Respiratory Tract and Thorax: Summary Stage 2018 Coding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pubid-1446077038.Pdf
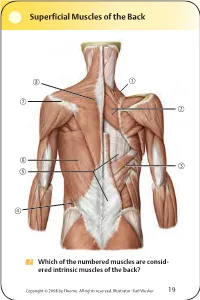
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

E Pleura and Lungs
Bailey & Love · Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy · Bailey & Love Bailey & Love · Essential Clinical Anatomy · Bailey & Love · EssentialChapter Clinical4 Anatomy e pleura and lungs • The pleura ............................................................................63 • MCQs .....................................................................................75 • The lungs .............................................................................64 • USMLE MCQs ....................................................................77 • Lymphatic drainage of the thorax ..............................70 • EMQs ......................................................................................77 • Autonomic nervous system ...........................................71 • Applied questions .............................................................78 THE PLEURA reections pass laterally behind the costal margin to reach the 8th rib in the midclavicular line and the 10th rib in the The pleura is a broelastic serous membrane lined by squa- midaxillary line, and along the 12th rib and the paravertebral mous epithelium forming a sac on each side of the chest. Each line (lying over the tips of the transverse processes, about 3 pleural sac is a closed cavity invaginated by a lung. Parietal cm from the midline). pleura lines the chest wall, and visceral (pulmonary) pleura Visceral pleura has no pain bres, but the parietal pleura covers -

Variations in Dimensions and Shape of Thoracic Cage with Aging: an Anatomical Review
REVIEW ARTICLE Anatomy Journal of Africa, 2014; 3 (2): 346 – 355 VARIATIONS IN DIMENSIONS AND SHAPE OF THORACIC CAGE WITH AGING: AN ANATOMICAL REVIEW ALLWYN JOSHUA, LATHIKA SHETTY, VIDYASHAMBHAVA PARE Correspondence author: S.Allwyn Joshua, Department of Anatomy, KVG Medical College, Sullia- 574327 DK, Karnataka,India. Email: [email protected]. Phone number; 09986380713. Fax number – 08257233408 ABSTRACT The thoracic cage variations in dimensions and proportions are influenced by age, sex and race. The objective of the present review was to describe the age related changes occurring in thoracic wall and its influence on the pattern of respiration in infants, adult and elderly. We had systematically reviewed, compared and analysed many original and review articles related to aging changes in chest wall images and with the aid of radiological findings recorded in a span of four years. We have concluded that alterations in the geometric dimensions of thoracic wall, change in the pattern and mechanism of respiration are influenced not only due to change in the inclination of the rib, curvature of the vertebral column even the position of the sternum plays a pivotal role. Awareness of basic anatomical changes in thoracic wall and respiratory physiology with aging would help clinicians in better understanding, interpretation and to differentiate between normal aging and chest wall deformation. Key words: Thoracic wall; Respiration; Ribs; Sternum; vertebral column INTRODUCTION The thoracic skeleton is an osteocartilaginous cage movement to the volume displacement of the frame around the principal organs of respiration lungs was evaluated by (Agostoni et al,m 1965; and circulation. It is narrow above and broad Grimby et al., 1968; Loring, 1982) for various below, flattened antero-posteriorly and longer human body postures. -

On the Anatomy of Intercostal Spaces in Man and Certain Other Mammals1 by Prof
ON THE ANATOMY OF INTERCOSTAL SPACES IN MAN AND CERTAIN OTHER MAMMALS1 BY PROF. M. A. H. SIDDIQI, M.B., D.L.O., M.S., F.R.C.S. (ENG.) AND DR A. N. MULLICK, M.B., B.S. Anatomy Department, King George's Medical College, Lucknow (India) TIHE standard description of the anatomy of the intercostal space has been discussed by Stibbe in a paper recently published in this Journal(2,3). Prof. Walmsley in 1916(1) showed that the intercostal nerves do not lie in the plane between the internal and external intercostal muscles but deep to the internal intercostal, and that they are separated from the pleura by a deeper musculo-fascial plane consisting of subcostal, intercostal and transversus thoracis muscles from behind forwards. According to Davies, Gladstone and Stibbe (3) there are four musculo-fascial planes in each space and in each space the main nerve lies with a collateral nerve deep to the internal intercostal. As the above paper effected a change in the teaching of the anatomy of intercostal space, we carried out the following investigations on human as well as on certain other Mammalian intercostal spaces. DISSECTION OF HUMAN INTERCOSTAL SPACES Sixty thoraces of different ages were dissected. From some of them the intercostal spaces were cut out en bloc to facilitate dissection; in others the thoracic wall was dissected as a whole. In the case of the foetuses microscopic sections were made to locate the muscular planes and the nerves. The results of our dissection were as follows: I. Intercostal muscles (fig. -

Thoracic Wall Foreign Bodies Following Penetrating Trauma in Pediatric Age Group: Report of Two Cases with Literature Review
CASE REPORT East J Med 25(1): 173-176, 2020 DOI: 10.5505/ejm.2020.68094 Thoracic Wall Foreign Bodies Following Penetrating Trauma In Pediatric Age Group: Report of Two Cases With Literature Review Volkan Sarper Erikci Department of Pediatric Surgery, Sağlık Bilimleri University Tepecik Training Hospital, Izmir, Turkey ABSTRACT Penetrating chest trauma is rarely seen in childhood. Following penetrative trauma various foreign objects may be detected as embedded in the tissues. A precise and prompt diagnosis together with an appropriate surgical management is paramount in these cases for a good prognosis. Here we present 2 cases with 2 different foreign bodies embedded in thoracic wall following different penetrating thoracic traumas. The purpose this report to critique the properties and handling of penetrative chest wall trauma in children with regard to post-traumatic retained FBs in thoracic wall and the topic is discussed under the light of relevant literature. Key Words: Chest wall trauma-retained foreign body-children Introduction cartridge bullet (Figure 1). There were not any findings consistent with hemo-pneumothorax or Penetrating chest injury may pose difficulty in pulmonary parenchymal injury in imaging studies like diagnosis of these cases for the health provider. chest roentgenogram and computed tomography. An Foreign bodies (FB) in thoracic wall after a easily palpable radiopaque FB was observed in the left penetrative injury are scarcely seen in childhood. hemithoracic wall adjacent to thoracic vertebrae There is a wide spectrum of foreign objects retained (Figure 2). Under general anesthesia during surgical in thorax following a trauma and these include bullets, intervention a midline rigid object was palpated 5 cm shrapnel, a piece of wearing, bones, rib particles and medial and away from to the wound. -

LATISSIMUS DORSI FLAP for HEAD and NECK RECONSTRUCTION Patrik Pipkorn, Ryan Jackson, Bruce Haughey
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY LATISSIMUS DORSI FLAP FOR HEAD AND NECK RECONSTRUCTION Patrik Pipkorn, Ryan Jackson, Bruce Haughey The latissimus dorsi is the largest muscle in Benefits the body by surface area. It can be as large as 20 x 40cms, enabling latissimus dorsi • Easy flap to learn to harvest flaps to cover very large defects (Figure 1). • Large thin muscle that can cover very large defects • Long (5-15cm) vascular pedicle if dis- sected up to the subscapular artery • The subscapular artery has a diameter of 2-5mm • Minimal long-term donor site morbidity • Can be harvested as a muscle flap or with a skin paddle • Can be harvested as a chimeric flap (multiple otherwise independent flaps that each have an independent vascular supply with all pedicles linked to a common source vessel) along with other flaps based on a singular subscapular artery Caveats • Donor site is close to head and neck area making two team harvest difficult, though not impossible Figure 1: Large pedicled latissimus dorsi • Because the donor site is on the back, it flap makes positioning more tedious • Large wound and potential dead space The flap can be harvested as a pedicled or after harvest has high risk of a seroma free flap and as a muscular or myocuta- neous flap with an overlying skin paddle. It can also be harvested along with any other Surgical anatomy flap based on the subscapular vascular system as a chimeric or subscapular “mega- The latissimus dorsi mainly adducts and flap”. Despite its size it can be harvested medially rotates the arm. -
Recognizing Pneumothorax-A Case Study
Recognizing Pneumothorax-A Case Study Mary Black Johnson, PhD, ATC Mark Haines, MA, ATC Brian Barry, MA, ATC Metropolitan State College Assistant Athletic Trainer The Jim Davis Connection Denver, Colorado San Diego State University Carlsbad, California 9%-neumothorax injuries are lung to expand fully within its own position and air is expired from infrequent but can be life threat- pleural sac. the lungs. The passive expiration ening. They are most often associ- During inspiration, the dia- process becomes active and is facili- ated with blunt trauma of the phragm contracts and flattens tated by contraction of abdominal chest. The trauma causes rib frac- while the ribs are lifted by contrac- and chest muscles during exercise. ture, which in turn perforates the tion of the intercostal muscles. pleural wall. Thus, air or gas accu- Thus, the negative pressure in- 9njuw Changes mulates in the pleural cavity and creases, resulting in air flow from in Respiration causes the lung to collapse. It is the atmosphere into the increased critical to recognize the signs and area of the lungs. When the chest wall is pierced, in symptoms of this condition in or- When the muscles involved in either an open or closed chest in- der to provide prompt and suc- respiration relax, the diaphragm jury, normal pressure gradients cessful treatment in what can be a returns to its dome-shaped resting are altered. The normal pressure medical emergency. , fluid-filled balloon Dynamics 1 , of Normal Breathing Within the thoracic cage, each lung resides in a separate com- partment, the pleural sac. Between the thoracic wall and the pleural sac is a thin layer of intrapleural fluid (Vander et al., 1985) (Fig- ure 1). -

The Pleura1 with Special Reference to Fibrothorax
Thorax (1970), 25, 515. The pleura1 With special reference to fibrothorax N. R. BARRETT Royal College of Surgeons of England We have met to honour and to remember Arthur always at his side; amongst the physicians, Sir Tudor Edwards, who died after the Second World Geoffrey Marshall helped him to found the War and who devoted much of his professional Thoracic Society in 1945. life to the advancement of thoracic surgery. Looking back upon the 1920s one can see that He lived and worked towards the end of an the emblems were not favourable for thoracic era when surgeons were 'prima donnas'. He was surgeons. J. E. H. Roberts and Tudor Edwards a man of handsome and commanding appear- had no beds of their own at the Brompton Hos- ance: his convictions *were strong and to his pital; they were at first at the beck and call of friends he was a staunch ally; the others he the physicians who decreed the operations they allowed to cultivate their own gardens. considered appropriate. The majority of these He was a pioneer in his own field and became were for general surgical conditions; little could one of the first thoracic surgeons in the United be done for chest diseases. But within a decade Kingdom to achieve an international reputation. the picture had changed: the Brompton had He deserved more recognition from his contem- become a Mecca for all who were interested in poraries in England than they gave him; indeed, his only honour was a medal from his colleagues in Norway. The reason was that thoracic surgery was not at first accepted as more than a foray into unlikely and hazardous territory. -
Powerpoint Handout: Lab 1, Thorax
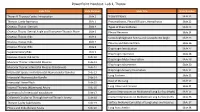
PowerPoint Handout: Lab 1, Thorax Slide Title Slide Number Slide Title Slide Number Thorax & Thoracic Cavity: Introduction Slide 2 Visceral Pleura Slide 21 Thoracic Cavity Apertures Slide 3 Pneumothorax, Pleural Effusion, Hemothorax Slide 22 Osseous Thorax: Sternum Slide 4 Types of Pneumothorax Slide 23 Osseous Thorax: Sternal Angle and Transverse Thoracic Plane Slide 5 Pleural Recesses Slide 24 Osseous Thorax: Ribs Slide 6 Costodiaphragmatic Recess and Costophrenic Angle Slide 25 Osseous Thorax: Ribs Slide 7 Pleurisy and Referred Pain Slide 26 Osseous Thorax: Ribs Slide 8 Diaphragm Introduction Slide 27 Supernumerary Ribs Slide 9 Diaphragm Apertures Slide 28 Osseous Thorax: Rib Joints Slide 10 Diaphragm Motor Innervation Slide 29 Muscular Thorax: Intercostal Muscles Slide 11 Diaphragm Movements Slide 30 Muscular Thorax: Intercostal Muscles (Continued) Slide 12 Diaphragm Sensory Innervation Slide 31 Intercostal Spaces and Intercostal Neurovascular Bundles Slide 13 Lung Surfaces Slide 32 Intercostal Neurovascular Bundle Slide 14 Root of the Lung Slide 33 Intercostal Nerve Block Slide 15 Slide 34 Internal Thoracic (Mammary) Artery Slide 16 Lung Lobes and Fissures Summary of of Intercostal Vasculature Slide 17 Contact Impressions on Mediastinal Lung Surface (Right) Slide 35 Collateral Circulation Through Internal Thoracic Artery Slide 18 Contact Impressions on Mediastinal Lung Surface (Left) Slide 36 Thoracic Cavity Subdivisions Slide 19 Surface Anatomy Correlates of Lung Lobes and Fissures Slide 37 Pleura and Endothoracic Fascia Slide 20 Lung Auscultation Slide 38 Thorax & Thoracic Cavity: Introduction The thorax refers to the region of the body between the neck https://3d4medic.al/enFsQOFf and the abdomen. The thoracic cavity is an irregularly shaped cylinder enclosed by the musculoskeletal walls of the thorax and the diaphragm. -

Human Anatomy: Thoracic Wall
Thoracic wall - structure, blood supply and innervation Ingrid Hodorová UPJŠ LF, Dept. of Anatomy MediTec training for students 1.-15.9.2019, Kosice, Slovakia Thoracic borders external - Upper: jugular notch, clavicule, acromion scapulae, spine of C7 (vertebra prominens) Lower: xiphoid process, costal arches (right and left), Th12 internal - Upper: superior thoracic aperture: jugular notch, 1. pair of ribs, Th1 Lower: inferior thoracic aperture: diaphragm (right side - to 4. ICS left side - to 5. ICS) Lines of orientation Anterior axillary l. Anterior median line (midsternal) Scapular l. Sternal line Middle axillary l. Paravertebral l. Parasternal l. Posterior median line Midclavicular l. Posterior axillary l. Layers of thoracic wall ► Deep layer - osteothorax, muscles of proper thoracic wall + intrinsic muscles of the back, deep structures, endothoracic fascia ► Middle layer - thoracohumeral mm., spinohumeral mm., spinocostal mm., (fascie, vessels, nerves) ► Superficial layer - skin, subcutaneous tissue, superficial structures, mammary gland ►Deep layer Osteothorax - ribs - sternum - thoracic vertebrae Osteothorax Ribs Types of ribs: Sternum - manunbrium of sternum - body of sternum - xiphoid process - manunbriosternal and xiphisternal synchondrosis(synostosis) Movement of the ribs and sternum during breathing Thoracic vertebrae - body - arch (lamina+pedicles) - spinous process - transverse processes - superior and inferior articular processes Joints of the ribs anteriorly ►sternocostal joints (2nd-5th ribs) posteriorly ►costovertebral -

Thorax Syllabus
THORAX COURSE CONTENT COMPETENCIES The first year medical student should be able to understand and describe the gross anatomy of thoracic wall, mediastinum and the contents of thoracic cavity, correlate the anatomical basis of clinical manifestations /clinical procedures pertaining to thorax and describe the radiological anatomy of thorax. REGIONS AND ORGANS THORACIC WALL THORACIC INLET Boundaries and contents Level 2: Details Level 3: Thoracic outlet syndrome THORACIC OUTLET Boundaries, diaphragm,attachments, major openings and their vertebral levels Level 2: Functional correlation; Minor openings Level 3: Development and congenital anomalies RIB CAGE THORAX Typical intercostal space – Boundaries and contents; Atypical intercostal space; Movements of respiration Level 2: Accessory muscles of respiration Level 3: Applied aspects: Barrel chest, pectus excavatum, rickety rosary MEDIASTINUM Divisions and major contents Level 2: Details Level 3: Applied aspects: Mediastinitis, mediastinoscopy SUPERIOR AND POSTERIOR MEDIASTINA Boundaries and contents: Trachea, Oesophagus, Aorta, Azygos system, Thoracic duct Level 2: Superior mediastinal Syndrome, Course, relation and branches / area of drainage Level 3: Applied aspects: Coarctation of aorta, aneurysm, developmental anomalies PLEURA Pleural reflections, recesses, innervation Level 2: Functional importance of recesses Level 3: Pleuritis, pleural effusion, pleural tap, posterior approach to kidney (importance of pleural reflection) 41 LUNGS Gross description including lobes, fissures and bronchopulmonary