(Pram) and Insulin A21G Improves Post-Prandial Glucose Vs Novolog
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

Insulin Aspart Sanofi, If It Is Coloured Or It Has Solid Pieces in It
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Insulin aspart Sanofi 100 units/ml solution for injection in vial Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One ml solution contains 100 units insulin aspart* (equivalent to 3.5 mg). Insulin aspart Sanofi 100 units/ml solution for injection in vial Each vial contains 10 ml equivalent to 1,000 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Each cartridge contains 3 ml equivalent to 300 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen Each pre-filled pen contains 3 ml equivalent to 300 units insulin aspart. Each pre-filled pen delivers 1-80 units in steps of 1 unit. *produced in Escherichia coli by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear, colourless, aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Insulin aspart Sanofi is indicated for the treatment of diabetes mellitus in adults, adolescents and children aged 1 year and above. 4.2 Posology and method of administration Posology The potency of insulin analogues, including insulin aspart, is expressed in units, whereas the potency of human insulin is expressed in international units. -

A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D
Drugs 2005; 65 (3): 325-340 REVIEW ARTICLE 0012-6667/05/0003-0325/$39.95/0 2005 Adis Data Information BV. All rights reserved. A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D. Mooradian Division of Endocrinology, Department of Internal Medicine, Diabetes, and Metabolism, St Louis University School of Medicine, St Louis, Missouri, USA Contents Abstract ....................................................................................325 1. Physiology of Insulin Secretion .............................................................326 2. Conventional Insulin Preparations ..........................................................327 3. Insulin Analogues ........................................................................328 3.1 Rapid-Acting Insulin Analogues .......................................................328 3.1.1 Insulin Lispro ...................................................................328 3.1.2 Insulin Aspart ..................................................................329 3.1.3 Insulin Glulisine .................................................................329 3.1.4 Clinical Utility of Rapid-Acting Insulin Analogues ...................................330 3.2 Premixed Insulins and Insulin Analogues ................................................331 3.3 Basal Insulin Analogues ...............................................................331 3.3.1 Insulin Glargine ................................................................331 -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -

Insulin Aspart (Nvolog): Important Patient Information
What is most important to remember? If you have questions: Strong Internal Medicine • Insulin aspart (Novolog®) is used to lower blood sugar. It is Ask your doctor, nurse or pharmacist for important to use this medicine as more information about insulin aspart directed by your doctor (Novolog®) • Do not start any new medicines, over-the-counter drugs or herbal remedies without talking to your doctor • Tell all doctors, dentists and pharmacists that you are using insulin aspart (Novolog®) • insulin aspart (Novolog®) can cause low blood sugar. Always Strong Internal Medicine keep a source of sugar handy for 601 Elmwood Avenue times when your blood sugar gets Ambulatory Care Facility, 5th Floor too low Rochester, NY 14642 Phone: (585) 275 -7424 Insulin Aspart • Do not use your insulin if it (Novolog®): Visit our website at: becomes cloudy or has particles www.urmc.rochester.edu/medicine/ - Important Patient Information in it general-medicine/patientcare/ • Throw away all opened insulin after 28 days, even if it is not used up What does insulin aspart (Novolog®) do? Are there any interactions with other drugs that I need What are some things that I need to be aware of when to worry about? taking insulin aspart (Novolog®)? • It is used to lower blood sugar in patient with high blood sugar (diabetes) • There are many drug interactions that may increase • Tell your doctor or pharmacist if you have an allergy to How should insulin aspart (Novolog®) be used? your risk of side effects insulin, or any other drugs, foods, or substances • Use this -
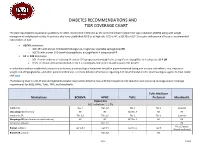
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -

New Diabetes Medications: Where Do They Fit in the Paradigm?
NEW DIABETES MEDICATIONS: WHERE DO THEY FIT IN THE PARADIGM? Nabila Ahmed-Sarwar, Pharm.D., BCPS, CDE Elizabeth Sutton Burke, Pharm.D., BCACP, CDE Wegmans School of Pharmacy November 19 th , 2016 Disclosure Statement No relevant financial relationships to disclose Learning Objectives Upon completion of this educational session, participants will be able to: • Summarize current and new targets for drug action that influence glucose homeostasis • Explain the clinical impact of the new therapeutic agents and determine their place in therapy for the treatment of diabetes mellitus Current Treatment Options Location Medications Effect Secretagogues Increase serum insulin DPP-IV Inhibitors levels Insulin Metformin Decrease Thiazolidinediones gluconeogenesis Increase glucose uptake Alpha-glucosidase Decrease glucose Inhibitors absorption Pramlintide American Diabetes Association-Standards of Care. Diabetes Care 2016 Where do we go from here?? Improved Improved Safety Efficacy Alternative Desirable targets for Administration glucose Regimens homeostasis New Anti-hyperglycemic Agents New Treatment Options Location Medications Effect Increase serum insulin levels Basal Insulins GLP-1 Analogs Decrease glucagon release SGLT-2 Inhibitors Increase urinary glucose excretion Where do we go from here?? Improved Improved Safety Efficacy Alternative Desirable targets for Administration glucose Regimens homeostasis New Anti-hyperglycemic Agents Basal-Rapid Acting Regimen Provides continuous basal coverage Insulin 7 amnoon 7 pm 11 pm 7 am Basal Insulins Generic -

Considering Pramlintide Therapy for Postprandial Blood Glucose Control
Feature Article/Considering Pramlintide Therapy Considering Pramlintide Therapy for Postprandial Blood Glucose Control Belinda P. Childs, ARNP, MN, BC-ADM, CDE; Nicole C. Kesty, PhD; Eric Klein, MD; Richard Rubin, PhD, CDE; and Allison Wick, MSN, ARNP, CDE Abstract Diabetes is a chronic disease affecting Several therapeutic options are cur- > 20 million Americans, and its inci- rently available to address postprandi- dence, especially in the form of type 2 al glucose fluctuations, including diabetes, is increasing. Multiple thera- rapid-acting insulin analogs, incretin peutics are available that address the mimetics, dipeptidyl peptidase IV dysregulation of the multiple hor- inhibitors, α-glucosidase inhibitors, mones responsible for glucose home- meglitinides, and amylinomimetics. ostasis. Despite the various options, This article presents the experiences of tight glycemic control is often elusive. three patients for whom pramlintide, Additionally, the pursuit of tight an amylinomimetic, was identified as glycemic control is generally accom- an appropriate therapeutic option. panied by various clinical challenges, Practical considerations for clinicians, such as hypoglycemia, weight gain, patient lifestyle factors, and percep- and glucose fluctuations, in particular, tions of pramlintide therapy are also postprandial fluctuations. presented. Diabetes, a chronic disease affecting postprandial hyperglycemia without ~ 20.8 million Americans,1 is character- causing concomitant weight gain, ized by chronic hyperglycemia resulting patients now have additional tools to from the body’s inadequate physiologi- manage their diabetes. cal response to glucose. In type 1 dia- betes, secretion of insulin and amylin Glucose Homeostasis into the circulatory system is absolutely Glucose homeostasis is maintained by deficient because of the destruction of a complex multihormonal system that pancreatic β-cells, whereas in type 2 continuously balances the appearance diabetes, secretion of insulin and and disappearance of glucose. -

Glucagon-Like Peptide-1 Receptor Agonists
Clinical Policy: Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists Reference Number: HIM.PA.53 Effective Date: 03.01.18 Last Review Date: 02.21 Line of Business: HIM Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description The following agents contain a synthetic glucagon-like peptide-1 (GLP-1) receptor agonist and require prior authorization: dulaglutide (Trulicity®), exenatide ER (Bydureon®, Bydureon BCise®), exenatide IR (Byetta®), liraglutide (Victoza®), liraglutide/insulin degludec (Xultophy®), lixisenatide (Adlyxin®), lixisenatide/insulin glargine (Soliqua®), and semaglutide (Ozempic®, Rybelsus®). FDA Approved Indication(s) GLP-1 receptor agonists are indicated as adjunct to diet and exercise to improve glycemic control with type 2 diabetes mellitus. Victoza is indicated in patients 10 years of age and older, while the other GLP-1 receptor agonists are indicated in adults. Ozempic, Trulicity and Victoza are also indicated to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes mellitus and: • Established cardiovascular disease (Ozempic, Trulicity, Victoza); • Cardiovascular risk factors (Trulicity only). Limitation(s) of use: • Trulicity, Bydureon, Bydureon BCise, and Xultophy are not recommended as a first-line therapy for patients inadequately controlled on diet and exercise. • Other than Soliqua and Xultophy which contains insulin, GLP-1 receptor agonists are not a substitute for insulin. They should not be used for the treatment of type 1 diabetes or diabetic ketoacidosis. • Other than Trulicity, concurrent use with prandial insulin has not been studied and cannot be recommended. • GLP-1 receptor agonists have not been studied in patients with a history of pancreatitis. -

Tresiba-Product-Monograph.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION TRESIBA® insulin degludec injection TRESIBA® FlexTouch® 100 U/mL, Solution for injection in a pre-filled pen TRESIBA® FlexTouch® 200 U/mL, Solution for injection in a pre-filled pen Subcutaneous Antidiabetic Agent Long-Acting Basal Insulin Analogue ATC Code: A10AE06 Novo Nordisk Canada Inc. Date of Initial Authorization: AUG 25, 2017 101-2476 Argentia Road Date of Revision: Mississauga, Ontario JUL 23, 2021 Canada L5N 6M1 Submission Control Number: 250276 Product Monograph Master Template Template Date: September 2020 TRESIBA® (insulin degludec injection) Page 1 of 2 RECENT MAJOR LABEL CHANGES 7 Warnings and Precautions 03/2021 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS ..............................................................................................................2 1 INDICATIONS ..................................................................................................................4 1.1 Pediatrics ................................................................................................................4 1.2 Geriatrics ................................................................................................................4 2 CONTRAINDICATIONS ..................................................................................................4 3 SERIOUS WARNINGS AND PRECAUTIONS BOX .......................................................4 4 DOSAGE AND ADMINISTRATION -

Study Protocol
CLINICAL TRIAL REPORT ZP4207-17086 (ZEA-DNK-02170) 16.1 TRIAL INFORMATION 16.1.1 PROTOCOL AND PROTOCOL AMENDMENTS This appendix includes Document Date, Version Clinical trial protocol Version 1.0, 08 June 2018 (valid in Slovenia and the USA) Version 3.0, 08 January 2019 (valid in Germany) Section 16.1.1: Protocol and Protocol Amendments Clinical Trial Protocol, final version 1.0 ZP4207-17086 (ZEA-DNK-02170) Clinical Trial Protocol A phase 3, randomized, double-blind, placebo- and active-controlled, parallel-arm trial to assess the efficacy, safety, and pharmacokinetics of dasiglucagon relative to placebo and GlucaGen® when administered as a rescue therapy for severe hypoglycemia in children with T1DM treated with insulin Sponsor code: ZP4207-17086 Synteract: ZEA-DNK-02170 EudraCT number: 2018-000892-33 Coordinating investigator: Prof. Dr. med. Thomas Danne Allgemeine Kinderheilkunde Diabetologie, Endokrinologie, Klinische Forschung Diabeteszentrum für Kinder und Jugendliche AUF DER BULT Kinder- und Jugendkrankenhaus Janusz-Korczak-Allee 12 30173 Hannover Germany Sponsor: Zealand Pharma A/S Smedeland 36 2600 Glostrup, Copenhagen Denmark Version: final version 1.0 Date: 08 June 2018 GCP statement This trial will be performed in compliance with Good Clinical Practice, the Declaration of Helsinki (with amendments) and local legal and regulatory requirements. 08 June 2018 CONFIDENTIAL Page 1/55 Zealand Pharma A/S ClinicalTrial Prolocol, final ve¡sion 1.0 zP 42A7 -1 7 A 86 (ZEA-DN K-02 1 L Slgnature¡ and agreoment wlth protocot Tltle: phase A 3, ¡andomized, double-blind, placebo- and aclivg-controlled, parallel-arm trial to assess the efficac¡ safety, and pharmacoítinetics of dasiglucagon rela¡ve to placebo and GlucaGeno when edministered as a rescue thêrapy for sevãre triposivcemia ¡n children w¡th TlDM treated with insulin we, the undersigned, agroe to conduct lhls trlal according to lhe Trlal protocol. -

Therapeutic Class Overview Therapeuticinsulin and Class Incretin Overview Mime Tic Combination Agents
Therapeutic Class Overview TherapeuticInsulin and Class Incretin Overview Mime tic combination agents INTRODUCTION Diabetes is a tremendous burden on the United States (US) healthcare system. In 2013, diabetes was the 7th leading cause of death in the US. More than 29 million people, or 9.3% of the US population, are estimated to have diagnosed or undiagnosed diabetes (Centers for Disease Control [CDC], 2014). The classification of diabetes includes four clinical classes: 1) type 1 diabetes mellitus (T1DM) which results from beta-cell (β-cell) destruction, usually leading to absolute insulin deficiency, 2) type 2 diabetes mellitus (T2DM) which results from a progressive insulin secretory defect on the background of insulin resistance, 3) other specific types of diabetes due to other causes, eg, genetic defects in β-cell function, genetic defects in insulin action, diseases of the exocrine pancreas (such as cystic fibrosis), and drug- or chemical-induced (such as in the treatment of human immunodeficiency virus [HIV]/acquired immunodeficiency syndrome [AIDS] or after organ transplantation), and 4) gestational diabetes mellitus (GDM) (diabetes diagnosed during pregnancy that is not clearly overt diabetes) (American Diabetes Association [ADA], 2017). The gold standard measure to assess average glycemic exposure in the diagnosis and treatment of T2DM is glycated hemoglobin (HbA1c). HbA1c reflects the average blood glucose (BG) levels over the past 12 weeks including both fasting plasma glucose (FPG) and postprandial plasma glucose (PPG). The exact contributions of PPG and FPG increments to the measure of hyperglycemia and its role in the development of both micro- and macrovascular complications of diabetes remain controversial (Monnier et al, 2011; Monnier et al, 2003).