What's Inside
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chairman of the Opening Session
The Universe had (probably) an origin: on singularity theorems & quantum fluctuations Emilio Elizalde ICE/CSIC & IEEC Campus UAB, Barcelona Cosmology and the Quantum Vacuum III, Benasque, Sep 4-10, 2016 Some facts (a few rather surprising...) • Adam Riess, NP 2011, at Starmus (Tenerife), about Hubble: • “Hubble obtained the distances and redshifts of distant nebulae…” • “Hubble discovered that the Universe was expanding…” • No mention to Vesto Slipher, an extraordinary astronomer • Brian Schmidt, NP 2011, at Starmus (Tenerife) & Lisa Randall, Harvard U, in Barcelona, about Einstein: SHOES- • “Einstein was the first to think about the possibility of a ‘dark energy’…” Supernovae • No mention to Fritz Zwicky, another extraordinary astronomer • Fritz Zwicky discovered dark matter in the early 1930s while studying how galaxies move within the Coma Cluster • He was also the first to postulate and use nebulae as gravitational lenses (1937) • How easily* brilliant astronomers get dismissed • How easily* scientific myths arise *in few decades How did the “Big Bang” get its name ? http://www.bbc.co.uk/science/space/universe/scientists/fred_hoyle • Sir Fred Hoyle (1915–2001) English astronomer noted primarily for the theory of stellar nucleosynthesis (1946,54 groundbreaking papers) • Work on Britain's radar project with Hermann Bondi and Thomas Gold • William Fowler NP’83: “The concept of nucleosynthesis in stars was first established by Hoyle in 1946” • He found the idea universe had a beginning to be pseudoscience, also arguments for a creator, “…for it's an irrational process, and can't be described in scientific terms”; “…belief in the first page of Genesis” • Hoyle-Gold-Bondi 1948 steady state theory, “creation or C-field” • BBC radio's Third Programme broadcast on 28 Mar 1949: “… for this to happen you would need such a Big Bang!” Thus: Big Bang = Impossible blow!! But now: Big Bang ≈ Inflation ! • Same underlying physics as in steady state theory, “creation or C-field” • Richard C. -

What Is the Universe Made Of? How Old Is the Universe?
What is the Universe made of? How old is it? Charles H. Lineweaver University of New South Wales ABSTRACT For the past 15 years most astronomers have assumed that 95% of the Universe was in some mysterious form of cold dark matter. They also assumed that the cosmo- logical constant, ΩΛ, was Einstein’s biggest blunder and could be ignored. However, recent measurements of the cosmic microwave background combined with other cos- mological observations strongly suggest that 75% of the Universe is made of cosmo- logical constant (vacuum energy), while only 20% is made of non-baryonic cold dark matter. Normal baryonic matter, the stuff most physicists study, makes up about 5% of the Universe. If these results are correct, an unknown 75% of the Universe has been identified. Estimates of the age of the Universe depend upon what it is made of. Thus, our new inventory gives us a new age for the Universe: 13.4 ± 1.6 Gyr. “The history of cosmology shows us that in every age devout people believe that they have at last discovered the true nature of the Universe.” (E. Harrison in Cosmology: The Science of the Universe 1981) 1 Progress A few decades ago cosmology was laughed at for being the only science with no data. Cosmology was theory-rich but data-poor. It attracted armchair enthusiasts spouting speculations without data to test them. It was the only science where the errors could be kept in the exponents – where you could set the speed of light c =1, not for dimensionless convenience, but because the observations were so poor that it didn’t matter. -

Unit 1 Module A: Jane Goodall Biography
Grade 4 Informative Writing Prompt District Common Writing Assessment Unit 1 Module A: Jane Goodall Biography Directions should be read aloud and clarified by the teacher. Directions Today, you are going to get ready to write a biography about Jane Goodall and how she made a difference in the world as a scientist. You are going to use what you have learned to write a biography which addresses the question: How did Jane Goodall make a difference in the world as a scientist? Day 1 Get ready to write. • Watch the video, Jane Goodall Mini Biography. (Link attached below) • Discuss how Jane Goodall made a difference in the world as a scientist. • Listen to and read the article: "Biographies for Kids: Jane Goodall". (Attached) You may want to take notes for your biography as you read. • Why was Jane Goodall an important scientist? Turn and talk to a partner about what you read in the text and heard in the video. Teacher notes: Take this time to use whatever note taking and partnering strategies you have been using in class. The video has a commercial at the start so please cue before viewing. Days 2-3 Write! • Watch the video, Jane Goodall Mini Biography. (Link attached below) • Listen to and read the article: "Biographies for Kids: Jane Goodall" (Attached) • When you have finished, write a biography detailing Jane Goodall’s life and how she made a difference in the world as a scientist. Remember, a good biography / informative essay: • Has an introduction • Clearly introduces the subject • Develops a main idea about the subject with facts and concrete details • Groups ideas in paragraphs • Uses precise language and vocabulary • Uses linking words to connect ideas • Has correct spelling, capitalization, and punctuation • Uses quotes to cite sources • Has an effective concluding statement Resources: Article: "Biographies for Kids Jane Goodall" (Attached) Video: Jane Goodall Mini Biography. -

Congressional Record—Senate S10810
S10810 CONGRESSIONAL RECORD — SENATE December 20, 2010 advocate for the Peace Corps program food safety dangers occur and are oc- Senior citizens deserve to have hous- and for volunteerism in general. In curring. The use of indirect food addi- ing that will help them maintain their that regard, he and I have much in tives and processing aids have not been independence. It is my hope that with common. As a young man, I served a determined to be the source of food the passage of S. 118, many more Amer- full-time mission for the Church of borne illness outbreaks and I believe it icans have a place to call home during Jesus Christ of Latter-day Saints. I too is important that the FDA continue to their golden years. learned much about the benefits of focus its scarce resources on the key f selfless, volunteer service while serving elements that this legislation hopes to TRIBUTE TO DR. JANE GOODALL as a missionary and those 2 years were address in the Food Safety area. instrumental in my understanding of f Mr. UDALL of New Mexico. Mr. the world and instilled me with a de- President, in July I introduced S. Res. ELDERLY HOUSING sire to serve and help others. The Serve 581, a resolution honoring the edu- America Act was meant to embody Mr. KOHL. Mr. President, I rise cational and scientific significance of these ideals and provide similar oppor- today to praise the passage of S. 118, Dr. Jane Goodall on the 50th anniver- tunities for others. It could have very the section 202 Supportive Housing for sary of the beginning of her work in easily been a purely Democratic en- the Elderly Act. -
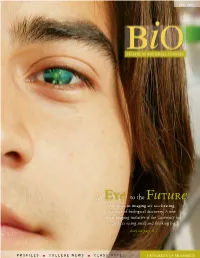
An Eye to the Future Advances in Imaging Are Accelerating the Pace of Biological Discovery
fall 2007 An Eye to the Future Advances in imaging are accelerating the pace of biological discovery. A new cellular imaging initiative at the University has researchers seeing small and thinking big. story on page 8 p r o f i l e s college News c l a s s N o t e s from the dean Where curiosity- and solution- driven science meet ome scientists are driven by a curiosity to under- As a curiosity-driven college, it’s CBS’ job to keep S stand how life works—from molecules to eco- adding to the foundation of knowledge that supports systems—and to add to the world’s collective body of translational and solution-driven science in other col- knowledge. Others are searching for a puzzle piece leges. As such, we are the stewards of the foundational that may yield a better way to treat cancer, produce disciplines in the biological sciences: biochemistry, food or create renewable forms of energy. molecular biology, genetics, cell biology and develop- ment, ecology, plant biology, etc. Both are essential, and there is plenty of overlap Robert Elde, Dean between the two. Curiosity-driven research often turns In order to keep fueling translational and solution- up a bit of information that has immediate applications driven research, we need to infuse foundational disci- in medicine, agriculture or engineering. By the same plines with new technologies and other opportunities token, solution-driven research can add to knowledge. as science evolves. And some scientists travel between these two worlds. Fall 07 Vol. 5 No. 3 Cellular imaging, the subject of our cover story, is one As a whole, College of Biological Sciences faculty of those opportunities. -

Inspiring Spaces
FALL 2011 Inspiring Spaces Explorations Grand Challenges and Inspiration: Lighting the Fire in the Next Generation 2011 Bradford Washburn Award In Gratitude Raytheon: Our Newest Premier Partner Fiscal Year 2011 Annual Report 418496 Booklet.CS4.indd 3 11/22/11 5:49 AM FIELD NOTES contents Special Nights with Special Friends… Nothing gets the Museum’s community of friends and supporters energized like a special event, and we were fortunate to have more than a few fantastic evening events this fall. A Day in Pompeii (see IN BRIEF) gave us an opportunity to gather and experience the art and archaeological artifacts of the ancient world, and two of our annual award programs offered us a chance to celebrate those members of the Museum community who inspire us most. We presented the 47th Bradford Washburn Award to Jean-Michel Cousteau on September 7 (see pages 22 – 23 for story and photos). In addition to recognizing Cousteau’s commitment to ocean exploration and environmental protection, the Washburn Award dinner provides us the occasion every year to remember Brad Washburn, the visionary founding director of the Museum of Science. On November 3 we honored members of the Colby Society, donors whose cumulative giving to the Museum is in excess of $100,000 (page 39). At the Colby dinner we paid special tribute to Sophia and Bernie Gordon, whose remarkable philanthropy is felt in the Museum every day at the Gordon Current Science & Technology Center, which was established in 2006 with their lead gift. The Gordons were presented with the Colonel Francis T. Colby Award and their names will join our inaugural Colby honorees, trustee emeriti Joan Suit and Brit d’Arbeloff, on the plaque beside the elephant doors at the entrance to the Museum’s Colby Room (see pages 18 – 19 for story and photos). -

Jane Goodall: a Timeline 3
Discussion Guide Table of Contents The Life of Jane Goodall: A Timeline 3 Growing Up: Jane Goodall’s Mission Starts Early 5 Louis Leakey and the ‘Trimates’ 7 Getting Started at Gombe 9 The Gombe Community 10 A Family of Her Own 12 A Lifelong Mission 14 Women in the Biological Sciences Today 17 Jane Goodall, in Her Own Words 18 Additional Resources for Further Study 19 © 2017 NGC Network US, LLC and NGC Network International, LLC. All rights reserved. 2 Journeys in Film : JANE The Life of Jane Goodall: A Timeline April 3, 1934 Valerie Jane Morris-Goodall is born in London, England. 1952 Jane graduates from secondary school, attends secretarial school, and gets a job at Oxford University. 1957 At the invitation of a school friend, Jane sails to Kenya, meets Dr. Louis Leakey, and takes a job as his secretary. 1960 Jane begins her observations of the chimpanzees at what was then Gombe Stream Game Reserve, taking careful notes. Her mother is her companion from July to November. 1961 The chimpanzee Jane has named David Greybeard accepts her, leading to her acceptance by the other chimpanzees. 1962 Jane goes to Cambridge University to pursue a doctorate, despite not having any undergraduate college degree. After the first term, she returns to Africa to continue her study of the chimpanzees. She continues to travel back and forth between Cambridge and Gombe for several years. Baron Hugo van Lawick, a photographer for National Geographic, begins taking photos and films at Gombe. 1964 Jane and Hugo marry in England and return to Gombe. -

Tinkering with Time the NEW TIME TRAVELERS: a JOURNEY to the on Our FRONTIERS of PHYSICS by DAVID TOOMEY Bookshelf W
BOOKS & ARTS Tinkering with time THE NEW TIME TRAVELERS: A JOURNEY TO THE On our FRONTIERS OF PHYSICS BY DAVID TOOMEY bookshelf W. W. Norton & Co.: 2007. 320 pp. $25.95 Years ago, David Toomey picked up H. G. Wells’ moving clocks tick slowly, making time travel The Time Machine and couldn’t put it down. to the future possible. We now know a number The Mathematics of He was most interested in the drawing-room of solutions to Einstein’s equations of general Egypt, Mesopotamia, discussion between the time traveller and his relativity (1915) that are sufficiently twisted to China, India, and Islam: friends in which time as a fourth dimension was allow time travel to the past: Kurt Gödel’s 1949 A Sourcebook discussed, but wanted to know more about just rotating universe; the Morris–Thorne–Yurtsever edited by Victor J. Katz how that time machine might work. Toomey was wormhole (1988); the Tipler–van Stockum infinite therefore delighted to learn that that drawing- rotating cylinder, moving cosmic strings (myself), Princeton Univ. Press: room conversation continues today — this time the rotating black-hole interior (Brandon Carter), 2007. 685 pp. $75 among physicists. a Roman ring of wormholes (Matt Visser), the We’re aware that Toomey captures well the personalities Everett–Alcubierre warp drive, my and Li–Xin Li’s the ancient cultures of the ‘new time travelers’ — those physicists self-creating universe; Amos Ori’s torus; and were mathematically interested in whether time travel to the past is others. The book discusses all of these. advanced. Now possible — from Stephen Hawking’s sense of But can a time machine really be constructed? translations of early texts humour to Kip Thorne’s penchant for placing Hawking, like one of the time traveller’s sceptical from five key regions are scientific bets. -

ACCRETION INTO and EMISSION from BLACK HOLES Thesis By
ACCRETION INTO AND EMISSION FROM BLACK HOLES Thesis by Don Nelson Page In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy California Institute of Technology Pasadena, California 1976 (Submitted May 20, 1976) -ii- ACKNOHLEDG:-IENTS For everything involved during my pursuit of a Ph. D. , I praise and thank my Lord Jesus Christ, in whom "all things were created, both in the heavens and on earth, visible and invisible, whether thrones or dominions or rulers or authorities--all things have been created through Him and for Him. And He is before all things, and in Him all things hold together" (Colossians 1: 16-17) . But He is not only the Creator and Sustainer of the universe, including the physi cal laws which rule and their dominion the spacetime manifold and its matter fields ; He is also my personal Savior, who was "wounded for our transgressions , ... bruised for our iniquities, .. and the Lord has lald on Him the iniquity of us all" (Isaiah 53:5-6). As the Apostle Paul expressed it shortly after Isaiah ' s prophecy had come true at least five hundred years after being written, "God demonstrates His own love tmvard us , in that while we were yet sinners, Christ died for us" (Romans 5 : 8) . Christ Himself said, " I have come that they may have life, and have it to the full" (John 10:10) . Indeed Christ has given me life to the full while I have been at Caltech, and I wish to acknowledge some of the main blessings He has granted: First I thank my advisors , KipS. -

West African Chimpanzees
Status Survey and Conservation Action Plan West African Chimpanzees Compiled and edited by Rebecca Kormos, Christophe Boesch, Mohamed I. Bakarr and Thomas M. Butynski IUCN/SSC Primate Specialist Group IUCN The World Conservation Union Donors to the SSC Conservation Communications Programme and West African Chimpanzees Action Plan The IUCN Species Survival Commission is committed to communicating important species conservation information to natural resource managers, decision makers and others whose actions affect the conservation of biodiversity. The SSC’s Action Plans, Occasional Papers, newsletter Species and other publications are supported by a wide variety of generous donors including: The Sultanate of Oman established the Peter Scott IUCN/SSC Action Plan Fund in 1990. The Fund supports Action Plan development and implementation. To date, more than 80 grants have been made from the Fund to SSC Specialist Groups. The SSC is grateful to the Sultanate of Oman for its confidence in and support for species conservation worldwide. The Council of Agriculture (COA), Taiwan has awarded major grants to the SSC’s Wildlife Trade Programme and Conser- vation Communications Programme. This support has enabled SSC to continue its valuable technical advisory service to the Parties to CITES as well as to the larger global conservation community. Among other responsibilities, the COA is in charge of matters concerning the designation and management of nature reserves, conservation of wildlife and their habitats, conser- vation of natural landscapes, coordination of law enforcement efforts, as well as promotion of conservation education, research, and international cooperation. The World Wide Fund for Nature (WWF) provides significant annual operating support to the SSC. -

SCIENCE and SUSTAINABILITY Impacts of Scientific Knowledge and Technology on Human Society and Its Environment
EM AD IA C S A C I A E PONTIFICIAE ACADEMIAE SCIENTIARVM ACTA 24 I N C T I I F A I R T V N Edited by Werner Arber M O P Joachim von Braun Marcelo Sánchez Sorondo SCIENCE and SUSTAINABILITY Impacts of Scientific Knowledge and Technology on Human Society and Its Environment Plenary Session | 25-29 November 2016 Casina Pio IV | Vatican City LIBRERIA EDITRICE VATICANA VATICAN CITY 2020 Science and Sustainability. Impacts of Scientific Knowledge and Technology on Human Society and its Environment Pontificiae Academiae Scientiarvm Acta 24 The Proceedings of the Plenary Session on Science and Sustainability. Impacts of Scientific Knowledge and Technology on Human Society and its Environment 25-29 November 2016 Edited by Werner Arber Joachim von Braun Marcelo Sánchez Sorondo EX AEDIBVS ACADEMICIS IN CIVITATE VATICANA • MMXX The Pontifical Academy of Sciences Casina Pio IV, 00120 Vatican City Tel: +39 0669883195 • Fax: +39 0669885218 Email: [email protected] • Website: www.pas.va The opinions expressed with absolute freedom during the presentation of the papers of this meeting, although published by the Academy, represent only the points of view of the participants and not those of the Academy. ISBN 978-88-7761-113-0 © Copyright 2020 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form, or by any means, electronic, mechanical, recording, pho- tocopying or otherwise without the expressed written permission of the publisher. PONTIFICIA ACADEMIA SCIENTIARVM LIBRERIA EDITRICE VATICANA VATICAN CITY The climate is a common good, belonging to all and meant for all. -

Remembering Dian Fossey: Primatology, Celebrity, Mythography
Kunapipi Volume 34 Issue 2 Article 16 2012 Remembering Dian Fossey: Primatology, Celebrity, Mythography Graham Huggan Follow this and additional works at: https://ro.uow.edu.au/kunapipi Part of the Arts and Humanities Commons Recommended Citation Huggan, Graham, Remembering Dian Fossey: Primatology, Celebrity, Mythography, Kunapipi, 34(2), 2012. Available at:https://ro.uow.edu.au/kunapipi/vol34/iss2/16 Research Online is the open access institutional repository for the University of Wollongong. For further information contact the UOW Library: [email protected] Remembering Dian Fossey: Primatology, Celebrity, Mythography Abstract It is generally accepted today that the turbulent life of the American primatologist Dian Fossey developed over time into the stuff of legend; so much so that its singularly nasty end — she was murdered in 1985 in circumstances that are still far from certain — is seen by some as ‘something she might well have made up for herself’ (Torgovnick 91). Fossey’s celebrity (or, perhaps better, her notoriety) is attributable to several different factors, not least the 1988 Hollywood film (Gorillas in the Mist) celebrating her exploits. This journal article is available in Kunapipi: https://ro.uow.edu.au/kunapipi/vol34/iss2/16 136 GRAHAM HUGGAN Remembering Dian Fossey: primatology, Celebrity, Mythography It is generally accepted today that the turbulent life of the American primatologist Dian Fossey developed over time into the stuff of legend; so much so that its singularly nasty end — she was murdered in 1985 in circumstances that are still far from certain — is seen by some as ‘something she might well have made up for herself’ (Torgovnick 91).