What to Do After Basal Insulin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GLP-1 Receptor Agonists
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in- development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain health, as well as for age-related health concerns that can affect brain health (e.g., cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports include evaluation of safety data, from clinical trials if available, and from preclinical models. GLP-1 Receptor Agonists Evidence Summary GLP-1 agonists are beneficial for patients with type 2 diabetes and obesity. Some evidence suggests benefits for Alzheimer’s disease. It is unclear whether it is beneficial for individuals without underlying metabolic disease. Semaglutide seems to be most effective for metabolic dysfunction, though liraglutide has more preclinical data for Alzheimer’s disease. Neuroprotective Benefit: Evidence from many preclinical studies and a pilot biomarker study suggest some neuroprotective benefits with GLP-1 agonists. However, whether they may be beneficial for everyone or only a subset of individuals (e.g. diabetics) is unclear. Aging and related health concerns: GLP-1 agonists are beneficial for treating diabetes and cardiovascular complications relating to diabetes. It is not clear whether they have beneficial effects in otherwise healthy individuals. Safety: GLP-1 agonists are generally safe for most people with minor side effects. However, long-term side effects are not known. 1 Availability: Available Dose: Varies - see Chemical formula: C172H265N43O51 (Liraglutide) as a prescription chart at the end of MW: 3751.262 g/mol medicine. -

A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D
Drugs 2005; 65 (3): 325-340 REVIEW ARTICLE 0012-6667/05/0003-0325/$39.95/0 2005 Adis Data Information BV. All rights reserved. A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D. Mooradian Division of Endocrinology, Department of Internal Medicine, Diabetes, and Metabolism, St Louis University School of Medicine, St Louis, Missouri, USA Contents Abstract ....................................................................................325 1. Physiology of Insulin Secretion .............................................................326 2. Conventional Insulin Preparations ..........................................................327 3. Insulin Analogues ........................................................................328 3.1 Rapid-Acting Insulin Analogues .......................................................328 3.1.1 Insulin Lispro ...................................................................328 3.1.2 Insulin Aspart ..................................................................329 3.1.3 Insulin Glulisine .................................................................329 3.1.4 Clinical Utility of Rapid-Acting Insulin Analogues ...................................330 3.2 Premixed Insulins and Insulin Analogues ................................................331 3.3 Basal Insulin Analogues ...............................................................331 3.3.1 Insulin Glargine ................................................................331 -

Byetta (Injection Pen) Usage & Safety Guide
Byetta (Injection Pen) Usage & Safety Guide - Drugs.com 04/07/2015 Tubeless Insulin Pump Tubeless, Reliable, Safe. Try The OmniPod®. Sign-Up For A Demo Kit! Browse all medications A B C D E F G H I J K L M N O P Q R S T U V W X Y Z Advanced Search Phonetic Search Drugs A-Z Pill Identifier Interactions Checker News Health Professionals Q & A Mednotes Apps Home → Conditions → Diabetes, Type 2 → Byetta Print Share Sign In or Register Byetta Related Information Availability Pregnancy Category Generic Name: exenatide (Byetta) (ex EN a tide) Prescription only Risk cannot be ruled out Brand Names: Byetta Prefilled Pen CSA Schedule Approval History Not a controlled drug FDA approved 2009 Overview Side Effects Dosage Interactions For Professionals More Reviews Average User Rating Prostate Cancer Stages 64 User Reviews 8.3 Rate it! See the Progression of Stages for Prostate Cancer. Get Expert Info Drug Class Incretin mimetics What is Byetta? Tubeless Byetta (exenatide) is an injectable diabetes Related Drugs medicine that helps control blood sugar levels . This medication helps Diabetes, Type 2 Insulin metformin your pancreas produce insulin more efficiently. insulin aspart Byetta is a short-acting form of exenatide. Januvia Pump Byetta is used to treat type 2 diabetes. Other glipizide Tubeless, diabetes medicines are sometimes used in glimepiride combination with Byetta if needed. Lantus Reliable, Invokana This medication guide provides information Victoza Safe. Try about the Byetta brand of exenatide. Bydureon glyburide is another brand of exenatide that is not Levemir The covered in this medication guide. -

125469Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 125469Orig1s000 SUMMARY REVIEW Division Director Review 1. Introduction On September 18, 2013 Eli Lilly and Company submitted a Biologics License Application (BLA) for Trulicity under section 351 of the Public Health Service Act. The applicant is seeking to indicate Trulicity as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Trulicity is a solution for injection containing either 0.75 or 1.5 mg of dulaglutide [i.e., a glucagon-like peptide 1 (GLP-1) receptor agonist]. Trulicity is to be administered by subcutaneous injection at once weekly intervals. Once approved, Trulicity will be the fifth GLP-1 agonist indicated for use in the management of patients with type 2 diabetes mellitus in the United States. This document serves as the division director’s memorandum for the application. 2. Background The drug substance in Trulicity is dulaglutide. In this memorandum, I will use Trulicity and dulaglutide interchangeably. Dulaglutide is a homodimer that consists of two identical polypeptide chains linked to each other by a disulfide bond. The polypeptide chain is a fusion protein that consists of a glucagon-like peptide 1 (GLP-1) variant, a linker, and the Fc portion of a human IgG4 variant antibody. The GLP-1 analog portion of dulaglutide is (b) (4) homologous to native human GLP-1 (7-37) (b) (4) (b) (4) Dulaglutide was demonstrated to bind and activate the GLP-1 receptor. The biological effects of endogenous GLP-1 on glucose homeostasis include augmentation of glucose stimulated insulin secretion, inhibition of glucagon release, and delay of gastric emptying. -
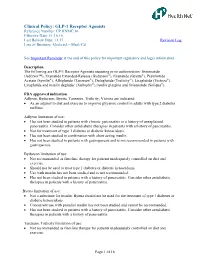
GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal
Clinical Policy: GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal See Important Reminder at the end of this policy for important regulatory and legal information. Description The following are GLP-1 Receptor Agonists requiring prior authorization: lixisenatide (Adlyxin™), Exenatide Extended-Release (Bydureon®), Exenatide (Byetta®), Pramlintide Acetate (Symlin®), Albiglutide (Tanzeum®), Dulaglutide (Trulicity®), Liraglutide (Victoza®), Liraglutide and insulin degludec (Xultophy®),Insulin glargine and lixisenatide (Soliqua®). FDA approved indication Adlyxin, Bydureon, Byetta, Tanzeum, Trulicity, Victoza are indicated: As an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Adlyxin limitation of use: Has not been studied in patients with chronic pancreatitis or a history of unexplained pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Not for treatment of type 1 diabetes or diabetic ketoacidosis. Has not been studied in combination with short acting insulin. Has not been studied in patients with gastroparesis and is not recommended in patients with gastroparesis. Bydureon limitation of use: Not recommended as first-line therapy for patients inadequately controlled on diet and exercise. Should not be used to treat type 1 diabetes or diabetic ketoacidosis. Use with insulin has not been studied and is not recommended. Has not been studied in patients with a history of pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Byetta limitation of use: Not a substitute for insulin. Byetta should not be used for the treatment of type 1 diabetes or diabetic ketoacidosis. -

New Drug Update
7/1/2014 New Drug Update LaKeisha Williams, PharmD, MSPH Drug Information Specialist Xavier University of Louisiana College of Pharmacy LPA Annual Convention –July 18, 2014 Speaker Disclosures • The speaker declares no conflicts of interest, real or apparent, and no financial interests in any company, product, or service mentioned in this program. 1 7/1/2014 Learning Objectives • At the completion of this activity, PHARMACISTS will be able to: – Recognize the clinical indications for selected new therapeutic agents approved by the Food and Drug Administration (FDA). – Explain the mechanisms of action for new therapeutic agents discussed. – Identify common adverse reactions, relevant drug interactions and key contraindications for the new approved therapeutic agents. – Discuss pertinent patient education for newly approved agents. Learning Objectives • At the completion of this activity, PHARMACY TECHNICIANS will be able to: – Describe selected new therapeutic agents approved by the Food and Drug Administration (FDA). – Recognize the indications of selected new therapeutic agents. – Summarize adverse reactions and precautions when evaluating FDA approved agents. – List counseling tips for newly approved therapeutic agents. 2 7/1/2014 New Drug Approvals of 2013 • Food and Drug Administration (FDA) approved 27 new molecular entities (NMEs) – More than a third (36%) of novel drugs approved are for rare diseases – Nearly one out of three (32%) are the first in their class – Approximately three‐quarters (72%) of novel drugs were first approved in the U.S. Jenkins J. U.S. Food and Drug Administration/FY 2013 New Drug Review. www.fda.gov New Drug Approvals of 2014 • Food and Drug Administration (FDA) approved 16 new molecular entities (NMEs) – Innovative new products that never before have been used in clinical practice – Many contain active moieties that have not been approved by FDA previously, either as a single ingredient drug or as part of a combination product Food and Drug Administration. -

Effective Switch from Twice-Daily Pre-Mixed Insulin 50/50 to Liraglutide to Achieve a Good Glycemic Control in Type 2 Diabetes
Elmer ress Case Report J Med Cases • 2011;2(2):76-80 Effective Switch From Twice-Daily Pre-Mixed Insulin 50/50 to Liraglutide to Achieve a Good Glycemic Control in Type 2 Diabetes Hidekatsu Yanaia, c, Taro Yoshimia, Ritsuko Hondab such gastrointestinal hormones. GLP-1 is produced mainly Abstract by L-cells in the ileum. GLP-1 is released into the blood from intestinal L-cells in response to meal ingestion, and GLP-1 The glucagon-like peptide 1 (GLP-1) stimulates insulin secretion stimulates insulin secretion from pancreatic β-cells in a glu- from pancreatic β-cells in a glucose-dependent manner. Therapeu- cose-dependent manner [1]. GLP-1 slows gastric emptying, tic strategies for type 2 diabetes mellitus are focused on the use which may aid weight loss, and inhibits glucagon release of GLP-1 analogues. Liraglutide, an acylated analogue of human from the pancreatic α-cells [1], improving insulin sensitivity. GLP-1, has been introduced in Japan in 2010. We will show a Therefore, therapeutic strategies for type 2 diabetes mel- 70-year-old woman with type 2 diabetes mellitus achieving a good litus are focused on the use of GLP-1 analogues. Exenatide glycemic control by switching from twice-daily pre-mixed insulin 50/50 to liraglutide. Measurements of plasma glucose and serum was introduced to the market in the United States in 2005 C-peptide levels before and after each meal ingestion and daily uri- and in Europe in 2007. Liraglutide has been introduced to nary C-peptide levels suggested that liraglutide ameliorates glucose the market in Europe in 2009 and in the United States and metabolism mainly not by the glucose-dependent insulinotropic Japan in 2010 [2]. -

Prior Authorization Protocol NATL
Prior Authorization Protocol BYDUREON™ (exenatide extended-release for injectable suspension), BYETTA TM (exenatide), SYMLIN PEN (pramlintide acetate), TANZEUM TM (albiglutide) TRULICITY™ (dulaglutide), VICTOZA ® (liraglutide) NATL Coverage of drugs is first determined by the member`s pharmacy or medical benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: • Bydureon, Byetta, Tanzeum, Trulicity, Victoza: An adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus • Symlin: Adjunctive treatment in patients with type 1 or type 2 diabetes who use mealtime insulin therapy and who have failed to achieve desired glucose control despite optimal insulin therapy. II. Health Net Approved Indications and Usage Guidelines: Bydureon/ Byetta/Tanzeum/Trulicity/Victoza: • Diagnosis of type 2 diabetes AND • Documentation of baseline A1C AND • Failure or clinically significant adverse effects to at least a 3 month trial of metformin (unless contraindicated) REAUTHORIZATION REQUESTS: If inadequate response to GLP-1 receptor agonist ( i.e. <0.5% reduction in A1c) at the end of initial authorization period, either a switch to insulin therapy, addition of insulin(s) to Victoza or a referral to an endocrinologist will be required. Reauthorization requests require documentation of continued metformin therapy (unless contraindicated). Symlin: • Diagnosis of Diabetes Mellitus Type 1 or 2 AND • Failure to achieve desired blood glucose level despite 3 months of three or more daily mealtime insulin (e.g. Humalog ®, Humulin ® R) injections or use of an insulin pump Confidential & Proprietary Page 1 Draft Prepared: 06.17.05 JP Approved by Health Net Pharmacy & Therapeutics Committee: 11.16.05, 04.06, 5.21.08, 11.19.08, 11.19.09, 8.25.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 04.07.06. -

Inpatient Care | Lantus (Insulin Glargine Injection) 100 Units/Ml
For noncritically ill hospitalized patients with diabetes Lantus® as part of a basal-prandial dosing regimen ARA basal-prandialBBIT 2 BASAL-PRA dosing NDoptionIAL forDOS nonintensiveING care inpatients with type 2 diabetes from the RABBIT 2 Study1,a A basal-prandial dosing option for inpatients with type 2 diabetes from the RABBIT 2 Study 31 Calculate total daily dose based Total daily dose on BG and weight at the time of • For BG 140-200 mg/dL, use 0.4 Units/kg admission • For BG 201-400 mg/dL, use 0.5 Units/kg Dose administration Divide the calculated dose into basal and prandial components • Administer 50% of daily dose as basal insulin • Administer the other 50% as rapid-acting prandial 50:50 insulin divided into 3 mealtime injections basal prandial Dose administration Monitor BG, add supplemental • If fasting or mean BG during the day >140 mg/dL, increase basal insulin dose by 20% rapid-acting insulin, and adjust doses as needed • If fasting and premeal BG >140 mg/dL, add supplemental rapid-acting insulin • If BG <70 mg/dL, reduce basal insulin dose by 20% • Hold prandial insulin doses in patients not eating RABBIT 2 was a multicenter, prospective, open-label, randomized study (N=130) to compare the efficacy of a basal-prandial regimen of insulin glargine + insulin glulisine with SSI monotherapy (regular human insulin) in insulin-naive nonsurgical patients aged 18 to 80 years with type 2 diabetes. Patients in the basal-prandial group received glargine once daily and glulisine before meals. SSI was given 4 times per Aday basal-prandialfor BG >140 mg/dL. -

Glucagon-Like Peptide-1 and Its Class BG Protein–Coupled Receptors
1521-0081/68/4/954–1013$25.00 http://dx.doi.org/10.1124/pr.115.011395 PHARMACOLOGICAL REVIEWS Pharmacol Rev 68:954–1013, October 2016 Copyright © 2016 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: RICHARD DEQUAN YE Glucagon-Like Peptide-1 and Its Class B G Protein–Coupled Receptors: A Long March to Therapeutic Successes Chris de Graaf, Dan Donnelly, Denise Wootten, Jesper Lau, Patrick M. Sexton, Laurence J. Miller, Jung-Mo Ahn, Jiayu Liao, Madeleine M. Fletcher, Dehua Yang, Alastair J. H. Brown, Caihong Zhou, Jiejie Deng, and Ming-Wei Wang Division of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands (C.d.G.); School of Biomedical Sciences, University of Leeds, Leeds, United Kingdom (D.D.); Drug Discovery Biology Theme and Department of Pharmacology, Monash Institute of Pharmaceutical Sciences, Parkville, Victoria, Australia (D.W., P.M.S., M.M.F.); Protein and Peptide Chemistry, Global Research, Novo Nordisk A/S, Måløv, Denmark (J.La.); Department of Molecular Pharmacology and Experimental Therapeutics, Mayo Clinic, Scottsdale, Arizona (L.J.M.); Department of Chemistry and Biochemistry, University of Texas at Dallas, Richardson, Texas (J.-M.A.); Department of Bioengineering, Bourns College of Engineering, University of California at Riverside, Riverside, California (J.Li.); National Center for Drug Screening and CAS Key Laboratory of Receptor Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, China (D.Y., C.Z., J.D., M.-W.W.); Heptares Therapeutics, BioPark, Welwyn Garden City, United Kingdom (A.J.H.B.); and School of Pharmacy, Fudan University, Zhangjiang High-Tech Park, Shanghai, China (M.-W.W.) Downloaded from Abstract. -

Lixisenatide Injection, Subcutaneous
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 New Drug Evaluation: lixisenatide injection, subcutaneous Date of Review: January 2017 End Date of Literature Search: Generic Name: lixisenatide Brand Name (Manufacturer): Adlyxin (Sanofi-Aventis) PDL Class: GLP-1 receptor agonists AMCP Dossier Received: Yes Current Status of PDL Class: See Appendix 1. Research Questions: Is there evidence that lixisenatide improves outcomes versus other GLP-1 receptor agonists in patients with type 2 diabetes mellitus (T2DM), including hemoglobin A1c (A1C) reduction, microvascular and macrovascular outcomes and mortality? Is there evidence that lixisenatide is safer than other GLP-1 receptor agonists in patients with T2DM? Are there subpopulations of patients with T2DM for which lixisenatide may be more effective or associated with less harm? Conclusions: Lixisenatide approval was based on 11 phase 3 clinical trials.1- 11 Eight trials were placebo-controlled and 3 were active treatment comparisons to either sitagliptin, exenatide or insulin glulisine. All trials were designed and funded by the manufacture Sanofi-Aventis. Limitations to the data include short trial durations (12-26 weeks for most) and insufficient evidence for improvement in any health outcomes. The studies are most applicable to patients with moderately uncontrolled T2DM (HbA1c around 8%) with few comorbidities. There is insufficient evidence to determine if lixisenatide has any effect on microvascular outcomes. One study provides moderate strength evidence that lixisenatide is not associated with increased risk for macrovascular outcomes compared to placebo. -

GLP-1) Agonists Annual Review Date: 12/17/2020
Policy: Glucagon-Like Peptide-1 (GLP-1) Agonists Annual Review Date: 12/17/2020 Impacted Last Revised Date: Drugs: • Tanzeum (albiglutide) • Victoza (liraglutide) 12/17/2020 • Adlyxin (lixisenatide) OVERVIEW Bydureon, Byetta, Tanzeum, Trulicity, Victoza, Adlyxin, Rybelsus and Ozempic are glucagon-like peptide-1(GLP-1) agonists indicated in adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes. Incretins, such as GLP-1, enhance glucose-dependent insulin secretion and exhibit other antihyperglycemic actions following their release into circulation from the gut. The GLP-1 agonists enhance glucose-dependent insulin secretion by the pancreatic beta-cell, suppress inappropriately elevated glucagon secretion, and slow gastric emptying. All of the GLP-1 agonists, except Rybelsus, are administered by subcutaneous (SC) injection. Bydureon is an extended release formulation of Byetta allowing for once-weekly (QW) administration. Unlike Byetta, Trulicity and Victoza, Bydureon and Tanzeum require reconstitution. Byetta is a twice-daily (BID) injection, Trulicity, Ozempic, and Tanzeum are once-weekly (QW) injections, and Victoza and Adlyxin are a once-daily (QD) injection. Rybelsus is a once daily oral tablet. The prescribing information for Bydureon and Byetta note that neither of these agents are recommended in patients with severe renal impairment (creatinine clearance [CrCl] < 30 mL/min) or end-stage renal disease (ESRD) and should be used with caution in patients with renal transplantation. Victoza’s prescribing information notes that it has not been found to be directly nephrotoxic in animal studies or clinical trials. Caution is recommended when initiating or escalating doses of Victoza in patients with renal impairment.