Symlin) Reference Number: CP.PMN.129 Effective Date: 06.01.18 Last Review Date: 02.21 Coding Implications Line of Business: Commercial, HIM, Medicaid Revision Log
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

(Pram) and Insulin A21G Improves Post-Prandial Glucose Vs Novolog
ADO09, A Co-Formulation Of Pramlintide (Pram) and Insulin A21G improves Post-Prandial Glucose Vs Novolog® in Type 1 Diabetes (T1DM) G.Meiffren¹, G.Andersen², R.Eloy¹, C.Seroussi¹, C.Mégret¹, S.Famulla², Y.-P Chan¹, M.Gaudier¹, O.Soula¹, J.H. DeVries²,T.Heise² (1 Adocia, Lyon, France ; 2 Profil, Neuss, Germany) Introduction & Background Overall safety Outpatient period results - CGM metrics o ADO09 (M1Pram) is a co-formulation of pramlintide and insulin A21G o Both treatments were well tolerated without any treatment-related serious adverse events o Most of the CGM metrics (TiR [70-180], TiR [80-140], mean blood glucose per day), were significantly improved developed to leverage the beneficial effects of pramlintide on post-prandial (Table 2). As expected M1Pram had numerically more, mostly gastrointestinal adverse events with M1Pram (Table 4). Postprandial and mean 24-hour glucose profiles were improved with M1Pram (Fig. 3) glucose without additional injections than insulin aspart Table 4: CGM metrics, all days. Significant differences are marked in bold Objective and design o No severe hypoglycemia were seen, slightly more hypoglycemic events occurred with M1Pram Ratio of LSMean* o To compare the effect of M1Pram and insulin aspart (Novolog®, Novo than with aspart (Table 3) Difference Parameter Treatment LS Mean M1Pram / Aspart P-value Nordisk) on post-prandial glucose control, glycemic control assessed by Table 2: Incidence of adverse events throughout the trial (M1Pram-Aspart) (95% CI) CGM and safety/tolerability M1Pram Aspart M1Pram -
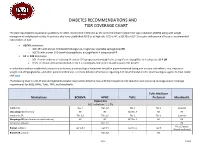
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -

Tresiba-Product-Monograph.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION TRESIBA® insulin degludec injection TRESIBA® FlexTouch® 100 U/mL, Solution for injection in a pre-filled pen TRESIBA® FlexTouch® 200 U/mL, Solution for injection in a pre-filled pen Subcutaneous Antidiabetic Agent Long-Acting Basal Insulin Analogue ATC Code: A10AE06 Novo Nordisk Canada Inc. Date of Initial Authorization: AUG 25, 2017 101-2476 Argentia Road Date of Revision: Mississauga, Ontario JUL 23, 2021 Canada L5N 6M1 Submission Control Number: 250276 Product Monograph Master Template Template Date: September 2020 TRESIBA® (insulin degludec injection) Page 1 of 2 RECENT MAJOR LABEL CHANGES 7 Warnings and Precautions 03/2021 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS ..............................................................................................................2 1 INDICATIONS ..................................................................................................................4 1.1 Pediatrics ................................................................................................................4 1.2 Geriatrics ................................................................................................................4 2 CONTRAINDICATIONS ..................................................................................................4 3 SERIOUS WARNINGS AND PRECAUTIONS BOX .......................................................4 4 DOSAGE AND ADMINISTRATION -

Prior Authorization Protocol NATL
Prior Authorization Protocol BYDUREON™ (exenatide extended-release for injectable suspension), BYETTA TM (exenatide), SYMLIN PEN (pramlintide acetate), TANZEUM TM (albiglutide) TRULICITY™ (dulaglutide), VICTOZA ® (liraglutide) NATL Coverage of drugs is first determined by the member`s pharmacy or medical benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: • Bydureon, Byetta, Tanzeum, Trulicity, Victoza: An adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus • Symlin: Adjunctive treatment in patients with type 1 or type 2 diabetes who use mealtime insulin therapy and who have failed to achieve desired glucose control despite optimal insulin therapy. II. Health Net Approved Indications and Usage Guidelines: Bydureon/ Byetta/Tanzeum/Trulicity/Victoza: • Diagnosis of type 2 diabetes AND • Documentation of baseline A1C AND • Failure or clinically significant adverse effects to at least a 3 month trial of metformin (unless contraindicated) REAUTHORIZATION REQUESTS: If inadequate response to GLP-1 receptor agonist ( i.e. <0.5% reduction in A1c) at the end of initial authorization period, either a switch to insulin therapy, addition of insulin(s) to Victoza or a referral to an endocrinologist will be required. Reauthorization requests require documentation of continued metformin therapy (unless contraindicated). Symlin: • Diagnosis of Diabetes Mellitus Type 1 or 2 AND • Failure to achieve desired blood glucose level despite 3 months of three or more daily mealtime insulin (e.g. Humalog ®, Humulin ® R) injections or use of an insulin pump Confidential & Proprietary Page 1 Draft Prepared: 06.17.05 JP Approved by Health Net Pharmacy & Therapeutics Committee: 11.16.05, 04.06, 5.21.08, 11.19.08, 11.19.09, 8.25.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 04.07.06. -

Ep 2330124 A2
(19) TZZ ¥¥Z_ T (11) EP 2 330 124 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.06.2011 Bulletin 2011/23 C07K 14/575 (2006.01) (21) Application number: 10012149.0 (22) Date of filing: 11.08.2006 (84) Designated Contracting States: • Lewis, Diana AT BE BG CH CY CZ DE DK EE ES FI FR GB GR San Diego, CA 92121 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Soares, Christopher J. SK TR San Diego, CA 92121 (US) • Ghosh, Soumitra S. (30) Priority: 11.08.2005 US 201664 San Diego, CA 92121 (US) 17.08.2005 US 206903 • D’Souza, Lawrence 12.12.2005 US 301744 San Diego, CA 92121 (US) • Parkes, David G. (62) Document number(s) of the earlier application(s) in San Diego, CA 92121 (US) accordance with Art. 76 EPC: • Mack, Christine M. 06801467.9 / 1 922 336 San Diego, CA 92121 (US) • Forood, Behrouz Bruce (71) Applicant: Amylin Pharmaceuticals Inc. San Diego, CA 92121 (US) San Diego, CA 92121 (US) (74) Representative: Gowshall, Jonathan Vallance et al (72) Inventors: Forrester & Boehmert • Levy, Odile Esther Pettenkoferstrasse 20-22 San Diego, CA 92121 (US) 80336 München (DE) • Hanley, Michael R. San Diego, CA 92121 (US) Remarks: • Jodka, Carolyn M. This application was filed on 30-09-2010 as a San Diego, CA 92121 (US) divisional application to the application mentioned under INID code 62. (54) Hybrid polypeptides with selectable properties (57) The present invention relates generally to novel, tions and disorders include, but are not limited to, hyper- selectable hybrid polypeptides useful as agents for the tension, dyslipidemia, cardiovascular disease, eating treatment and prevention of metabolic diseases and dis- disorders, insulin-resistance, obesity, and diabetes mel- orders which can be alleviated by control plasma glucose litus of any kind, including type 1, type 2, and gestational levels, insulin levels, and/or insulin secretion, such as diabetes. -

Maikawa STM 2021.Pdf
SCIENCE TRANSLATIONAL MEDICINE | REVIEW DRUG DEVELOPMENT Copyright © 2021 The Authors, some rights reserved; Engineering biopharmaceutical formulations exclusive licensee American Association to improve diabetes management for the Advancement Caitlin L. Maikawa1, Andrea I. d’Aquino2, Rayhan A. Lal3,4,5, of Science. No claim 4,5 1,2,4,5,6 to original U.S. Bruce A. Buckingham , Eric A. Appel * Government Works Insulin was first isolated almost a century ago, yet commercial formulations of insulin and its analogs for hormone replacement therapy still fall short of appropriately mimicking endogenous glycemic control. Moreover, the controlled delivery of complementary hormones (such as amylin or glucagon) is complicated by instability of the pharmacologic agents and complexity of maintaining multiple infusions. In this review, we highlight the advantages and limitations of recent advances in drug formulation that improve protein stability and pharmacokinetics, prolong drug delivery, or enable alternative dosage forms for the management of diabetes. With controlled delivery, Downloaded from these formulations could improve closed-loop glycemic control. ENGINEERING OPPORTUNITIES TO IMPROVE DIABETES tive treatment with insulin alone is already highly burdensome and MANAGEMENT costly—requiring frequent glucose monitoring, mealtime insulin Over the past century, insulin replacement therapy has been impera- boluses, basal insulin delivery through infusion pumps or long-acting http://stm.sciencemag.org/ tive to saving lives and improving diabetes treatment outcomes. The analogs, and routine carbohydrate counting—and still does not truly administration of exogenous insulin prevents ketoacidosis, which recapitulate the complexities of metabolic control in nondiabetic was once a universally fatal condition. Although insulin has histor- individuals (Fig. 1B) (7). -

INSULIN-CONTAINING PRODUCTS from NOVO NORDISK Storage, and Savings Information
Please see the following pages for Tresiba®, ® ® Xultophy 100/3.6, and Fiasp Dosing, 1 INSULIN-CONTAINING PRODUCTS FROM NOVO NORDISK Storage, and Savings Information. BASAL 100 units/mL; total of 200 units/mL; total of 100 units/mL; total of 300 units/pen; 5-pen pack1 600 units/pen; 3-pen pack1 1000 units/vial; 1 vial/pack1 NDC: 0169-2660-15 NDC: 0169-2550-13 NDC: 0169-2662-11 100 units/mL insulin degludec and 3.6 mg/mL liraglutide; total of 300 units insulin degludec and 10.8 mg liraglutide; 5-pen pack2 NDC: 0169-2911-15 BASAL/GLP-1 RA Approved for use in pumps3 Refer to the insulin infusion pump user manual to see if Fiasp® can be used. Use in accordance with the insulin pump’s Instructions for Use. 100 units/mL; total of 300 units; 100 units/mL; total of 100 units/mL; total of PRANDIAL 5-pen pack3 300 units/pen; 5-cartridge pack3 1000 units/vial; 1 vial/pack3 NDC: 0169-3204-15 NDC: 0169-3205-15 NDC: 0169-3201-11 GLP-1 RA=glucagon-like peptide-1 receptor agonist. Tresiba® Indications and Usage Xultophy® 100/3.6 Indications and Xultophy® 100/3.6 Important Safety Fiasp® Indications and Usage Tresiba® (insulin degludec injection) is indicated to Limitations of Use Information Fiasp® (insulin aspart injection) 100 U/mL is a improve glycemic control in patients 1 year of age and Xultophy® 100/3.6 (insulin degludec and liraglutide injection) rapid-acting insulin analog indicated to improve older with diabetes mellitus. WARNING: RISK OF THYROID C-CELL TUMORS 100 units/mL and 3.6 mg/mL is a combination of insulin ® glycemic control in adult and pediatric patients with degludec and liraglutide and is indicated as an adjunct to diet • Liraglutide, one of the components of Xultophy 100/3.6, causes dose-dependent and treatment-duration-dependent thyroid diabetes mellitus. -

Glycemic Management of Type 2 Diabetes
Glycemic Management of Type 2 Diabetes Gail Nunlee-Bland, M.D. Professor Medicine & Pediatrics Director, Diabetes Treatment Center Howard University 1 Disclosures • None Learning Objectives • Understand the importance of lifestyle therapy in diabetes management • Know the classes of antihyperglycemic agents, mechanism of action, benefits and side effects of these agents • Recognize the importance of individualized treatment goals for diabetic patients AACE Comprehensive Care Plan Disease management from Antihyperglycemic a multidisciplinary team pharmacotherapy Comprehensive Care Plan Comprehensive diabetes Therapeutic lifestyle self-education for the change patient 4 Handelsman YH, et al. Endocr Pract. 2015;21(suppl 1):1-87. Glycemic Management of Type 2 Diabetes THERAPEUTIC LIFESTYLE CHANGE 5 Components of Therapeutic Lifestyle Change • Healthful eating • Sufficient physical activity • Sufficient sleep • Avoidance of tobacco products • Limited alcohol consumption • Stress reduction 6 Handelsman YH, et al. Endocr Pract. 2015;21(suppl 1):1-87. Glycemic Management of Type 2 Diabetes ANTIHYPERGLYCEMIC THERAPY 7 Cardiovascular Outcomes Trials: A Brief History • 2008 FDA guidance mandating assessment of CV safety of all antihyperglycemic agents in RCTs – Designed as noninferiority studies to demonstrate study drug was not associated with more MACE than placebo • Some study designs tested for superiority if noninferiority criteria were met – Primary endpoint: composite of cardiovascular death, nonfatal MI, and nonfatal stroke • Some primary -

RYZODEG® 70/30 (Insulin Degludec and Insulin Aspart Injection) Label
1 HIGHLIGHTS OF PRESCRIBING INFORMATION 39 • Hyper- or hypoglyemia with changes in insulin regimen: Carry out under 2 These highlights do not include all the information needed to use 40 close medical supervision and increase frequency of blood glucose 3 RYZODEG 70/30 safely and effectively. See full prescribing information 41 monitoring (5.2). 4 for RYZODEG 70/30. 42 • Hypoglycemia: May be life-threatening. Increase monitoring with 5 43 changes to: insulin dosage, co-administered glucose lowering ® 6 RYZODEG 70/30 (insulin degludec and insulin aspart injection), for 44 medications, meal pattern, physical activity; and in patients with renal 7 subcutaneous use 45 impairment or hepatic impairment or hypoglycemia unawareness (5.3,5.4, 8 Initial U.S. Approval: [2015] 46 6.1). 47 • Hypoglycemia due to medication errors: Accidental mix-ups between 9 -----------------------INDICATIONS AND USAGE---------------------------- 48 insulin products can occur. Instruct patients to check insulin labels before 10 RYZODEG 70/30 is an insulin analog indicated to improve glycemic control 49 injection. DO NOT transfer RYZODEG 70/30 into a syringe for 11 in adults with diabetes mellitus (1). 50 administration as overdosage and severe hypoglycemia can result (5.4). 12 • 13 Limitations of Use: 51 Hypersensitivity reactions: Severe, life-threatening, generalized allergy, including anaphylaxis, can occur. Discontinue RYZODEG 70/30, monitor 14 Not recommended for treating diabetic ketoacidosis. 52 53 and treat if indicated (5.5). 15 -----------------DOSAGE AND ADMINISTRATION------------------------- 54 • Hypokalemia: May be life-threatening. Monitor potassium levels in 16 • DO NOT dilute or mix RYZODEG 70/30 with any other insulin products 55 patients at risk for hypokalemia and treat if indicated (5.6). -

Randomized Comparison of Pramlintide Or Mealtime Insulin Added to Basal Insulin Treatment for Patients with Type 2 Diabetes
Clinical Care/Education/Nutrition/Psychosocial Research ORIGINAL ARTICLE Randomized Comparison of Pramlintide or Mealtime Insulin Added to Basal Insulin Treatment for Patients With Type 2 Diabetes 1 2 MATTHEW RIDDLE, MD KAREN LUTZ, PHD limit postmeal hyperglycemia. Amylin 2 2 RICHARD PENCEK, PHD KEN WILHELM, MD deficiency accelerates gastric emptying, 2 2 SUPOAT CHARENKAVANICH, PHD LISA PORTER, MD increases glucagon secretion, and alters satiety mechanisms (10,11). Pramlintide, an injectable synthetic OBJECTIVE — To compare the efficacy and safety of adding mealtime pramlintide or rapid- analog of amylin, slows gastric emptying, acting insulin analogs (RAIAs) to basal insulin for patients with inadequately controlled type 2 attenuates postprandial glucagon secre- diabetes. tion, enhances satiety, and reduces food intake (12–14). Pramlintide is approved RESEARCH DESIGN AND METHODS — In a 24-week open-label, multicenter study, as adjunctive treatment for patients with 113 patients were randomly assigned 1:1 to addition of mealtime pramlintide (120 g) or a diabetes who use mealtime insulin with or titrated RAIA to basal insulin and prior oral antihyperglycemic drugs (OADs). At screening, patients were insulin naive or had been receiving Ͻ50 units/day basal insulin for Ͻ6 months. without oral antihyperglycemic drugs The basal insulin dosage was titrated from day 1, seeking fasting plasma glucose (FPG) Ն70– (OADs) and have not achieved desired Ͻ100 mg/dl. Pramlintide and an RAIA were initiated on day 1 and week 4, respectively. The glucose control. Recently, a 16-week, proportion of patients achieving A1C Յ7.0% without weight gain or severe hypoglycemia at double-blind, placebo-controlled study week 24 was the primary end point. -

Semaglutide Tablets (RYBELSUS) Monograph
Oral Semaglutide Monograph Semaglutide Tablets (RYBELSUS) National Drug Monograph January 2020 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. The Product Information or other resources should be consulted for detailed and most current drug information. FDA Approval Information Description/Mechanism of Action Semaglutide is a once daily oral glucagon-like peptide 1 (GLP-1) agonist used in the treatment of type2 diabetes. Semaglutide increases glucose-dependent insulin release, decreases glucagon secretion, and slows gastric emptying. Indication(s) Under Review in This Document • Adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Limitations of use: • Not recommended as first-line therapy for patients inadequately controlled on diet and exercise • Has not been studied in patients with a history of pancreatitis. Consider another antidiabetic therapy. • Not indicated for use in type 1 diabetes mellitus or treatment of diabetic ketoacidosis Dosage Form(s) Under Review 3mg, 7mg, and 14mg tablets supplied in blister packs to protect tablets from moisture Executive Summary Efficacy • Mean reduction in A1C ranged from 0.9% to 1.4% and weight from 2.2kg to 4.4kg across phase 3 clinical trials • In patients with type 2 diabetes and at high cardiovascular (CV) risk, oral semaglutide was found to be noninferior to placebo for the primary composite outcome (risk of CV death, nonfatal MI, nonfatal stroke). (Hazard Ratio 0.79; 95% CI 0.57, 1.11 p<0.001 for noninferiority and p=0.17 for superiority).