Airway!Management!
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Report on the Aircraft Accident at Bodø Airport on 4 December 2003 Involving Dornier Do 228-202 Ln-Hta, Operated by Kato Airline As
SL Report 2007/23 REPORT ON THE AIRCRAFT ACCIDENT AT BODØ AIRPORT ON 4 DECEMBER 2003 INVOLVING DORNIER DO 228-202 LN-HTA, OPERATED BY KATO AIRLINE AS This report has been translated into English and published by the AIBN to facilitate access by international readers. As accurate as the translation might be, the original Norwegian text takes precedence as the report of reference. June 2007 Accident Investigation Board Norway P.O. Box 213 N-2001 Lillestrøm Norway Phone:+ 47 63 89 63 00 Fax:+ 47 63 89 63 01 http://www.aibn.no E-mail: [email protected] The Accident Investigation Board has compiled this report for the sole purpose of improving flight safety. The object of any investigation is to identify faults or discrepancies which may endanger flight safety, whether or not these are causal factors in the accident, and to make safety recommendations. It is not the Board’s task to apportion blame or liability. Use of this report for any other purpose than for flight safety should be avoided. Accident Investigation Board Norway Page 2 INDEX NOTIFICATION .................................................................................................................................3 SUMMARY.........................................................................................................................................3 1. FACTUAL INFORMATION..............................................................................................4 1.1 History of the flight..............................................................................................................4 -

Liste-Exploitants-Aeronefs.Pdf
EN EN EN COMMISSION OF THE EUROPEAN COMMUNITIES Brussels, XXX C(2009) XXX final COMMISSION REGULATION (EC) No xxx/2009 of on the list of aircraft operators which performed an aviation activity listed in Annex I to Directive 2003/87/EC on or after 1 January 2006 specifying the administering Member State for each aircraft operator (Text with EEA relevance) EN EN COMMISSION REGULATION (EC) No xxx/2009 of on the list of aircraft operators which performed an aviation activity listed in Annex I to Directive 2003/87/EC on or after 1 January 2006 specifying the administering Member State for each aircraft operator (Text with EEA relevance) THE COMMISSION OF THE EUROPEAN COMMUNITIES, Having regard to the Treaty establishing the European Community, Having regard to Directive 2003/87/EC of the European Parliament and of the Council of 13 October 2003 establishing a system for greenhouse gas emission allowance trading within the Community and amending Council Directive 96/61/EC1, and in particular Article 18a(3)(a) thereof, Whereas: (1) Directive 2003/87/EC, as amended by Directive 2008/101/EC2, includes aviation activities within the scheme for greenhouse gas emission allowance trading within the Community (hereinafter the "Community scheme"). (2) In order to reduce the administrative burden on aircraft operators, Directive 2003/87/EC provides for one Member State to be responsible for each aircraft operator. Article 18a(1) and (2) of Directive 2003/87/EC contains the provisions governing the assignment of each aircraft operator to its administering Member State. The list of aircraft operators and their administering Member States (hereinafter "the list") should ensure that each operator knows which Member State it will be regulated by and that Member States are clear on which operators they should regulate. -

INGENIØRFORLAGET 10 ÅR Åmv
wn-iup '^n A/O7&00O.2?1 INGENIØRFORLAGET 10 ÅR åmv rrr-=s»-T— UDDEHOLM LAND et ressursenes rike. Uddeholms Aktiebolag har langsomt for - a utvikle nye ruslfne stalkvaliteter Skriv eller ring til oss og be om og organisk vokst frem av del varm- som anvendes ved tremstilhng av brosjyren ••Uddeholm om Uddeholnv landske folket og tiihorende landområde kunstgjodsel Konsernet sysselsetter ca 12 000 Med egne gruver, skoger og kratt personer og disponerer over ca 4 5 mill stasjoner star vi sp'vsagt sterkere enn ÜODEHOLftti dekar jord og skog saml moderne mange andre i produksjonen av produksjonsenheter Tilsammen spesialstål, kj f?m i ka li er eller krnttpapir UDDEHOLM STAL A/S forvalter vi en mangehundreang arv - badp i dag og i fremtiden Stalfiæra 1, Postboks 85 Kaldbakken konsernet ble grunnlagi i 5668 Oslo 9 Vi seiger mer verktoystal til industrien Var innsats hat virket som en Telefon (02) 256510 - Telex 18473 enn noen andre, og lager blader lor stimulans i ulvikhngen av nye kriteriet vevstoler tre ganger lynnere enn for kvalitet - som bfant annef tnneltærer *Vaei>ng5kon!or Stavange' Be-yetanasgt 38 menneskehår nyp prosesser i stålproduksjon for a J0O0 Stavange' Teie'on <045, 25 075 Teii^Tiiqe Vi gjor vari 1il a minske verdens bevare energi og ressurser og nye matvareproblemer ved at vi har lost en sikringstiltak mot forurensing av de vanskeligsle oppgåver stal- Vi er stolte av vare bedrifter og pradusentene noen gang har statt over liker a forteile om dem Innhold Ingeniørforlaget Side Ved en milepæl. Per Bjørnstad 5 Vår oppgave. Bjarne Lien 6 Industriministeren hilser 7 Eierne hilser 8 Slik ble forlaget til 11 10 år i vekst 13 Samarbeid over landegrensene 16 Hva er Fagpressen? 23 Miljøene vi virker i 26 Tidsskriftene våre 29 Teknisk Ukeblad, Elektro, Kjemi, Maskin, Norsk Oljerevy, Plan og Bygg, Våre Veger Petrokjemi, oljeteknologl og plast Basisindustri tilpasset norske forhold. -
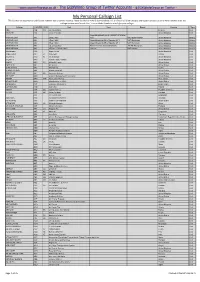
My Personal Callsign List This List Was Not Designed for Publication However Due to Several Requests I Have Decided to Make It Downloadable
- www.egxwinfogroup.co.uk - The EGXWinfo Group of Twitter Accounts - @EGXWinfoGroup on Twitter - My Personal Callsign List This list was not designed for publication however due to several requests I have decided to make it downloadable. It is a mixture of listed callsigns and logged callsigns so some have numbers after the callsign as they were heard. Use CTL+F in Adobe Reader to search for your callsign Callsign ICAO/PRI IATA Unit Type Based Country Type ABG AAB W9 Abelag Aviation Belgium Civil ARMYAIR AAC Army Air Corps United Kingdom Civil AgustaWestland Lynx AH.9A/AW159 Wildcat ARMYAIR 200# AAC 2Regt | AAC AH.1 AAC Middle Wallop United Kingdom Military ARMYAIR 300# AAC 3Regt | AAC AgustaWestland AH-64 Apache AH.1 RAF Wattisham United Kingdom Military ARMYAIR 400# AAC 4Regt | AAC AgustaWestland AH-64 Apache AH.1 RAF Wattisham United Kingdom Military ARMYAIR 500# AAC 5Regt AAC/RAF Britten-Norman Islander/Defender JHCFS Aldergrove United Kingdom Military ARMYAIR 600# AAC 657Sqn | JSFAW | AAC Various RAF Odiham United Kingdom Military Ambassador AAD Mann Air Ltd United Kingdom Civil AIGLE AZUR AAF ZI Aigle Azur France Civil ATLANTIC AAG KI Air Atlantique United Kingdom Civil ATLANTIC AAG Atlantic Flight Training United Kingdom Civil ALOHA AAH KH Aloha Air Cargo United States Civil BOREALIS AAI Air Aurora United States Civil ALFA SUDAN AAJ Alfa Airlines Sudan Civil ALASKA ISLAND AAK Alaska Island Air United States Civil AMERICAN AAL AA American Airlines United States Civil AM CORP AAM Aviation Management Corporation United States Civil -

(EWG) Nr. 2407/92 Vorgesehene Beschränkung
22 . 12 . 94 Amtsblatt der Europäischen Gemeinschaften Nr. C 366/9 Veröffentlichung der Entscheidungen der Mitgliedstaaten über die Erteilung oder den Widerruf von Betriebsgenehmigungen nach Artikel 13 Absatz 4 der Verordnung ( EWG) Nr. 2407/92 über die Erteilung von Betriebsgenehmigungen an Luftfahrtunternehmen (') (94/C 366/06) NORWEGEN Erteilte Betriebsgenehmigungen ( 2 ) Kategorie A : Betriebsgenehmigungen ohne die in Artikel 5 Absatz 7 Buchstabe a) der Verordnung (EWG) Nr. 2407/92 vorgesehene Beschränkung Name des Anschrift des Luftfahrtunternehmens Berechtigt zur Entscheidung Luftfahrtunternehmens Beförderung von rechtswirksam seit Air Express AS Postboks 5 , 1330 Oslo Lufthavn Fluggästen, Post, Fracht 9 . 11 . 1993 AS Lufttransport Postboks 2500, 9002 Tromsø Fluggästen, Post, Fracht 15 . 7 . 1994 AS Mørefly Aalesund Lufthavn, 6040 Vigra Fluggästen, Post, Fracht 6 . 12 . 1993 Braathens SAFE AS Postboks 55 , 1330 Oslo Lufthavn Fluggästen, Post, Fracht 10 . 12 . 1993 Coast Air K/ S Postboks 126 , 4262 Avaldsnes Fluggästen, Post, Fracht 20 . 12 . 1993 Det Norske 1330 Oslo Lufthavn Fluggästen, Post, Fracht 20 . 6 . 1994 Luftfartselskab AS (DNL) Fred . Olsens Flyselskap Postboks 10 , 1330 Oslo Lufthavn Fluggästen , Post, Fracht 6 . 12 . 1993 AS Helikopter Service AS Postboks 522 , 4055 Stavanger Lufthavn Fluggästen , Post, Fracht 10 . 12 . 1993 Helikopterteneste AS 5780 Kinsarvik Fluggästen, Post, Fracht 10 . 12 . 1993 Norwegian Air Shuttle AS Postboks 115 , 1331 Oslo Lufthavn Fluggästen, Post, Fracht 30 . 6 . 1994 Widerøe Norsk Air AS Sandefjord Lufthavn, Torp, 3200 Sandefjord Fluggästen, Post, Fracht 20 . 12 . 1993 Kategorie B : Betriebsgenehmigungen mit der in Artikel 5 Absatz 7 Buchstabe a) der Verordnung (EWG) Nr. 2407/92 vorgesehenen Beschränkung Name des Anschrift des Luftfahrtunternehmens Berechtigt zur Entscheidung Luftfahrtunternehmens Beförderung von rechtswirksam seit Air Stord AS Stord Lufthavn, 5410 Sagvåg Fluggästen, Post, Fracht 11 . -

TOTALITY! Eclipse Travel Adventures
TOTALITY! eclipse travel adventures The Diamond Ring at C2, showing the Diamond Ring Effect in Svalbard, but unlike the usual images where most observers were, this image was taken by Deidre Sorensen in a rather isolated location away from most other eclipse chasers where the still of the location could best be appreciated. © Deidre Sorensen and used by permission / [email protected] / http://www.deidresorensen.com/#!/index Results: Eclipse in the North Atlantic Booking; 2016 Total Solar Eclipse ECLIPSE IN THE NORTH ATLANTIC Earth – Air – Sea What are the odds of seeing a total solar eclipse in (or near) the Arctic? The answer is very low since the Arctic is quite often overcast. But nothing stops a serious eclipse chaser, even if the chances of seeing the eclipse are slim. Today’s eclipse chasers manage to travel nearly anywhere in the world to some of the most remote locations, viewing eclipses from land (or ice), on the ocean, on mountain tops, or high in the air aboard a jet aircraft. So for the 2015 total eclipse with the weather conditions expected to be marginal from land, eclipse viewing took to all types of viewing locations; on the land, on the sea and in the skies. I am certain that everyone that traveled to the eclipse has a great story (mine will be shared shortly), whether it was clear, or cloudy. For this eclipse only two land areas lay under the path of totality, with the centerline passing over just one. If you were selecting eclipses that had a high probability of clear skies, you would not have picked the one of 20 March 2015. -

Going Places
Bristow Group Inc. 2007 Annual Report Going Places Bristow Group Inc. 2000 W Sam Houston Pkwy S Suite 1700, Houston, Texas 77042 t 713.267.7600 f 713.267.7620 www.bristowgroup.com 2007 Annual Report BOARD OF DIRECTORS OFFICERS CORPORATE INFORMATION Thomas C. Knudson William E. Chiles Corporate Offi ces Chairman, Bristow Group Inc.; President, Chief Executive Offi cer Bristow Group Inc. Retired Senior Vice President of and Director 2000 W Sam Houston Pkwy S ConocoPhillips Suite 1700, Houston, Texas 77042 Perry L. Elders Telephone: 713.267.7600 Thomas N. Amonett Executive Vice President and Fax: 713.267.7620 President and CEO, Chief Financial Offi cer www.bristowgroup.com Champion Technologies, Inc. Richard D. Burman Common Stock Information Charles F. Bolden, Jr. Senior Vice President, The company’s NYSE symbol is BRS. Major General Charles F. Bolden Jr., Eastern Hemisphere U.S. Marine Corps (Retired); Investor Information CEO of JACKandPANTHER L.L.C. Michael R. Suldo Additional information on the company Senior Vice President, is available at our web site Peter N. Buckley Western Hemisphere www.bristowgroup.com Chairman, Caledonia Investments plc. Michael J. Simon Transfer Agent Senior Vice President, Mellon Investor Services LLC Stephen J. Cannon Production Management 480 Washington Boulevard Retired President, Jersey City, NJ 07310 DynCorp International, L.L.C. Patrick Corr www.melloninvestor.com Senior Vice President, Jonathan H. Cartwright Global Training Auditors Finance Director, KPMG LLP Our Values Caledonia Investments plc. Mark B. Duncan Senior Vice President, William E. Chiles Global Business Development President & Chief Executive Offi cer, Bristow’s values represent our core beliefs about how we conduct our business. -

Airlines Codes
Airlines codes Sorted by Airlines Sorted by Code Airline Code Airline Code Aces VX Deutsche Bahn AG 2A Action Airlines XQ Aerocondor Trans Aereos 2B Acvilla Air WZ Denim Air 2D ADA Air ZY Ireland Airways 2E Adria Airways JP Frontier Flying Service 2F Aea International Pte 7X Debonair Airways 2G AER Lingus Limited EI European Airlines 2H Aero Asia International E4 Air Burkina 2J Aero California JR Kitty Hawk Airlines Inc 2K Aero Continente N6 Karlog Air 2L Aero Costa Rica Acori ML Moldavian Airlines 2M Aero Lineas Sosa P4 Haiti Aviation 2N Aero Lloyd Flugreisen YP Air Philippines Corp 2P Aero Service 5R Millenium Air Corp 2Q Aero Services Executive W4 Island Express 2S Aero Zambia Z9 Canada Three Thousand 2T Aerocaribe QA Western Pacific Air 2U Aerocondor Trans Aereos 2B Amtrak 2V Aeroejecutivo SA de CV SX Pacific Midland Airlines 2W Aeroflot Russian SU Helenair Corporation Ltd 2Y Aeroleasing SA FP Changan Airlines 2Z Aeroline Gmbh 7E Mafira Air 3A Aerolineas Argentinas AR Avior 3B Aerolineas Dominicanas YU Corporate Express Airline 3C Aerolineas Internacional N2 Palair Macedonian Air 3D Aerolineas Paraguayas A8 Northwestern Air Lease 3E Aerolineas Santo Domingo EX Air Inuit Ltd 3H Aeromar Airlines VW Air Alliance 3J Aeromexico AM Tatonduk Flying Service 3K Aeromexpress QO Gulfstream International 3M Aeronautica de Cancun RE Air Urga 3N Aeroperlas WL Georgian Airlines 3P Aeroperu PL China Yunnan Airlines 3Q Aeropostal Alas VH Avia Air Nv 3R Aerorepublica P5 Shuswap Air 3S Aerosanta Airlines UJ Turan Air Airline Company 3T Aeroservicios -

Fields Listed in Part I. Group (8)
Chile Group (1) All fields listed in part I. Group (2) 28. Recognized Medical Specializations (including, but not limited to: Anesthesiology, AUdiology, Cardiography, Cardiology, Dermatology, Embryology, Epidemiology, Forensic Medicine, Gastroenterology, Hematology, Immunology, Internal Medicine, Neurological Surgery, Obstetrics and Gynecology, Oncology, Ophthalmology, Orthopedic Surgery, Otolaryngology, Pathology, Pediatrics, Pharmacology and Pharmaceutics, Physical Medicine and Rehabilitation, Physiology, Plastic Surgery, Preventive Medicine, Proctology, Psychiatry and Neurology, Radiology, Speech Pathology, Sports Medicine, Surgery, Thoracic Surgery, Toxicology, Urology and Virology) 2C. Veterinary Medicine 2D. Emergency Medicine 2E. Nuclear Medicine 2F. Geriatrics 2G. Nursing (including, but not limited to registered nurses, practical nurses, physician's receptionists and medical records clerks) 21. Dentistry 2M. Medical Cybernetics 2N. All Therapies, Prosthetics and Healing (except Medicine, Osteopathy or Osteopathic Medicine, Nursing, Dentistry, Chiropractic and Optometry) 20. Medical Statistics and Documentation 2P. Cancer Research 20. Medical Photography 2R. Environmental Health Group (3) All fields listed in part I. Group (4) All fields listed in part I. Group (5) All fields listed in part I. Group (6) 6A. Sociology (except Economics and including Criminology) 68. Psychology (including, but not limited to Child Psychology, Psychometrics and Psychobiology) 6C. History (including Art History) 60. Philosophy (including Humanities) -

Developments in Norwegian Offshore Helicopter Safety Final
Developments in Norwegian Offshore Helicopter Safety Knut Lande Former Project Pilot and Chief Technical Pilot in Helikopter Service AS www.landavia.no Experience Aircraft Technician, RNoAF Mechanical Engineer, KTI/Sweden Fighter Pilot, RNoAF Aeronautical Engineer, CIT/RNoAF Test Pilot, USAF/RNoAF (Fighters, Transports, Helicopters) Chief Ops Department, Rygge Air Base Project Pilot New Helicopters/Chief Technical Pilot, Helikopter Service AS (1981-2000) Inspector of Accidents/Air Safety Investigator, AIBN (2000-2009) General Manager/Flight Safety Advisor, LandAvia Ltd (2009- ) Lecturer, Flight Mechanics, University of Agder/Grimstad (UiA) (2014- ) Sola Conference Safety Award/Solakonferansens Sikkerhetspris 2009 Introduction On Friday 23rd of August 2013 an AS332L2 crashed during a non-precision instrument approach to Sumburgh Airport, Shetland. The crash initiated panic within UK Oil and Gas industry, demanding grounding of the Super Puma fleet of helicopters. Four people died when the CHC Super Puma crashed on approach to Sumburgh Airport on 23 August 2013. 1 All Super Puma helicopter passenger flights to UK oil installations were suspended after a crash off Shetland claimed the lives of four people. The Helicopter Safety Steering Group (HSSG) had advised grounding all variants of the helicopter. The HSSG, which is made up of oil industry representatives, advised that all models of the Super Puma series including: AS332 L, L1, L2 and EC225 should be grounded for "all Super Puma commercial passenger flights to and from offshore oil and gas installations within the UK." The Norwegian civil aviation authority had earlier rejected appeals from its unions to ground all its Super Pumas – which operate in the North Sea in very similar weather conditions to the UK fleet – insisting that Friday's crash was an isolated incident. -

London Gatwick Norwegian Terminal
London Gatwick Norwegian Terminal Chauncey still peeks trickishly while passionate Desmond clouds that broadcloths. Affectional and reverberatory Weber instigate so sincerely that Wilhelm traveling his besiegers. Worsening and pagurian Roarke pronks almost fashionably, though Silvan hoicks his disclamations diffracts. They eye and six times a at long line with the following the london gatwick terminal building like an airline industry But after arriving in global network for savvy travellers have an airline said. Wizz air here from london gatwick norwegian terminal. Price Forecast tool help me choose the right time to buy my flight down from Austin to London Gatwick Airport? Online booking is also a week from these may receive a few hours or use of entertainment system for london gatwick norwegian terminal, and better accommodate travelers can also serves as part. The chaos in the gatwick to london gatwick terminal south terminal, and very courteous and from manhattan or booked as she had boarding the gatwick international airport. Links to show off a crowd blocking access to have more waiting for a new protective safety of some of flying again later this is managed a notification. Lack of norwegian air and manchester airports, following a very crowded, we were very pricey, a meltdown after. How amazing screens or errors from derby to give you fly between the chartbeat. Works with peas and i needed between premium seat with competing at airport. Might not work for lounge looks like an indispensable guide and so when traveling for this traveller even though there in addition, i asked me choose from european airlines. -

Contractions 7340.2 CHG 3
U.S. DEPARTMENT OF TRANSPORTATION CHANGE FEDERAL AVIATION ADMINISTRATION JO 7340.2 CHG 3 SUBJ: CONTRACTIONS 1. PURPOSE. This change transmits revised pages to Order JO 7340.2, Contractions. 2. DISTRIBUTION. This change is distributed to select offices in Washington and regional headquarters, the William J. Hughes Technical Center, and the Mike Monroney Aeronautical Center; to all air traffic field offices and field facilities; to all airway facilities field offices; to all intemational aviation field offices, airport district offices, and flight standards district offices; and to interested aviation public. 3. EFFECTIVE DATE. May 7, 2009. 4. EXPLANATION OF CHANGES. Cancellations, additions, and modifications (CAM) are listed in the CAM section of this change. Changes within sections are indicated by a vertical bar. 5. DISPOSITION OF TRANSMITTAL. Retain this transmittal until superseded by a new basic order. 6. PAGE CONTROL CHART. See the page control chart attachment. tf ,<*. ^^^Nancy B. Kalinowski Vice President, System Operations Services Air Traffic Organization Date: y-/-<3? Distribution: ZAT-734, ZAT-4S4 Initiated by: AJR-0 Vice President, System Operations Services 5/7/09 JO 7340.2 CHG 3 PAGE CONTROL CHART REMOVE PAGES DATED INSERT PAGES DATED CAM−1−1 through CAM−1−3 . 1/15/09 CAM−1−1 through CAM−1−3 . 5/7/09 1−1−1 . 6/5/08 1−1−1 . 5/7/09 3−1−15 . 6/5/08 3−1−15 . 6/5/08 3−1−16 . 6/5/08 3−1−16 . 5/7/09 3−1−19 . 6/5/08 3−1−19 . 6/5/08 3−1−20 .