Corticosteroids for Acute Rhinosinusitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -
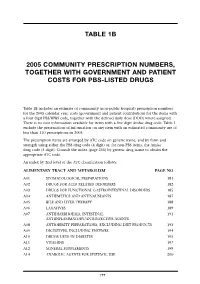
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

Laaketilasto07 2.Pdf
Keskeisiä lukuja lääkkeiden myynnistä ja lääkekorvauksista vuonna 2007 Muutos vuodesta 2006 Lääkkeiden kokonaismyynti 2 500 milj. € 5,9 % avohoidon reseptilääkkeiden myynti (verollisin vähittäismyyntihinnoin) 1 817 milj. € 4,2 % avohoidon itsehoitolääkkeiden myynti (verollisin vähittäismyyntihinnoin) 275 milj. € 15,5 % sairaalamyynti (tukkuohjehinnoin) 408 milj. € 7,5 % Lääkkeistä maksetut korvaukset 1 142 milj. € 3,8 % peruskorvaukset 369 milj. € 0,6 % erityiskorvaukset 662 milj. € 6,8 % lisäkorvaukset 111 milj. € -2,3 % Key figures for medicine sales and their reimbursement in 2007 Change from 2006 Total sales of pharmaceuticals EUR 2,500 million 5.9% prescription medicines in outpatient care (at pharmacy prices with VAT) EUR 1,817 million 4.2% OTC medicines in outpatient care (at pharmacy prices with VAT) EUR 275 million 15.5% sales to hospitals (at wholesale prices) EUR 408 million 7.5% Reimbursement of medicine costs EUR 1,142 million 3.8% Basic Refunds EUR 369 million 0.6% Special Refunds EUR 662 million 6.8% Additional Refunds EUR 111 million -2.3% SUOMEN LÄÄKETILASTO FINNISH STATISTICS ON MEDICINES 2007 Lääkelaitos ja Kansaneläkelaitos National Agency for Medicines and Social Insurance Institution Helsinki 2008 LÄÄKELAITOS KANSANELÄKELAITOS NATIONAL AGENCY SOCIAL INSURANCE FOR MEDICINES INSTITUTION Lääketurvaosasto Tutkimusosasto Department of Safety Research Department and Drug Information Mannerheimintie 103b Nordenskiöldinkatu 12 P.O. Box 55 P.O. Box 450 FI-00301 Helsinki FI-00101 Helsinki Finland Finland Puh. (09) 473 341 Puh. 020 634 11 Tel. +358 9 473 341 Tel. +358 20 634 11 Telekopio (09) 473 34297 Telekopio 020 634 1700 Fax +358 9 473 34297 Fax +358 20 634 1700 ISSN 0786-2180 Kansi / Cover: Kari Piippo Edita Prima Oy Helsinki 2008 SISÄLLYS Kuvaluettelo ..................................................................................................................... -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -
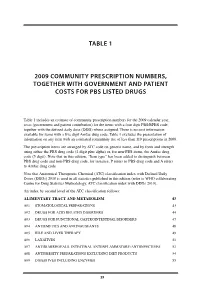
Table 1 2009 Community Prescription Numbers
TABLE 1 2009 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS LISTED DRUGS Table 1 includes an estimate of community prescription numbers for the 2009 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 excludes the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2009. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit plus alpha) or, for non-PBS items, the Amfac drug code (5 digit). Note that in this edition, “Item type” has been added to distinguish between PBS drug code and non-PBS drug code, for instance, P refers to PBS drug code and A refers to Amfac drug code. Note that Anatomical Therapeutic Chemical (ATC) classification index with Defined Daily Doses (DDDs) 2010 is used in all statistics published in this edition (refer to WHO collaborating Centre for Drug Statistics Methodology, ATC classification index with DDDs 2010). An index by second level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM 43 A01 STOMATOLOGICAL PREPARATIONS 43 A02 DRUGS FOR ACID RELATED DISORDERS 44 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 47 A04 ANTIEMETICS AND ANTINAUSEANTS 48 A05 BILE AND LIVER THERAPY 49 A06 LAXATIVES 51 A07 ANTIDIARRHOEALS, INTESTINAL ANTIINFLAMMATORY/ANTIINFECTIVES -

The Selection and Use of Essential Medicines
WHO Technical Report Series 958 THE SELECTION AND USE OF ESSENTIAL MEDICINES This report presents the recommendations of the WHO Expert THE SELECTION AND USE Committee responsible for updating the WHO Model List of Essential Medicines. The fi rst part contains a review of the OF ESSENTIAL MEDICINES report of the meeting of the Expert Subcommittee on the Selection and Use of Essential Medicines, held in October 2008. It also provides details of new applications for paediatric medicines and summarizes the Committee’s considerations and justifi cations for additions and changes to the Model List, including its recommendations. Part Two of the publication is the report of the second meeting of the Subcommittee of the Expert Committee on the Selection and Use of Essential Medicines. Annexes include the revised version of the WHO Model List of Essential Medicines (the 16th) and the revised version of the WHO Model List of Report of the WHO Expert Committee, 2009 Essential Medicines for Children (the 2nd). In addition there is a list of all the items on the Model List sorted according to their (including the 16th WHO Model List of Essential Medicines Anatomical Therapeutic Chemical (ATC) classifi cation codes. and the 2nd WHO Model List of Essential Medicines for Children) WHO Technical Report Series — 958 WHO Technical ISBN 978-92-4-120958-8 Geneva TTRS958cover.inddRS958cover.indd 1 110.06.100.06.10 008:328:32 The World Health Organization was established in 1948 as a specialized agency of the United Nations serving as the directing and coordinating authority for SELECTED WHO PUBLICATIONS OF RELATED INTEREST international health matters and public health. -

Review of Existing Classification Efforts
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.1.1 Review of existing classification efforts Due date of deliverable: (15.01.2008) Actual submission date: (07.02.2008) Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UGent Revision 1.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public X PP Restricted to other programme participants (including the Commission Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) Task 4.1 : Review of existing classification efforts Authors: Kristof Pil, Elke Raes, Thomas Van den Neste, An-Sofie Goessaert, Jolien Veramme, Alain Verstraete (Ghent University, Belgium) Partners: - F. Javier Alvarez (work package leader), M. Trinidad Gómez-Talegón, Inmaculada Fierro (University of Valladolid, Spain) - Monica Colas, Juan Carlos Gonzalez-Luque (DGT, Spain) - Han de Gier, Sylvia Hummel, Sholeh Mobaser (University of Groningen, the Netherlands) - Martina Albrecht, Michael Heiβing (Bundesanstalt für Straßenwesen, Germany) - Michel Mallaret, Charles Mercier-Guyon (University of Grenoble, Centre Regional de Pharmacovigilance, France) - Vassilis Papakostopoulos, Villy Portouli, Andriani Mousadakou (Centre for Research and Technology Hellas, Greece) DRUID 6th Framework Programme Deliverable D.4.1.1. Revision 1.0 Review of Existing Classification Efforts Page 2 of 127 Introduction DRUID work package 4 focusses on the classification and labeling of medicinal drugs according to their influence on driving performance. -

Reseptregisteret 2014–2018 the Norwegian Prescription Database 2014–2018
LEGEMIDDELSTATISTIKK 2019:2 Reseptregisteret 2014–2018 The Norwegian Prescription Database 2014–2018 Reseptregisteret 2014–2018 The Norwegian Prescription Database 2014–2018 Christian Lie Berg Kristine Olsen Solveig Sakshaug Utgitt av Folkehelseinstituttet / Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2019 Tittel/Title: Legemiddelstatistikk 2019:2 Reseptregisteret 2014–2018 / The Norwegian Prescription Database 2014–2018 Forfattere/Authors: Christian Berg, redaktør/editor Kristine Olsen Solveig Sakshaug Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no / The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon / Contact information: Folkehelseinstituttet / Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8406-014-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2014–2018 [The Norwegian Prescription Database 2014–2018] Legemiddelstatistikk 2019:2, Oslo, Norge: Folkehelseinstituttet, 2019. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian -

Evaluation of the Affordable Medicines Programme in Ukraine
EVALUATION OF THE AFFORDABLE MEDICINES PROGRAMME IN UKRAINE EVALUATION OF THE AFFORDABLE MEDICINES PROGRAMME IN UKRAINE Health Technologies and Pharmacies Division of Health Systems and Public Health Abstract This report reviews and analyses the Affordable Medicines Programme, which was introduced in Ukraine in April 2017 to provide patients with improved access to 23 outpatient medicines for the treatment of chronic noncommunicable diseases. The evaluation combines both quantitative and qualitative analysis. The findings confirm that the Programme has contributed to a significant increase in access to needed outpatient medicines in Ukraine. Further, while implementation was successful overall, uptake across regions was uneven. The report concludes by listing a number of policy options to support the sustainability and expansion of the Affordable Medicines Programme. Keywords UNIVERSAL HEALTH COVERAGE AFFORDABLE MEDICINES UKRAINE ACCESS TO OUTPATIENT MEDICINES FINANCIAL PROTECTION ISBN 978 92 890 5400 3 Address requests about publications of the WHO Regional Office for Europe to: Publications WHO Regional Office for Europe UN City, Marmorvej 51 DK-2100 Copenhagen Ø, Denmark Alternatively, complete an online request form for documentation, health information, or for permission to quote or translate, on the Regional Office website (http://www.euro.who.int/pubrequest). © World Health Organization 2019 All rights reserved. The Regional Office for Europe of the World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Evaluation of Carcinogenicity Studies of Medicinal Products for Human Use Authorised Via the European Centralised Procedure
Regulatory Toxicology and Pharmacology xxx (2011) xxx–xxx Contents lists available at ScienceDirect Regulatory Toxicology and Pharmacology journal homepage: www.elsevier.com/locate/yrtph Evaluation of carcinogenicity studies of medicinal products for human use authorised via the European centralised procedure (1995–2009) ⇑ Anita Friedrich a, , Klaus Olejniczak b a Granzer Regulatory Consulting and Services, Zielstattstrasse 44, 81379 Munich, Germany b Federal Institute for Drugs and Medical Devices, Kurt-Georg-Kiesinger-Allee 3, 53175 Bonn, Germany article info abstract Article history: Carcinogenicity data of medicinal products for human use that have been authorised via the European Received 25 October 2010 centralised procedure (CP) between 1995 and 2009 were evaluated. Carcinogenicity data, either from Available online xxxx long-term rodent carcinogenicity studies, transgenic mouse studies or repeat-dose toxicity studies were available for 144 active substances contained in 159 medicinal products. Out of these compounds, 94 Keywords: (65%) were positive in at least one long-term carcinogenicity study or in repeat-dose toxicity studies. Medicinal products Fifty compounds (35%) showed no evidence of a carcinogenic potential. Out of the 94 compounds with Carcinogenicity positive findings in either carcinogenicity or repeat-dose toxicity studies, 33 were positive in both mice Rodents and rats, 40 were positive in rats only, and 21 were positive exclusively in mice. Long-term carcinogenic- ity studies in two rodent species were available for 116 compounds. Data from one long-term carcinoge- nicity study in rats and a transgenic mouse model were available for eight compounds. For 13 compounds, carcinogenicity data were generated in only one rodent species. One compound was exclu- sively tested in a transgenic mouse model. -

National Licensed Medicine List of Afghanistan
islamic republic of afghanistan ministry of public health general directorate of pharmaceutical affairs avicenna pharmaceutical institute National Licensed Medicine List of Afghanistan 2014 2 NATIONAL LICENSED MEDICINES LIST OF AFGHANISTAN Preface With thanks to God for enabling us, we present this revision of the national essential medicines list (EML) and the licensed medicines list (LML) of Afghanistan. These documents are critical to the delivery of quality health services across the country. The policy of the Ministry of Public Health (MoPH) of the Islamic Republic of Afghanistan includes ensuring that the population of Afghanistan has access to safe, effective, and affordable medicines to treat its primary health problems. The EML includes the medicines needed for adequately addressing the priority health problems defined in the MoPH’s health strategy. The LML includes the medicines listed in the EML and additional medicines for conditions not included as priorities in the present strategy and medicines used in private sector. The MoPH developed and published the national EML of Afghanistan for the first time in 1995 and the LML in 2003; the last revision and publication occurred in 2007. The EML and LML should be revised regularly in response to the rapid expansion of basic health services in Afghanistan since 2003, the changing of internationally and nationally recommended treatment protocols for some diseases, the presence of new and emergent diseases, and the withdrawal of some toxic medicines from treatment guidelines. To revise the EML and LML, the MoPH authorized the National Medicine Selection Committee (NMSC) to develop a detailed procedure for inclusion or exclusion of medicines from the 2007 lists.