Maikawa STM 2021.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular Basis of Blood Glucose Regulation Asma Ahmed and Noman Khalique
Chapter Molecular Basis of Blood Glucose Regulation Asma Ahmed and Noman Khalique Abstract Blood glucose level is regulated by multiple pancreatic hormones, which regulate it by different pathways in normal and abnormal conditions by expressing or suppressing multiple genes or molecular or cellular targets. Multiple synthetic drugs and therapies are used to cure glucose regulatory problems, while many of them are used to cure other health issues, which arise due to disturbance in blood glucose regulations. Many new approaches are used for the development of phytochemical- based drugs to cure blood glucose regulation problems, and many of the compounds have been isolated and identified to cure insulin resistance or regulate beta cell function or glucose absorption in the guts or GLP-1 homoeostasis or two/more pathways (e.g., either cure hyperglycemia or raise insulin resistance or cure pan- creatic beta cell regeneration or augmentation of GLP-1, production of islet cell, production and increased insulin receptor signaling and insulin secretion or decreased insulin tolerance or gluconeogenesis and insulin-mimetic action or pro- duction of α-glucosidase and α-amylase inhibitor or conserve islet mass or activate protein kinase A (PKA) and extracellular signal regulated kinases (ERK) or activate AMPK and reduce insulin sensitivity or suppress α-glucosidase activity and activate AMPK and downstream molecules or prevents cell death of pancreatic β-cell and activates SIRT1 or lower blood glucose due to their insulin-like chemical structures or decrease lipid peroxidation. Keywords: genes, molecular and cellular targets, hormones, pathways 1. Introduction Blood glucose is regulated by the pancreatic hormones alone or in combination with other endocrine glands and all this is controlled by one or more gene or cellular or molecular targets. -

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

(Pram) and Insulin A21G Improves Post-Prandial Glucose Vs Novolog
ADO09, A Co-Formulation Of Pramlintide (Pram) and Insulin A21G improves Post-Prandial Glucose Vs Novolog® in Type 1 Diabetes (T1DM) G.Meiffren¹, G.Andersen², R.Eloy¹, C.Seroussi¹, C.Mégret¹, S.Famulla², Y.-P Chan¹, M.Gaudier¹, O.Soula¹, J.H. DeVries²,T.Heise² (1 Adocia, Lyon, France ; 2 Profil, Neuss, Germany) Introduction & Background Overall safety Outpatient period results - CGM metrics o ADO09 (M1Pram) is a co-formulation of pramlintide and insulin A21G o Both treatments were well tolerated without any treatment-related serious adverse events o Most of the CGM metrics (TiR [70-180], TiR [80-140], mean blood glucose per day), were significantly improved developed to leverage the beneficial effects of pramlintide on post-prandial (Table 2). As expected M1Pram had numerically more, mostly gastrointestinal adverse events with M1Pram (Table 4). Postprandial and mean 24-hour glucose profiles were improved with M1Pram (Fig. 3) glucose without additional injections than insulin aspart Table 4: CGM metrics, all days. Significant differences are marked in bold Objective and design o No severe hypoglycemia were seen, slightly more hypoglycemic events occurred with M1Pram Ratio of LSMean* o To compare the effect of M1Pram and insulin aspart (Novolog®, Novo than with aspart (Table 3) Difference Parameter Treatment LS Mean M1Pram / Aspart P-value Nordisk) on post-prandial glucose control, glycemic control assessed by Table 2: Incidence of adverse events throughout the trial (M1Pram-Aspart) (95% CI) CGM and safety/tolerability M1Pram Aspart M1Pram -

Inhaled Insulin: the Solution for Suboptimal Diabetes Control?
I EDITORIALS Inhaled insulin: the solution for suboptimal diabetes control? Stephanie A Amiel Stephanie A Amiel For nearly a century, we have been using insulin to action comparable to human soluble (regular) BSc MD FRCP, treat diabetes. Until recently, that insulin has been insulin rather than fast-acting analogues.10 In trials, RD Lawrence given by injection. In 2006, the first inhaled insulin, Exubera® is only ‘non-inferior’ to conventional (not Professor of Diabetic Exubera®, was licenced for use in Europe. The man- analogue) insulins, the latter not always used in Medicine, King’s ufacturers hoped for a warm welcome – the end of equivalent basal-bolus regimens11–14 and in type 2, College London School of Medicine injections and the dawn of a new era of enthusiastic slightly more effective than adding a second oral insulin takers with perfect diabetic control. The agent in very poorly controlled disease.15,16 It has not Clin Med National Institute for Health and Clinical Excellence been tested against fully flexible analogue regimens. 2007;7:430–2 (NICE) was more cautious and recommend that It is clear that inhaled insulin’s sole advantage over inhaled insulin only be used in the presence of diag- injected insulin is its route of delivery. nosed needle phobia (or severe intractable problems Exubera® has low bioavailability, minor and prob- with injection sites) and should be supervised by dia- ably reversible effects on lung function17 and a nat- betes specialists.1 True needle phobia is rare and ural lack of long-term safety data. Active smoking treatable by standard psychological techniques.2,3 On contraindicates its use because of increased bioavail- the NICE criteria, the market for inhaled insulin may abilty of inhaled insulin,18,19 while absorption may be small indeed. -
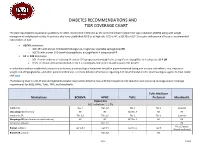
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -

The Un-Design and Design of Insulin: Structural Evolution
THE UN-DESIGN AND DESIGN OF INSULIN: STRUCTURAL EVOLUTION WITH APPLICATION TO THERAPEUTIC DESIGN By NISCHAY K. REGE Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Biochemistry Dissertation Advisor: Dr. Michael A. Weiss CASE WESTERN RESERVE UNIVERSITY August, 2018 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of Nischay K. Rege candidate for the degree of Doctor of Philosophy*. Committee Chair Paul Carey Committee Member Michael Weiss Committee Member Faramarz Ismail-Beigi Committee Member George Dubyak Date of Defense: June 26th, 2018 *We also certify that written approval has been obtained for any proprietary material contained therein. Dedication This thesis is dedicated to my mother, Dipti, whose constant love and faith have never failed, to my father, Kiran, who taught me of the virtue of curiosity, and to my wife, Shipra, whose kindness and companionship have given me enough strength for eight lifetimes. i Table of Contents Dedication ..................................................................................................................................... i Table of Contents ......................................................................................................................... ii List of Tables ............................................................................................................................... v List of Figures ........................................................................................................................... -

Tresiba-Product-Monograph.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION TRESIBA® insulin degludec injection TRESIBA® FlexTouch® 100 U/mL, Solution for injection in a pre-filled pen TRESIBA® FlexTouch® 200 U/mL, Solution for injection in a pre-filled pen Subcutaneous Antidiabetic Agent Long-Acting Basal Insulin Analogue ATC Code: A10AE06 Novo Nordisk Canada Inc. Date of Initial Authorization: AUG 25, 2017 101-2476 Argentia Road Date of Revision: Mississauga, Ontario JUL 23, 2021 Canada L5N 6M1 Submission Control Number: 250276 Product Monograph Master Template Template Date: September 2020 TRESIBA® (insulin degludec injection) Page 1 of 2 RECENT MAJOR LABEL CHANGES 7 Warnings and Precautions 03/2021 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS ..............................................................................................................2 1 INDICATIONS ..................................................................................................................4 1.1 Pediatrics ................................................................................................................4 1.2 Geriatrics ................................................................................................................4 2 CONTRAINDICATIONS ..................................................................................................4 3 SERIOUS WARNINGS AND PRECAUTIONS BOX .......................................................4 4 DOSAGE AND ADMINISTRATION -

Prior Authorization Protocol NATL
Prior Authorization Protocol BYDUREON™ (exenatide extended-release for injectable suspension), BYETTA TM (exenatide), SYMLIN PEN (pramlintide acetate), TANZEUM TM (albiglutide) TRULICITY™ (dulaglutide), VICTOZA ® (liraglutide) NATL Coverage of drugs is first determined by the member`s pharmacy or medical benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: • Bydureon, Byetta, Tanzeum, Trulicity, Victoza: An adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus • Symlin: Adjunctive treatment in patients with type 1 or type 2 diabetes who use mealtime insulin therapy and who have failed to achieve desired glucose control despite optimal insulin therapy. II. Health Net Approved Indications and Usage Guidelines: Bydureon/ Byetta/Tanzeum/Trulicity/Victoza: • Diagnosis of type 2 diabetes AND • Documentation of baseline A1C AND • Failure or clinically significant adverse effects to at least a 3 month trial of metformin (unless contraindicated) REAUTHORIZATION REQUESTS: If inadequate response to GLP-1 receptor agonist ( i.e. <0.5% reduction in A1c) at the end of initial authorization period, either a switch to insulin therapy, addition of insulin(s) to Victoza or a referral to an endocrinologist will be required. Reauthorization requests require documentation of continued metformin therapy (unless contraindicated). Symlin: • Diagnosis of Diabetes Mellitus Type 1 or 2 AND • Failure to achieve desired blood glucose level despite 3 months of three or more daily mealtime insulin (e.g. Humalog ®, Humulin ® R) injections or use of an insulin pump Confidential & Proprietary Page 1 Draft Prepared: 06.17.05 JP Approved by Health Net Pharmacy & Therapeutics Committee: 11.16.05, 04.06, 5.21.08, 11.19.08, 11.19.09, 8.25.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 04.07.06. -

Ep 2330124 A2
(19) TZZ ¥¥Z_ T (11) EP 2 330 124 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.06.2011 Bulletin 2011/23 C07K 14/575 (2006.01) (21) Application number: 10012149.0 (22) Date of filing: 11.08.2006 (84) Designated Contracting States: • Lewis, Diana AT BE BG CH CY CZ DE DK EE ES FI FR GB GR San Diego, CA 92121 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Soares, Christopher J. SK TR San Diego, CA 92121 (US) • Ghosh, Soumitra S. (30) Priority: 11.08.2005 US 201664 San Diego, CA 92121 (US) 17.08.2005 US 206903 • D’Souza, Lawrence 12.12.2005 US 301744 San Diego, CA 92121 (US) • Parkes, David G. (62) Document number(s) of the earlier application(s) in San Diego, CA 92121 (US) accordance with Art. 76 EPC: • Mack, Christine M. 06801467.9 / 1 922 336 San Diego, CA 92121 (US) • Forood, Behrouz Bruce (71) Applicant: Amylin Pharmaceuticals Inc. San Diego, CA 92121 (US) San Diego, CA 92121 (US) (74) Representative: Gowshall, Jonathan Vallance et al (72) Inventors: Forrester & Boehmert • Levy, Odile Esther Pettenkoferstrasse 20-22 San Diego, CA 92121 (US) 80336 München (DE) • Hanley, Michael R. San Diego, CA 92121 (US) Remarks: • Jodka, Carolyn M. This application was filed on 30-09-2010 as a San Diego, CA 92121 (US) divisional application to the application mentioned under INID code 62. (54) Hybrid polypeptides with selectable properties (57) The present invention relates generally to novel, tions and disorders include, but are not limited to, hyper- selectable hybrid polypeptides useful as agents for the tension, dyslipidemia, cardiovascular disease, eating treatment and prevention of metabolic diseases and dis- disorders, insulin-resistance, obesity, and diabetes mel- orders which can be alleviated by control plasma glucose litus of any kind, including type 1, type 2, and gestational levels, insulin levels, and/or insulin secretion, such as diabetes. -

INSULIN-CONTAINING PRODUCTS from NOVO NORDISK Storage, and Savings Information
Please see the following pages for Tresiba®, ® ® Xultophy 100/3.6, and Fiasp Dosing, 1 INSULIN-CONTAINING PRODUCTS FROM NOVO NORDISK Storage, and Savings Information. BASAL 100 units/mL; total of 200 units/mL; total of 100 units/mL; total of 300 units/pen; 5-pen pack1 600 units/pen; 3-pen pack1 1000 units/vial; 1 vial/pack1 NDC: 0169-2660-15 NDC: 0169-2550-13 NDC: 0169-2662-11 100 units/mL insulin degludec and 3.6 mg/mL liraglutide; total of 300 units insulin degludec and 10.8 mg liraglutide; 5-pen pack2 NDC: 0169-2911-15 BASAL/GLP-1 RA Approved for use in pumps3 Refer to the insulin infusion pump user manual to see if Fiasp® can be used. Use in accordance with the insulin pump’s Instructions for Use. 100 units/mL; total of 300 units; 100 units/mL; total of 100 units/mL; total of PRANDIAL 5-pen pack3 300 units/pen; 5-cartridge pack3 1000 units/vial; 1 vial/pack3 NDC: 0169-3204-15 NDC: 0169-3205-15 NDC: 0169-3201-11 GLP-1 RA=glucagon-like peptide-1 receptor agonist. Tresiba® Indications and Usage Xultophy® 100/3.6 Indications and Xultophy® 100/3.6 Important Safety Fiasp® Indications and Usage Tresiba® (insulin degludec injection) is indicated to Limitations of Use Information Fiasp® (insulin aspart injection) 100 U/mL is a improve glycemic control in patients 1 year of age and Xultophy® 100/3.6 (insulin degludec and liraglutide injection) rapid-acting insulin analog indicated to improve older with diabetes mellitus. WARNING: RISK OF THYROID C-CELL TUMORS 100 units/mL and 3.6 mg/mL is a combination of insulin ® glycemic control in adult and pediatric patients with degludec and liraglutide and is indicated as an adjunct to diet • Liraglutide, one of the components of Xultophy 100/3.6, causes dose-dependent and treatment-duration-dependent thyroid diabetes mellitus. -

The Leading Source of Diabetes Business News It's Complicated
The Leading Source of Diabetes Business News It’s Complicated January/February 2011 • No. 105 The diabetes business used to be fairly straightforward. It’s a lot more complicated now, but that’s not a bad thing. Take insulin. After it was commercialized in the early 1920s, the goal was clear: sell more insulin. But look at today’s three major insulin makers: Eli Lilly, sanofi-aventis, and Novo Nordisk. For all three, to be sure, insulin is still preeminent. The diabetes divisions of Novo Nordisk and Lilly draw most of their revenue from human insulin and rapid-acting analogs, while sanofi-aventis’ blockbuster basal analog Lantus, as well as its mealtime insulins, continue to drive the bottom line. But all three companies have also developed (or are developing) GLP-1 analogs, Lilly has invested in oral drugs for type 2 diabetes (most recently through a major partnership with Boehringer Ingelheim), and the companies are also developing new therapeutic approaches for different stages of disease progression. The evolution of the insulin makers reflects broader industry trends. As our understanding of diabetes has expanded – and we dig deeper into the molecular complexities of the disease – it’s clear that single- focus large companies can no longer prosper. Ours is an era of individualized treatment that mixes and matches different drugs and technologies that try to meet the unique needs of every person with diabetes. Toward that end, companies are forming partnerships to find complementary therapies and development efforts that will create -

Various Emerging Trends in Insulin Drug Delivery Systems
British Journal of Pharmaceutical Research 5(5): 294-308, 2015, Article no.BJPR.2015.029 ISSN: 2231-2919 SCIENCEDOMAIN international www.sciencedomain.org Various Emerging Trends in Insulin Drug Delivery Systems Yasmeen1, T. Mamatha1*, Md. Zubair1, Sana Begum1 and Tayyaba Muneera1 1Department of Pharmaceutics, Sultan-ul-Uloom College of Pharmacy, affiliated to Jawaharlal Nehru Technological University Hyderabad, Road No.3, Banjara hills, Hyderabad 500 034, Telangana, India. Authors’ contributions This work was carried out in collaboration between all authors. Author TM designed the study, Authors Y and SB wrote the protocol, and wrote the first draft of the manuscript. Authors Md. Z and TM managed the literature searches. All authors read and approved the final manuscript. Article Information DOI:10.9734/BJPR/2015/12528 Editor(s): (1) Rafik Karaman, Bioorganic Chemistry, College of Pharmacy, Al-Quds University, USA. (2) Alyautdin Renad N, The Department of Pharmacology, I. M. Sechenov MSMU, Russia. Reviewers: (1) Anonymous, Italy. (2) Anonymous, Spain. (3) Anonymous, Norway. (4) Wei Wu, School of Pharmacy, Fudan University, China. (5) Anonymous, Malaysia. (6) Anastasia Thanopoulou, Diabetes Centre and Department of Internal Medicine, National University of Athens, Hippokration General Hospital, Athens, Greece. Complete Peer review History: http://www.sciencedomain.org/review-history.php?iid=883&id=14&aid=7718 Received 4th July 2014 th Review Article Accepted 28 November 2014 Published 9th January 2015 ABSTRACT Lowering of blood glucose level in patients can be achieved by insulin therapy as it plays a key role in the control of hyperglycaemia for type 1 diabetes. Insulin delivery systems that are currently available include syringes, infusion pumps, jet injectors and pens.