Prior Authorization Protocol NATL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GLP-1 Receptor Agonists
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in- development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain health, as well as for age-related health concerns that can affect brain health (e.g., cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports include evaluation of safety data, from clinical trials if available, and from preclinical models. GLP-1 Receptor Agonists Evidence Summary GLP-1 agonists are beneficial for patients with type 2 diabetes and obesity. Some evidence suggests benefits for Alzheimer’s disease. It is unclear whether it is beneficial for individuals without underlying metabolic disease. Semaglutide seems to be most effective for metabolic dysfunction, though liraglutide has more preclinical data for Alzheimer’s disease. Neuroprotective Benefit: Evidence from many preclinical studies and a pilot biomarker study suggest some neuroprotective benefits with GLP-1 agonists. However, whether they may be beneficial for everyone or only a subset of individuals (e.g. diabetics) is unclear. Aging and related health concerns: GLP-1 agonists are beneficial for treating diabetes and cardiovascular complications relating to diabetes. It is not clear whether they have beneficial effects in otherwise healthy individuals. Safety: GLP-1 agonists are generally safe for most people with minor side effects. However, long-term side effects are not known. 1 Availability: Available Dose: Varies - see Chemical formula: C172H265N43O51 (Liraglutide) as a prescription chart at the end of MW: 3751.262 g/mol medicine. -

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

(Pram) and Insulin A21G Improves Post-Prandial Glucose Vs Novolog
ADO09, A Co-Formulation Of Pramlintide (Pram) and Insulin A21G improves Post-Prandial Glucose Vs Novolog® in Type 1 Diabetes (T1DM) G.Meiffren¹, G.Andersen², R.Eloy¹, C.Seroussi¹, C.Mégret¹, S.Famulla², Y.-P Chan¹, M.Gaudier¹, O.Soula¹, J.H. DeVries²,T.Heise² (1 Adocia, Lyon, France ; 2 Profil, Neuss, Germany) Introduction & Background Overall safety Outpatient period results - CGM metrics o ADO09 (M1Pram) is a co-formulation of pramlintide and insulin A21G o Both treatments were well tolerated without any treatment-related serious adverse events o Most of the CGM metrics (TiR [70-180], TiR [80-140], mean blood glucose per day), were significantly improved developed to leverage the beneficial effects of pramlintide on post-prandial (Table 2). As expected M1Pram had numerically more, mostly gastrointestinal adverse events with M1Pram (Table 4). Postprandial and mean 24-hour glucose profiles were improved with M1Pram (Fig. 3) glucose without additional injections than insulin aspart Table 4: CGM metrics, all days. Significant differences are marked in bold Objective and design o No severe hypoglycemia were seen, slightly more hypoglycemic events occurred with M1Pram Ratio of LSMean* o To compare the effect of M1Pram and insulin aspart (Novolog®, Novo than with aspart (Table 3) Difference Parameter Treatment LS Mean M1Pram / Aspart P-value Nordisk) on post-prandial glucose control, glycemic control assessed by Table 2: Incidence of adverse events throughout the trial (M1Pram-Aspart) (95% CI) CGM and safety/tolerability M1Pram Aspart M1Pram -

125469Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125469Orig1s000 SUMMARY REVIEW Division Director Review 1. Introduction On September 18, 2013 Eli Lilly and Company submitted a Biologics License Application (BLA) for Trulicity under section 351 of the Public Health Service Act. The applicant is seeking to indicate Trulicity as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Trulicity is a solution for injection containing either 0.75 or 1.5 mg of dulaglutide [i.e., a glucagon-like peptide 1 (GLP-1) receptor agonist]. Trulicity is to be administered by subcutaneous injection at once weekly intervals. Once approved, Trulicity will be the fifth GLP-1 agonist indicated for use in the management of patients with type 2 diabetes mellitus in the United States. This document serves as the division director’s memorandum for the application. 2. Background The drug substance in Trulicity is dulaglutide. In this memorandum, I will use Trulicity and dulaglutide interchangeably. Dulaglutide is a homodimer that consists of two identical polypeptide chains linked to each other by a disulfide bond. The polypeptide chain is a fusion protein that consists of a glucagon-like peptide 1 (GLP-1) variant, a linker, and the Fc portion of a human IgG4 variant antibody. The GLP-1 analog portion of dulaglutide is (b) (4) homologous to native human GLP-1 (7-37) (b) (4) (b) (4) Dulaglutide was demonstrated to bind and activate the GLP-1 receptor. The biological effects of endogenous GLP-1 on glucose homeostasis include augmentation of glucose stimulated insulin secretion, inhibition of glucagon release, and delay of gastric emptying. -
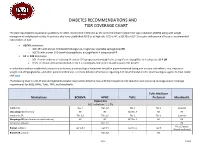
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -
GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal
Clinical Policy: GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal See Important Reminder at the end of this policy for important regulatory and legal information. Description The following are GLP-1 Receptor Agonists requiring prior authorization: lixisenatide (Adlyxin™), Exenatide Extended-Release (Bydureon®), Exenatide (Byetta®), Pramlintide Acetate (Symlin®), Albiglutide (Tanzeum®), Dulaglutide (Trulicity®), Liraglutide (Victoza®), Liraglutide and insulin degludec (Xultophy®),Insulin glargine and lixisenatide (Soliqua®). FDA approved indication Adlyxin, Bydureon, Byetta, Tanzeum, Trulicity, Victoza are indicated: As an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Adlyxin limitation of use: Has not been studied in patients with chronic pancreatitis or a history of unexplained pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Not for treatment of type 1 diabetes or diabetic ketoacidosis. Has not been studied in combination with short acting insulin. Has not been studied in patients with gastroparesis and is not recommended in patients with gastroparesis. Bydureon limitation of use: Not recommended as first-line therapy for patients inadequately controlled on diet and exercise. Should not be used to treat type 1 diabetes or diabetic ketoacidosis. Use with insulin has not been studied and is not recommended. Has not been studied in patients with a history of pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Byetta limitation of use: Not a substitute for insulin. Byetta should not be used for the treatment of type 1 diabetes or diabetic ketoacidosis. -

New Drug Update
7/1/2014 New Drug Update LaKeisha Williams, PharmD, MSPH Drug Information Specialist Xavier University of Louisiana College of Pharmacy LPA Annual Convention –July 18, 2014 Speaker Disclosures • The speaker declares no conflicts of interest, real or apparent, and no financial interests in any company, product, or service mentioned in this program. 1 7/1/2014 Learning Objectives • At the completion of this activity, PHARMACISTS will be able to: – Recognize the clinical indications for selected new therapeutic agents approved by the Food and Drug Administration (FDA). – Explain the mechanisms of action for new therapeutic agents discussed. – Identify common adverse reactions, relevant drug interactions and key contraindications for the new approved therapeutic agents. – Discuss pertinent patient education for newly approved agents. Learning Objectives • At the completion of this activity, PHARMACY TECHNICIANS will be able to: – Describe selected new therapeutic agents approved by the Food and Drug Administration (FDA). – Recognize the indications of selected new therapeutic agents. – Summarize adverse reactions and precautions when evaluating FDA approved agents. – List counseling tips for newly approved therapeutic agents. 2 7/1/2014 New Drug Approvals of 2013 • Food and Drug Administration (FDA) approved 27 new molecular entities (NMEs) – More than a third (36%) of novel drugs approved are for rare diseases – Nearly one out of three (32%) are the first in their class – Approximately three‐quarters (72%) of novel drugs were first approved in the U.S. Jenkins J. U.S. Food and Drug Administration/FY 2013 New Drug Review. www.fda.gov New Drug Approvals of 2014 • Food and Drug Administration (FDA) approved 16 new molecular entities (NMEs) – Innovative new products that never before have been used in clinical practice – Many contain active moieties that have not been approved by FDA previously, either as a single ingredient drug or as part of a combination product Food and Drug Administration. -

Tresiba-Product-Monograph.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION TRESIBA® insulin degludec injection TRESIBA® FlexTouch® 100 U/mL, Solution for injection in a pre-filled pen TRESIBA® FlexTouch® 200 U/mL, Solution for injection in a pre-filled pen Subcutaneous Antidiabetic Agent Long-Acting Basal Insulin Analogue ATC Code: A10AE06 Novo Nordisk Canada Inc. Date of Initial Authorization: AUG 25, 2017 101-2476 Argentia Road Date of Revision: Mississauga, Ontario JUL 23, 2021 Canada L5N 6M1 Submission Control Number: 250276 Product Monograph Master Template Template Date: September 2020 TRESIBA® (insulin degludec injection) Page 1 of 2 RECENT MAJOR LABEL CHANGES 7 Warnings and Precautions 03/2021 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS ..............................................................................................................2 1 INDICATIONS ..................................................................................................................4 1.1 Pediatrics ................................................................................................................4 1.2 Geriatrics ................................................................................................................4 2 CONTRAINDICATIONS ..................................................................................................4 3 SERIOUS WARNINGS AND PRECAUTIONS BOX .......................................................4 4 DOSAGE AND ADMINISTRATION -
What to Do After Basal Insulin
BASALINSULIN What to Do After Basal Insulin 3 Treatment Strategies for Type 2 Diabetes These strategies can help you optimize glucose control in your patient with type 2 diabetes when basal insulin alone is insufficient. Lubaina Presswala, DO, Jay Shubrook, DO, FAAFP, FACOFP, BC-ADM iabetes mellitus is a complex, progressive disease that af- Practice fects every primary care provider’s practice. Major diabe- recommendations tes organizations recommend that treatment be ongoing • Intensify diabetes treatment D and progressive in order to control the disease. The American Dia- for patients who have a normal betes Association (ADA), the European Association for the Study fasting glucose but an A1C > 7% of Diabetes (EASD), and the American Association of Clinical En- and daytime hyperglycemia, and for those who are not at goal docrinologists recommend that patients be assessed every two to despite basal insulin doses three months after diagnosis and that treatment should be intensi- 1,2 > 0.5 U/kg/d. B fied if the patient is not meeting treatment goals. Using this ap- • Consider intensifying diabetes proach, all people with type 2 diabetes could be on insulin one management beyond basal insulin year after diagnosis.1,2 therapy by adding a glucagon-like While many clinicians have become comfortable with using peptide 1 receptor agonist, insulin once-daily basal insulin, such as glargine or detemir, what to do prior to one meal each day, or after basal insulin is much more complex. This review explains insulin prior to all meals. C three strategies to consider when basal insulin alone isn’t enough. -

Glucagon-Like Peptide-1 and Its Class BG Protein–Coupled Receptors
1521-0081/68/4/954–1013$25.00 http://dx.doi.org/10.1124/pr.115.011395 PHARMACOLOGICAL REVIEWS Pharmacol Rev 68:954–1013, October 2016 Copyright © 2016 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: RICHARD DEQUAN YE Glucagon-Like Peptide-1 and Its Class B G Protein–Coupled Receptors: A Long March to Therapeutic Successes Chris de Graaf, Dan Donnelly, Denise Wootten, Jesper Lau, Patrick M. Sexton, Laurence J. Miller, Jung-Mo Ahn, Jiayu Liao, Madeleine M. Fletcher, Dehua Yang, Alastair J. H. Brown, Caihong Zhou, Jiejie Deng, and Ming-Wei Wang Division of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands (C.d.G.); School of Biomedical Sciences, University of Leeds, Leeds, United Kingdom (D.D.); Drug Discovery Biology Theme and Department of Pharmacology, Monash Institute of Pharmaceutical Sciences, Parkville, Victoria, Australia (D.W., P.M.S., M.M.F.); Protein and Peptide Chemistry, Global Research, Novo Nordisk A/S, Måløv, Denmark (J.La.); Department of Molecular Pharmacology and Experimental Therapeutics, Mayo Clinic, Scottsdale, Arizona (L.J.M.); Department of Chemistry and Biochemistry, University of Texas at Dallas, Richardson, Texas (J.-M.A.); Department of Bioengineering, Bourns College of Engineering, University of California at Riverside, Riverside, California (J.Li.); National Center for Drug Screening and CAS Key Laboratory of Receptor Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, China (D.Y., C.Z., J.D., M.-W.W.); Heptares Therapeutics, BioPark, Welwyn Garden City, United Kingdom (A.J.H.B.); and School of Pharmacy, Fudan University, Zhangjiang High-Tech Park, Shanghai, China (M.-W.W.) Downloaded from Abstract. -

Ep 2330124 A2
(19) TZZ ¥¥Z_ T (11) EP 2 330 124 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.06.2011 Bulletin 2011/23 C07K 14/575 (2006.01) (21) Application number: 10012149.0 (22) Date of filing: 11.08.2006 (84) Designated Contracting States: • Lewis, Diana AT BE BG CH CY CZ DE DK EE ES FI FR GB GR San Diego, CA 92121 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Soares, Christopher J. SK TR San Diego, CA 92121 (US) • Ghosh, Soumitra S. (30) Priority: 11.08.2005 US 201664 San Diego, CA 92121 (US) 17.08.2005 US 206903 • D’Souza, Lawrence 12.12.2005 US 301744 San Diego, CA 92121 (US) • Parkes, David G. (62) Document number(s) of the earlier application(s) in San Diego, CA 92121 (US) accordance with Art. 76 EPC: • Mack, Christine M. 06801467.9 / 1 922 336 San Diego, CA 92121 (US) • Forood, Behrouz Bruce (71) Applicant: Amylin Pharmaceuticals Inc. San Diego, CA 92121 (US) San Diego, CA 92121 (US) (74) Representative: Gowshall, Jonathan Vallance et al (72) Inventors: Forrester & Boehmert • Levy, Odile Esther Pettenkoferstrasse 20-22 San Diego, CA 92121 (US) 80336 München (DE) • Hanley, Michael R. San Diego, CA 92121 (US) Remarks: • Jodka, Carolyn M. This application was filed on 30-09-2010 as a San Diego, CA 92121 (US) divisional application to the application mentioned under INID code 62. (54) Hybrid polypeptides with selectable properties (57) The present invention relates generally to novel, tions and disorders include, but are not limited to, hyper- selectable hybrid polypeptides useful as agents for the tension, dyslipidemia, cardiovascular disease, eating treatment and prevention of metabolic diseases and dis- disorders, insulin-resistance, obesity, and diabetes mel- orders which can be alleviated by control plasma glucose litus of any kind, including type 1, type 2, and gestational levels, insulin levels, and/or insulin secretion, such as diabetes. -

Maikawa STM 2021.Pdf
SCIENCE TRANSLATIONAL MEDICINE | REVIEW DRUG DEVELOPMENT Copyright © 2021 The Authors, some rights reserved; Engineering biopharmaceutical formulations exclusive licensee American Association to improve diabetes management for the Advancement Caitlin L. Maikawa1, Andrea I. d’Aquino2, Rayhan A. Lal3,4,5, of Science. No claim 4,5 1,2,4,5,6 to original U.S. Bruce A. Buckingham , Eric A. Appel * Government Works Insulin was first isolated almost a century ago, yet commercial formulations of insulin and its analogs for hormone replacement therapy still fall short of appropriately mimicking endogenous glycemic control. Moreover, the controlled delivery of complementary hormones (such as amylin or glucagon) is complicated by instability of the pharmacologic agents and complexity of maintaining multiple infusions. In this review, we highlight the advantages and limitations of recent advances in drug formulation that improve protein stability and pharmacokinetics, prolong drug delivery, or enable alternative dosage forms for the management of diabetes. With controlled delivery, Downloaded from these formulations could improve closed-loop glycemic control. ENGINEERING OPPORTUNITIES TO IMPROVE DIABETES tive treatment with insulin alone is already highly burdensome and MANAGEMENT costly—requiring frequent glucose monitoring, mealtime insulin Over the past century, insulin replacement therapy has been impera- boluses, basal insulin delivery through infusion pumps or long-acting http://stm.sciencemag.org/ tive to saving lives and improving diabetes treatment outcomes. The analogs, and routine carbohydrate counting—and still does not truly administration of exogenous insulin prevents ketoacidosis, which recapitulate the complexities of metabolic control in nondiabetic was once a universally fatal condition. Although insulin has histor- individuals (Fig. 1B) (7).