A Direct Comparison of Insulin Aspart and Insulin Lispro in Patients with Type 1 Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Insulin Aspart Sanofi, If It Is Coloured Or It Has Solid Pieces in It
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Insulin aspart Sanofi 100 units/ml solution for injection in vial Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One ml solution contains 100 units insulin aspart* (equivalent to 3.5 mg). Insulin aspart Sanofi 100 units/ml solution for injection in vial Each vial contains 10 ml equivalent to 1,000 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Each cartridge contains 3 ml equivalent to 300 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen Each pre-filled pen contains 3 ml equivalent to 300 units insulin aspart. Each pre-filled pen delivers 1-80 units in steps of 1 unit. *produced in Escherichia coli by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear, colourless, aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Insulin aspart Sanofi is indicated for the treatment of diabetes mellitus in adults, adolescents and children aged 1 year and above. 4.2 Posology and method of administration Posology The potency of insulin analogues, including insulin aspart, is expressed in units, whereas the potency of human insulin is expressed in international units. -

Combining a Glucagon-Like Peptide-1 Receptor Agonist with Basal Insulin: the Why and How
Combining a Glucagon-like Peptide-1 Receptor Agonist with Basal Insulin: The Why and How Case Study Mary is a 61 year-old female diagnosed with type 2 diabetes mellitus (T2DM) 8 years ago. She was initially managed with the combination of lifestyle modification and metformin. Since that time she was treated with a sulfonylurea, but it was discontinued due to symptomatic hypoglycemia. She was also treated with pioglitazone, but significant fluid retention led to it discontinuation. A year-and-a- half ago, basal insulin was added to her lifestyle and metformin management. She now administers 52 units (0.62 units/kg) once daily at bedtime. Since starting basal insulin, she has experienced 3 episodes of mild hypoglycemia. Since her diagnosis, Mary’s HbA1c has never been <7.0%; her current HbA1c is 7.9%. Over the past month, her fasting plasma glucose (FPG) has ranged from 103 mg/dL to 136 mg/dL and her postprandial glucose (PPG) from 164 mg/dL to 213 mg/dL. She has gained 2.6 kg since starting basal insulin and her body mass index is now 31 kg/m2. Her blood pressure is 134/82 mmHg. She experiences occasional tingling in her feet. Eye examination reveals grade 1 retinopathy. Current medications are: metformin 1000mg twice daily, basal insulin 52 units once daily at bedtime, and hydrochlorothiazide 25 mg once daily. Her family physician notes that Mary’s FPG is reasonably well-controlled, yet her HbA1c and PPG remain elevated. He is also concerned about her episodes of hypoglycemia and weight gain and the evidence indicating microvascular damage. -

A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D
Drugs 2005; 65 (3): 325-340 REVIEW ARTICLE 0012-6667/05/0003-0325/$39.95/0 2005 Adis Data Information BV. All rights reserved. A Critical Appraisal of the Role of Insulin Analogues in the Management of Diabetes Mellitus Ralph Oiknine, Marla Bernbaum and Arshag D. Mooradian Division of Endocrinology, Department of Internal Medicine, Diabetes, and Metabolism, St Louis University School of Medicine, St Louis, Missouri, USA Contents Abstract ....................................................................................325 1. Physiology of Insulin Secretion .............................................................326 2. Conventional Insulin Preparations ..........................................................327 3. Insulin Analogues ........................................................................328 3.1 Rapid-Acting Insulin Analogues .......................................................328 3.1.1 Insulin Lispro ...................................................................328 3.1.2 Insulin Aspart ..................................................................329 3.1.3 Insulin Glulisine .................................................................329 3.1.4 Clinical Utility of Rapid-Acting Insulin Analogues ...................................330 3.2 Premixed Insulins and Insulin Analogues ................................................331 3.3 Basal Insulin Analogues ...............................................................331 3.3.1 Insulin Glargine ................................................................331 -

Performance of the Insulin-Only Ilet Bionic Pancreas and The
e118 Diabetes Care Volume 44, June 2021 Performance of the Insulin-Only Luz E. Castellanos,1 Courtney A. Balliro,1 Jordan S. Sherwood,1 Rabab Jafri,1 iLet Bionic Pancreas and the Mallory A. Hillard,1 Evelyn Greaux,1 Rajendranath Selagamsetty,2 Hui Zheng,3 Bihormonal iLet Using Firas H. El-Khatib,2 Edward R. Damiano,2,4 and Dasiglucagon in Adults With Type Steven J. Russell1 1 Diabetes in a Home-Use Setting Diabetes Care 2021;44:e118–e120 | https://doi.org/10.2337/dc20-1086 Reductions in blood glucose levels in with insulin lispro (Eli Lilly) or aspart (Table 1). The mean CGM glucose and people with diabetes are often achieved (Novo Nordisk), the bihormonal iLet for time in range (70–180 mg/dL) were 149 at the expense of increased hypoglyce- 7dayswithdasiglucagon(4mg/mL) ±13mg/dLand72±8%,respectively,in mia. A novel approach is to automati- and insulin lispro or aspart, or both, us- the insulin-only period, and 139 ± 11 cally deliver microdose glucagon when ing the same glucose target (110 mg/ mg/dL and 79 ± 9%, respectively, in the automation of insulin delivery alone is dL), in random order. There were no re- bihormonal period. The mean daily car- not sufficient to prevent hypoglycemia. strictions on diet or exercise. The prima- bohydrates consumed to prevent or The approach requires a bihormonal de- ry outcomes were prespecified iLet treat hypoglycemia were 16 ± 13 g and vice and a stable form of glucagon or operational thresholds. The key second- 18 ± 21 g in the insulin-only and bihor- glucagon analog. -

(Pram) and Insulin A21G Improves Post-Prandial Glucose Vs Novolog
ADO09, A Co-Formulation Of Pramlintide (Pram) and Insulin A21G improves Post-Prandial Glucose Vs Novolog® in Type 1 Diabetes (T1DM) G.Meiffren¹, G.Andersen², R.Eloy¹, C.Seroussi¹, C.Mégret¹, S.Famulla², Y.-P Chan¹, M.Gaudier¹, O.Soula¹, J.H. DeVries²,T.Heise² (1 Adocia, Lyon, France ; 2 Profil, Neuss, Germany) Introduction & Background Overall safety Outpatient period results - CGM metrics o ADO09 (M1Pram) is a co-formulation of pramlintide and insulin A21G o Both treatments were well tolerated without any treatment-related serious adverse events o Most of the CGM metrics (TiR [70-180], TiR [80-140], mean blood glucose per day), were significantly improved developed to leverage the beneficial effects of pramlintide on post-prandial (Table 2). As expected M1Pram had numerically more, mostly gastrointestinal adverse events with M1Pram (Table 4). Postprandial and mean 24-hour glucose profiles were improved with M1Pram (Fig. 3) glucose without additional injections than insulin aspart Table 4: CGM metrics, all days. Significant differences are marked in bold Objective and design o No severe hypoglycemia were seen, slightly more hypoglycemic events occurred with M1Pram Ratio of LSMean* o To compare the effect of M1Pram and insulin aspart (Novolog®, Novo than with aspart (Table 3) Difference Parameter Treatment LS Mean M1Pram / Aspart P-value Nordisk) on post-prandial glucose control, glycemic control assessed by Table 2: Incidence of adverse events throughout the trial (M1Pram-Aspart) (95% CI) CGM and safety/tolerability M1Pram Aspart M1Pram -

TRULICITY, INN-Dulaglutide
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Trulicity 0.75 mg solution for injection in pre-filled pen Trulicity 1.5 mg solution for injection in pre-filled pen Trulicity 3 mg solution for injection in pre-filled pen Trulicity 4.5 mg solution for injection in pre-filled pen 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Trulicity 0.75 mg solution for injection in pre-filled pen Each pre-filled pen contains 0.75 mg of dulaglutide* in 0.5 ml solution. Trulicity 1.5 mg solution for injection in pre-filled pen Each pre-filled pen contains 1.5 mg of dulaglutide* in 0.5 ml solution. Trulicity 3 mg solution for injection in pre-filled pen Each pre-filled pen contains 3 mg of dulaglutide* in 0.5 ml solution. Trulicity 4.5 mg solution for injection in pre-filled pen Each pre-filled pen contains 4.5 mg of dulaglutide* in 0.5 ml solution. *produced in CHO cells by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection. Clear, colourless solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Type 2 Diabetes Mellitus Trulicity is indicated for the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise • as monotherapy when metformin is considered inappropriate due to intolerance or contraindications • in addition to other medicinal products for the treatment of diabetes. For study results with respect to combinations, effects on glycaemic control and cardiovascular events, and the populations studied, see sections 4.4, 4.5 and 5.1. -

Soliqua – Criteria
Criteria Based Consultation Prescribing Program CRITERIA FOR DRUG COVERAGE Insulin glargine; lixisenatide (Soliqua) subcutaneous injection Initiation (new start) criteria: Non-formulary lixisenatide/glargine (Soliqua) will be covered on the prescription drug benefit when the following criteria are met: Must meet criteria for both individual agents lixisenatide and insulin glargine. Criteria for lixisenatide: • Diagnosis of Type 2 Diabetes Mellitus • Intolerance to preferred GLP-1 agonists liraglutide (Victoza) AND injectable semaglutide (Ozempic) • No personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) • No personal history of gastroparesis • On maximally tolerated metformin dose (dose appropriate per renal function) or allergy or intolerance* to metformin (includes both metformin IR and XR) • And meets one of the following criteria: o Inadequate glycemic response on both basal and bolus insulin despite high dose requirements (total daily insulin dose of 1.5 units per kilogram of body weight or more OR greater than 200 units) OR o Has experienced recurrent nocturnal hypoglycemia with basal insulin defined as: 3 or more episodes of nocturnal hypoglycemia (BG less than 70 mg/dL) over the preceding 30 days that persists despite basal insulin dose reduction (including decrease in NPH dose and subsequent switch to and dose adjustment of insulin glargine) Criteria for insulin glargine • Use in patients with type 1 diabetes mellitus as basal insulin -OR- • Use in patients with -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -

Insulin Aspart (Nvolog): Important Patient Information
What is most important to remember? If you have questions: Strong Internal Medicine • Insulin aspart (Novolog®) is used to lower blood sugar. It is Ask your doctor, nurse or pharmacist for important to use this medicine as more information about insulin aspart directed by your doctor (Novolog®) • Do not start any new medicines, over-the-counter drugs or herbal remedies without talking to your doctor • Tell all doctors, dentists and pharmacists that you are using insulin aspart (Novolog®) • insulin aspart (Novolog®) can cause low blood sugar. Always Strong Internal Medicine keep a source of sugar handy for 601 Elmwood Avenue times when your blood sugar gets Ambulatory Care Facility, 5th Floor too low Rochester, NY 14642 Phone: (585) 275 -7424 Insulin Aspart • Do not use your insulin if it (Novolog®): Visit our website at: becomes cloudy or has particles www.urmc.rochester.edu/medicine/ - Important Patient Information in it general-medicine/patientcare/ • Throw away all opened insulin after 28 days, even if it is not used up What does insulin aspart (Novolog®) do? Are there any interactions with other drugs that I need What are some things that I need to be aware of when to worry about? taking insulin aspart (Novolog®)? • It is used to lower blood sugar in patient with high blood sugar (diabetes) • There are many drug interactions that may increase • Tell your doctor or pharmacist if you have an allergy to How should insulin aspart (Novolog®) be used? your risk of side effects insulin, or any other drugs, foods, or substances • Use this -

Safety of Insulin Lispro and a Biosimilar Insulin Lispro When
DSTXXX10.1177/1932296817753644Journal of Diabetes Science and TechnologyThrasher et al 753644research-article2018 Original Article Journal of Diabetes Science and Technology 2018, Vol. 12(3) 680 –686 Safety of Insulin Lispro and a Biosimilar © 2018 Diabetes Technology Society Insulin Lispro When Administered Reprints and permissions: sagepub.com/journalsPermissions.nav Through an Insulin Pump DOI:https://doi.org/10.1177/1932296817753644 10.1177/1932296817753644 journals.sagepub.com/home/dst James Thrasher, MD1, Howard Surks, MD2, Irene Nowotny, PhD3, Suzanne Pierre, MSc4, Baerbel Rotthaeuser, PhD3, Karin Wernicke-Panten, MD3, and Satish Garg, MD5 Abstract Background: SAR342434 (U100; SAR-Lis; insulin lispro) is a biosimilar/follow-on to insulin lispro (U100; Ly-Lis). Similar pharmacokinetics/pharmacodynamics between the two products has been demonstrated in a hyperinsulinemic euglycemic clamp study. The current study evaluated the safety of SAR-Lis and Ly-Lis when administered by continuous subcutaneous insulin infusion (CSII; insulin pumps). Methods: This was a randomized, open-label, 2 × 4-week, two-arm crossover study in 27 patients with type 1 diabetes mellitus (NCT02603510). The main outcome was the incidence of infusion set occlusions (ISOs), defined as failure to correct hyperglycemia (plasma glucose ≥≥ 300 mg/dl) by 50 mg/dl within 60 minutes by insulin bolus via the pump. Secondary outcomes included intervals between infusion set changes, treatment-emergent adverse events (TEAEs) including infusion site, hypersensitivity reactions and hypoglycemic events, and safety. Results: The number of patients reporting at least one ISO was small: 6/25 patients on SAR-Lis reported 14 ISOs and 4/27 on Ly-Lis reported nine ISOs. The estimated difference in ISO risk for SAR-Lis versus Ly-Lis was 7.9% (95% CI, –1.90 to 17.73). -
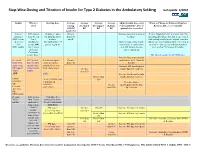
Step-Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting Last Update 5/2010
Step -Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting last update 5/2010 Insulin When to Starting dose Average Average Average Average Adjust Insulin dose every When to Change to Different Regimen start fasting Pre-lunch Pre-supper Bedtime 3 days until BG < 130, or Recheck A1C every 3 months AM BG BG BG BG optimal dose is reached Goal<130 Lantus A1C greater 10 units or up to Greater Increase dose by 2-4 units at If after 3 months if A1c is greater than 7% (glargine) than 8% on 0.2 units/kg SQ at than 130 bedtime. and optimal bedtime dose has been reached OR Levemir 2 or 3 bedtime mg/dL with fasting blood glucose at goal, consider (detemir) antidiabetic (DC sulfonylurea if Optimal long acting (basal) adding a pre-meal bolus insulin at the largest OR agents OR part of regimen) insulin dose keeps bedtime meal of the day, pre-meal bolus insulin at NPH insulin 1 or 2 agents and AM fasting glucose each meal or 70/30 premix insulin. if Serum values consistent. Creatinine greater than 2 DC all oral agents except Metformin. Increase long acting (basal) Pre-meal A1C greater 2-4 units of rapid Greater insulin dose by 2-4 units at bolus with than 7% with acting or regular than 130 bedtime rapid acting optimal long insulin SQ at each Increase AM rapid/regular OR regular acting (basal) meal (base dose) Greater insulin dose by 2-4 units. insulin insulin. than 130 AND with Increase lunch rapid/regular Greater than insulin dose by 2-4 units. -

Considering Pramlintide Therapy for Postprandial Blood Glucose Control
Feature Article/Considering Pramlintide Therapy Considering Pramlintide Therapy for Postprandial Blood Glucose Control Belinda P. Childs, ARNP, MN, BC-ADM, CDE; Nicole C. Kesty, PhD; Eric Klein, MD; Richard Rubin, PhD, CDE; and Allison Wick, MSN, ARNP, CDE Abstract Diabetes is a chronic disease affecting Several therapeutic options are cur- > 20 million Americans, and its inci- rently available to address postprandi- dence, especially in the form of type 2 al glucose fluctuations, including diabetes, is increasing. Multiple thera- rapid-acting insulin analogs, incretin peutics are available that address the mimetics, dipeptidyl peptidase IV dysregulation of the multiple hor- inhibitors, α-glucosidase inhibitors, mones responsible for glucose home- meglitinides, and amylinomimetics. ostasis. Despite the various options, This article presents the experiences of tight glycemic control is often elusive. three patients for whom pramlintide, Additionally, the pursuit of tight an amylinomimetic, was identified as glycemic control is generally accom- an appropriate therapeutic option. panied by various clinical challenges, Practical considerations for clinicians, such as hypoglycemia, weight gain, patient lifestyle factors, and percep- and glucose fluctuations, in particular, tions of pramlintide therapy are also postprandial fluctuations. presented. Diabetes, a chronic disease affecting postprandial hyperglycemia without ~ 20.8 million Americans,1 is character- causing concomitant weight gain, ized by chronic hyperglycemia resulting patients now have additional tools to from the body’s inadequate physiologi- manage their diabetes. cal response to glucose. In type 1 dia- betes, secretion of insulin and amylin Glucose Homeostasis into the circulatory system is absolutely Glucose homeostasis is maintained by deficient because of the destruction of a complex multihormonal system that pancreatic β-cells, whereas in type 2 continuously balances the appearance diabetes, secretion of insulin and and disappearance of glucose.