearm NERVE lateral root of MEDIAN NERVE Medial pectoral nerve Pectoralis minor and sternocostal part of pectoralis major o Medial cord forms ULNAR NERVE Intrinsic muscles of the hand, EXCEPT 1st and 2nd lumbricals and three of the thenar muscles Flexor carpi ulnaris Ulnar half of the flexor digitorum profundis to the pinky and ring fingers Upper subscapular nerve Superior half of subscapularis medial root of MEDIAN NERVE Lower subscapular nerve Inferior half of subscapularis AND teres major medial pectoral nerve medial cutaneous nerveGlenohumeral of arm joint Teres minor medial cutaneous nerve of forearm Posterior cord AXILLARY NERVE Deltoid ULNAR NERVE Skin over the deltoid RADIAL NERVE ALL MUSCLES IN THE POSTERIOR COMPARTMENT OF THE ARM AND FOREARM Ski over posterior and inferolateral forearm Some of the dorsum of the hand o o Thoracodorsal nerve Latissimus Dorsi o o Posterior cord forms: Long Thoracic nerve Serratus anterior Dorsal scapular nerve Rhomboids; Supraclavicular branches levator scapulae Subclavius and Nerve to subclavius sternoclavicular joint Suprascapular nerve Supraspinatus Infraspinatus Glenohumeral joint. -
Pectoral Region and Axilla Doctors Notes Notes/Extra Explanation Editing File Objectives
Color Code Important Pectoral Region and Axilla Doctors Notes Notes/Extra explanation Editing File Objectives By the end of the lecture the students should be able to : Identify and describe the muscles of the pectoral region. I. Pectoralis major. II. Pectoralis minor. III. Subclavius. IV. Serratus anterior. Describe and demonstrate the boundaries and contents of the axilla. Describe the formation of the brachial plexus and its branches. The movements of the upper limb Note: differentiate between the different regions Flexion & extension of Flexion & extension of Flexion & extension of wrist = hand elbow = forearm shoulder = arm = humerus I. Pectoralis Major Origin 2 heads Clavicular head: From Medial ½ of the front of the clavicle. Sternocostal head: From; Sternum. Upper 6 costal cartilages. Aponeurosis of the external oblique muscle. Insertion Lateral lip of bicipital groove (humerus)* Costal cartilage (hyaline Nerve Supply Medial & lateral pectoral nerves. cartilage that connects the ribs to the sternum) Action Adduction and medial rotation of the arm. Recall what we took in foundation: Only the clavicular head helps in flexion of arm Muscles are attached to bones / (shoulder). ligaments / cartilage by 1) tendons * 3 muscles are attached at the bicipital groove: 2) aponeurosis Latissimus dorsi, pectoral major, teres major 3) raphe Extra Extra picture for understanding II. Pectoralis Minor Origin From 3rd ,4th, & 5th ribs close to their costal cartilages. Insertion Coracoid process (scapula)* 3 Nerve Supply Medial pectoral nerve. 4 Action 1. Depression of the shoulder. 5 2. Draw the ribs upward and outwards during deep inspiration. *Don’t confuse the coracoid process on the scapula with the coronoid process on the ulna Extra III. -

A Comprehensive Review of Anatomy and Regional Anesthesia Techniques of Clavicle Surgeries
vv ISSN: 2641-3116 DOI: https://dx.doi.org/10.17352/ojor CLINICAL GROUP Received: 31 March, 2021 Research Article Accepted: 07 April, 2021 Published: 10 April, 2021 *Corresponding author: Dr. Kartik Sonawane, Uncovering secrets of the Junior Consultant, Department of Anesthesiol- ogy, Ganga Medical Centre & Hospitals, Pvt. Ltd. Coimbatore, Tamil Nadu, India, E-mail: beauty bone: A comprehensive Keywords: Clavicle fractures; Floating shoulder sur- gery; Clavicle surgery; Clavicle anesthesia; Procedure review of anatomy and specific anesthesia; Clavicular block regional anesthesia techniques https://www.peertechzpublications.com of clavicle surgeries Kartik Sonawane1*, Hrudini Dixit2, J.Balavenkatasubramanian3 and Palanichamy Gurumoorthi4 1Junior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 2Fellow in Regional Anesthesia, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 3Senior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 4Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India Abstract The clavicle is the most frequently fractured bone in humans. General anesthesia with or without Regional Anesthesia (RA) is most frequently used for clavicle surgeries due to its complex innervation. Many RA techniques, alone or in combination, have been used for clavicle surgeries. These include interscalene block, cervical plexus (superficial and deep) blocks, SCUT (supraclavicular nerve + selective upper trunk) block, and pectoral nerve blocks (PEC I and PEC II). The clavipectoral fascial plane block is also a safe and simple option and replaces most other RA techniques due to its lack of side effects like phrenic nerve palsy or motor block of the upper limb. -

Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies
Electrodiagnosis of Brachial Plexopathies and Proximal Upper Extremity Neuropathies Zachary Simmons, MD* KEYWORDS Brachial plexus Brachial plexopathy Axillary nerve Musculocutaneous nerve Suprascapular nerve Nerve conduction studies Electromyography KEY POINTS The brachial plexus provides all motor and sensory innervation of the upper extremity. The plexus is usually derived from the C5 through T1 anterior primary rami, which divide in various ways to form the upper, middle, and lower trunks; the lateral, posterior, and medial cords; and multiple terminal branches. Traction is the most common cause of brachial plexopathy, although compression, lacer- ations, ischemia, neoplasms, radiation, thoracic outlet syndrome, and neuralgic amyotro- phy may all produce brachial plexus lesions. Upper extremity mononeuropathies affecting the musculocutaneous, axillary, and supra- scapular motor nerves and the medial and lateral antebrachial cutaneous sensory nerves often occur in the context of more widespread brachial plexus damage, often from trauma or neuralgic amyotrophy but may occur in isolation. Extensive electrodiagnostic testing often is needed to properly localize lesions of the brachial plexus, frequently requiring testing of sensory nerves, which are not commonly used in the assessment of other types of lesions. INTRODUCTION Few anatomic structures are as daunting to medical students, residents, and prac- ticing physicians as the brachial plexus. Yet, detailed understanding of brachial plexus anatomy is central to electrodiagnosis because of the plexus’ role in supplying all motor and sensory innervation of the upper extremity and shoulder girdle. There also are several proximal upper extremity nerves, derived from the brachial plexus, Conflicts of Interest: None. Neuromuscular Program and ALS Center, Penn State Hershey Medical Center, Penn State College of Medicine, PA, USA * Department of Neurology, Penn State Hershey Medical Center, EC 037 30 Hope Drive, PO Box 859, Hershey, PA 17033. -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

Langer's Axillary Arch (Axillopectoral Muscle): a Variation of Latissimus
eISSN 1308-4038 International Journal of Anatomical Variations (2010) 3: 91–92 Case Report Langer’s axillary arch (axillopectoral muscle): a variation of latissimus dorsi muscle Published online June 30th, 2010 © http://www.ijav.org Sinan BAKIRCI ABSTRACT Ilker Mustafa KAFA Langer’s axillary arch (axillopectoral muscle) is a variant muscular structure of the axilla which was described Murat UYSAL under various names as Langer’s muscle, axillary arch or muscular axillary arch by different authors. During Erdogan SENDEMIR routine dissections, we found a muscular slip on the right axillary fossa that originated from latissimus dorsi muscle and attached to the deep surface of the tendon of pectoralis major muscle, and described it as Langer’s axillary arch. Arterial, venous and nervous structures passed under this muscular slip which constitutes an arch in the axillary fossa. Although axillary arch is not very rare, it is generally neglected and not explored or described well. It has immense clinical and morphologic importance for surgical operations performed on axillary region; thus, surgeons should well be aware of its possible existence. © IJAV. 2010; 3: 91–92. Department of Anatomy, Faculty of Medicine, Uludag University, Bursa, TURKEY. Ilker Mustafa Kafa, MD Department of Anatomy Uludag University Faculty of Medicine Gorukle, 16059, Bursa, TURKEY. +90 (224) 295 23 16 [email protected] Received November 20th, 2009; accepted June 21st, 2010 Key words [axillary arch] [Langer’s muscle] [latissimus dorsi muscle] [axillopectoral muscle] [axillary fossa] Introduction os ilium. The axillary arch is a variant muscular slip of Best-known variant structure of the axillary components this muscle and is about 7 to 10 cm in length, splits from of men is a muscular or fibro-muscular slip extending the upper edge of the latissimus dorsi and crosses the from the latissimus dorsi muscle to the tendons, muscles or axilla in front of the axillary vessels and nerves [4]. -

Winged Scapula
r e v b r a s o r t o p . 2 0 1 5;5 0(5):573–577 www.rbo.org.br Artigo Original Síndrome do aprisionamento fascial do nervo ଝ torácico longo: escápula alada a,b c,∗ b,d Jefferson Braga Silva , Samanta Gerhardt e Ivan Pacheco a Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brasil b Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul (PUC-RS), Porto Alegre, RS, Brasil c Faculdade de Medicina, Pontifícia Universidade Católica do Rio Grande do Sul (PUC-RS), Porto Alegre, RS, Brasil d Instituto de Medicina do Esporte, Hospital Mãe de Deus, Porto Alegre, RS, Brasil informações sobre o artigo r e s u m o Histórico do artigo: Objetivo: Analisar os resultados de cirurgia de intervenc¸ão precoce em pacientes com sín- Recebido em 1 de julho de 2014 drome do aprisionamento fascial do nervo torácico longo e consequente escápula alada. Aceito em 16 de setembro de 2014 Métodos: Acompanhamos seis pacientes com uma síndrome de aprisionamento sem On-line em 24 de dezembro de 2014 restric¸ões específicas de estiramento ao nervo. Resultados: Pacientes tiveram melhoria em seus sintomas seis a 20 meses após o proce- Palavras-chave: dimento. Sintomas motores melhoraram completamente sem qualquer dor persistente. A Escápula deformidade medial da escápula alada melhorou em todos os casos sem distúrbios estéticos Tórax residuais. Síndromes de compressão nervosa Conclusão: A abordagem de liberac¸ão cirúrgica precoce parece ser um melhor preditor na recuperac¸ão de paralisia não traumática do músculo serrátil anterior. -

Anatomical Study of Pectoral Nerves and Its Implications in Surgery a Natomy S Ection
DOI: 10.7860/JCDR/2014/8631.4545 Original Article ection Anatomical Study of Pectoral Nerves and S its Implications in Surgery natomy A PRAKASH KG1, SANIYA K2 ABSTRACT ramify within the muscle supplying it, finally runs along the Introduction: This anatomical study of the pectoral nerves lateral aspect (lower border) of the pectoralis minor muscle and their innervation is to provide detail informations on the to supply the lower portion or distal segment of the pectoralis pectoral nerves and their variations in their course, to guide major muscle. Similarly, the lateral pectoral nerve runs along the cosmetic and plastic surgeons for their easy intra operative the upper border (medial aspect) of the pectoralis minor muscle localization and to improve the understanding of the pectoral (98%) and then runs under surface of the pectoralis major muscle innervation, which is very much required during breast muscle along with the pectoral branch of thoracoacromial reconstruction after modified radical mastectomy (MRM) in artery, supplying the upper portion or most of the proximal 2/3rd breast cancer; axillary dissection; removal of the pectoralis of the pectoralis major muscle. Therefore, when the pectoralis minor muscle, and in harvesting the pectoralis major for minor muscle is removed in a modified radical mastectomy or myocutaneous head and neck island flap surgeries. during dissection between the two muscles, there is partial denervation of the pectoralis major muscle with partial atrophy Materials and Methods: A total of 50 pectoral region specimens and decrease in muscle mass. If the lateral pectoral nerve also (both right and left sided) from 25 embalmed adult human injured along with the medial pectoral nerve, it can result in total cadavers (20 female & 05 male) were studied by dissection denervation of the pectoralis major muscle with severe atrophy method. -

Abrant Origion and Distribution of Pectoral Nerves with Prominent Ansa Pectoralis and Absent Lateral Pectoral Nerve Chernet Bahru Tessema*
Case Report Abrant origion and distribution of pectoral nerves with prominent ansa pectoralis and absent lateral pectoral nerve Chernet Bahru Tessema* Tessema CB. Abrant origion and distribution of pectoral nerves with that distributed to the two pectoralis muscles. Two of the ansa pectoralis prominent ansa pectoralis and absent lateral pectoral nerve. Int J Anat branchesentered pectoralis major, one ended on pectoralis minor and one Var. 2020;13(2):1-3. entered both muscles. No lateral pectoral nerve from the lateral cord was observed. ABSTRACT Though the presence of multiple branches like in this case would make During the dissection of the left axilla of an 80-year-old male cadaver three approach to the pectoral region difficult without damage to these nerves, it anterior and one medial pectoral nerves were incidentally detected. All the could safeguard the normal muscle function in situation of isolated nerve three anterior pectoral nerve arose from the anterior division of the middle injuries. trunk of the brachial plexus. The upper two anterior pectoral nerves entered pectoralis major while the most inferior joined the medial pectoral nerve to Key Words: Brachial plexus; Anterior pectoral nerves; Medial pectoral nerve; Ansa form a prominent ansa pectoralis. The ansa pectorals then gave four branches pectoralis. INTRODUCTION entered the clavicular part of pectoralis major and the middle terminated in the most superior fibers of the sternocostal part of pectoralis major closer to he pectoralis muscles are innervated by the medial and lateral pectoral its clavicular part (Figures 1-3). The inferior anterior pectoral nerve joined Tnerves, which are branches of the respective cords of the brachial the medial pectoral nerve to form a loop, the ansa pectoralis (Figures 1 and plexus.