Anatomy of the Thoracic Wall, Pulmonary Cavities, and Mediastinum
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Part 1 the Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3
ECA1 7/18/06 6:30 PM Page 1 Part 1 The Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3 Surface anatomy and surface markings The experienced clinician spends much of his working life relating the surface anatomy of his patients to their deep structures (Fig. 1; see also Figs. 11 and 22). The following bony prominences can usually be palpated in the living subject (corresponding vertebral levels are given in brackets): •◊◊superior angle of the scapula (T2); •◊◊upper border of the manubrium sterni, the suprasternal notch (T2/3); •◊◊spine of the scapula (T3); •◊◊sternal angle (of Louis) — the transverse ridge at the manubrio-sternal junction (T4/5); •◊◊inferior angle of scapula (T8); •◊◊xiphisternal joint (T9); •◊◊lowest part of costal margin—10th rib (the subcostal line passes through L3). Note from Fig. 1 that the manubrium corresponds to the 3rd and 4th thoracic vertebrae and overlies the aortic arch, and that the sternum corre- sponds to the 5th to 8th vertebrae and neatly overlies the heart. Since the 1st and 12th ribs are difficult to feel, the ribs should be enu- merated from the 2nd costal cartilage, which articulates with the sternum at the angle of Louis. The spinous processes of all the thoracic vertebrae can be palpated in the midline posteriorly, but it should be remembered that the first spinous process that can be felt is that of C7 (the vertebra prominens). The position of the nipple varies considerably in the female, but in the male it usually lies in the 4th intercostal space about 4in (10cm) from the midline. -
Pubid-1446077038.Pdf
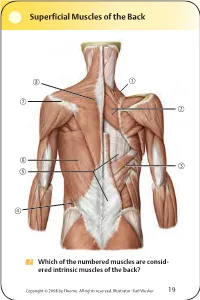
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

The Effect of the Moufarrege Total Posterior Pedicle Reduction Mammaplasty on the Erogenous Sensation of the Nipple
Surgical Science, 2019, 10, 127-140 http://www.scirp.org/journal/ss ISSN Online: 2157-9415 ISSN Print: 2157-9407 The Effect of the Moufarrege Total Posterior Pedicle Reduction Mammaplasty on the Erogenous Sensation of the Nipple Richard Moufarrege1,2*, Mohammed El Mehdi El Yamani1, Laura Barriault1, Ahmed Amine Alaoui1 1Faculty of Medicine, Université de Montréal, Montreal, Canada 2Department of Plastic Surgery, Université de Montréal, Montreal, Canada How to cite this paper: Moufarrege, R., El Abstract Yamani, M.E.M., Barriault, L. and Alaoui, A.A. (2019) The Effect of the Moufarrege Traditional reduction mammoplasties have the simple concern to guarantee Total Posterior Pedicle Reduction Mam- the survival of the nipple areola complex after surgery. Little has been done to maplasty on the Erogenous Sensation of the take care of essential functions in the nipple, especially the erogenous sensa- Nipple. Surgical Science, 10, 127-140. https://doi.org/10.4236/ss.2019.104016 tion. We have conducted a retrospective study on a cohort of 573 female pa- tients operated using the Total Posterior Pedicle of Moufarrege between 1985 Received: February 25, 2019 and 1995 to evaluate its effect on the erogenous sensation of the nipple. This Accepted: April 23, 2019 study demonstrated the preservation of the erogenous sensation of the nipple Published: April 26, 2019 in a high proportion of these patients. The physiology of this preservation is Copyright © 2019 by author(s) and explained in regard of the technique details in Moufarrege mammoplasty Scientific Research Publishing Inc. compared to other techniques. The Moufarrege Total Posterior Pedicle would This work is licensed under the Creative therefore be a highly reliable reduction technique to ensure the preservation Commons Attribution International License (CC BY 4.0). -

Ch22: Actions of the Respiratory Muscles
CHAPTER 22 ACTIONS OF THE RESPIRATORY MUSCLES André de Troyer he so-called respiratory muscles are those muscles that caudally and ventrally from their costotransverse articula- Tprovide the motive power for the act of breathing. Thus, tions, such that their ventral ends and the costal cartilages although many of these muscles are involved in a variety of are more caudal than their dorsal parts (Figure 22-2B, C). activities, such as speech production, cough, vomiting, and When the ribs are displaced in the cranial direction, their trunk motion, their primary task is to displace the chest wall ventral ends move laterally and ventrally as well as cra- rhythmically to pump gas in and out of the lungs. The pres- nially, the cartilages rotate cranially around the chon- ent chapter, therefore, starts with a discussion of the basic drosternal junctions, and the sternum is displaced ventrally. mechanical structure of the chest wall in humans. Then, the Consequently, there is usually an increase in both the lateral action of each group of muscles is analyzed. For the sake of and the dorsoventral diameters of the rib cage (see Figure clarity, the functions of the diaphragm, the intercostal mus- 22-2B, C). Conversely, a displacement of the ribs in the cau- cles, the muscles of the neck, and the muscles of the abdom- dal direction is usually associated with a decrease in rib cage inal wall are analyzed sequentially. However, since all these diameters. As a corollary, the muscles that elevate the ribs as muscles normally work together in a coordinated manner, their primary action have an inspiratory effect on the rib the most critical aspects of their mechanical interactions are cage, whereas the muscles that lower the ribs have an expi- also emphasized. -

Suggested Osteopathic Treatment.Pdf
Suggested Osteopathic Treatment of Respiratory Diseases Processes Region Biomechanical Model Neurological Model Cardio/Resp Model Metabolic Model Behavioral Model Sample Techniques Head/OA Improve motion CN X - Improve Parasympathetic innervations affect Improve CSF flow (part Reduces anxiety associated with Sub-occipital release; OA decompression; parasympathetic balance heart rate; Improve PRM of PRM) contraction of disease Sinus Drainage (if sings of URI) C-Spine C3-5 Diaphragm C3-5 Diaphragm Assist lymph movement Reduces anxiety associated with Soft Tissue/Myofascial of C-spine, BLT, contraction of disease MET, Counterstrain Thoracic Improve rib cage Stellate Ganglion Lymph drainage (bolster immune Improve oxygenation Normalizes sympathetic drive thus Thoracic Outlet Release, 1st rib release, Outlet motion response) balancing somatopsychological pathways Sternum Improve rib cage Intercostal nerves Improve lymph flow (bolster immune Improve oxygenation Normalizes sympathetic drive thus Sternal/ C-T myofascial release motion response) (reduces work of balancing somatopsychological breathing) pathways Upper Scapula – improve rib Brachial plexus Improve lymph flow Normalizes sympathetic drive thus Scapular balancing, Spencer’s technique, Extremity cage function balancing somatopsychological MET, Counterstrain, Upper Extremity pathways Wobble technique Thoracic Improve rib cage Celiac, Inferior and Improve lymph flow Improve oxygenation Normalizes sympathetic drive thus Soft Tissue/Myofascial of T-spine or Spine motion superior mesenteric -

The Variations of the Subclavian Artery and Its Branches Ahmet H
Okajimas Folia Anat. Jpn., 76(5): 255-262, December, 1999 The Variations of the Subclavian Artery and Its Branches By Ahmet H. YUCEL, Emine KIZILKANAT and CengizO. OZDEMIR Department of Anatomy, Faculty of Medicine, Cukurova University, 01330 Balcali, Adana Turkey -Received for Publication, June 19,1999- Key Words: Subclavian artery, Vertebral artery, Arterial variation Summary: This study reports important variations in branches of the subclavian artery in a singular cadaver. The origin of the left vertebral artery was from the aortic arch. On the right side, no thyrocervical trunk was found. The two branches which normally originate from the thyrocervical trunk had a different origin. The transverse cervical artery arose directly from the subclavian artery and suprascapular artery originated from the internal thoracic artery. This variation provides a short route for posterior scapular anastomoses. An awareness of this rare variation is important because this area is used for diagnostic and surgical procedures. The subclavian artery, the main artery of the The variations of the subclavian artery and its upper extremity, also gives off the branches which branches have a great importance both in blood supply the neck region. The right subclavian arises vessels surgery and in angiographic investigations. from the brachiocephalic trunk, the left from the aortic arch. Because of this, the first part of the right and left subclavian arteries differs both in the Subjects origin and length. The branches of the subclavian artery are vertebral artery, internal thoracic artery, This work is based on a dissection carried out in thyrocervical trunk, costocervical trunk and dorsal the Department of Anatomy in the Faculty of scapular artery. -

The Azygos Vein System in the Rat
THE AZYGOS VEIN SYSTEM IN THE RAT MYRON H. HALPERN' Departments of Anatomy, University of Xichigan, Ann Arbor, and Hahnemann Medical College, Philadelphia THREE FIGURES The adult pattern of the azygos vein system of various mam- mals has received the attention of many early investigators (Eustachius, 1561; Bardeleben, 1848 ; Marshall, 1850; and Morrison, 1879). Since there has not almways been agreement among these workers in the patterns described, attempts were made by some of them to try to correlate the patterns on a de- velopmental basis (Barcleleben, 1848 ; Marshall, 1850; and Parker and Tozier, 1897). Tihey ( 'B), Kampmeier ( 'la), Sabin ( '14, '15), and Reagan ('19) each described the develop- ment of the azygos system of a different mammal. Although there was partial agreement on certain aspects of the embry- ology, it was not until recently that there has been general accord. Since one of the more significant contributions to the development of the azygos system in the rat (Strong, '36) has never appeared as a journal article and is procurable only as a thesis from the Indiana University Library, it will be included and related to the present description of the adult pattern. MATERIALS To investigate the constancy of pattern and to check fully the points of previous disagreement in the adult pattern, 57 rats were studied by the fluorescent-latex injection technique previously described by the author ( '52). Eleven additional 1 The author wishes to thank Dr. Russell T. Woodburne, Department of Anatomy, University of Michigan for his critical reading of this manuscript. a Portion of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the University of Michigan. -
The Descending Thoracic Aorta Morphological Characteristics
ARS Medica Tomitana - 2016; 3(22): 186 - 191 10.1515/arsm-2016-0031 Malik S., Bordei P., Rusali A., Iliescu D. M. The descending thoracic aorta morphological characteristics Faculty of Medicine, “Ovidius” University, Constanta ABSTRACT Introduction Our study was conducted by consulting angioCT sites made on a CT GE LightSpeed VCT64 Slice CT and a CT GE LightSpeed 16 Slice CT, following the path and relationships of the descending thoracic aorta against the vertebral column, outside diameters thereof at the Descending thoracic aorta extends from the thoracic vertebrae T4, T7, T12 and posterior intercostal aortic arch (which it continues) and aortic hiatus of arteries characteristics. The origin of of the descending the diaphragm at level of T12 vertebra [1,2,3,4,5] thoracic aorta we found most commonly on the left corresponding to the front of T10 [6], level that flank of the lower edge of the vertebral body T4, but continues with the abdominal descending aorta. She I have encountered cases where it had come above the enters the posterior mediastinum at the T4 vertebra and lower edge of T4 on level of intervertebral disc T4-T5 or describes a trajectory which is vertically downward as even at the upper edge of T5 vertebral body. At thoracic a whole, being slightly inferior oblique and to the right, vertebra T4, on a total of 30 cases, the descending thoracic aorta present a diameter of 20.0 to 32.6 mm, then, first at a distance of 2-3 cm midline, progressive values that correspond to male gender and to females approach to become median and prevertebral at the diameter ranging from 25.5 to 27, 4 mm. -

The Neuroanatomy of Female Pelvic Pain
Chapter 2 The Neuroanatomy of Female Pelvic Pain Frank H. Willard and Mark D. Schuenke Introduction The female pelvis is innervated through primary afferent fi bers that course in nerves related to both the somatic and autonomic nervous systems. The somatic pelvis includes the bony pelvis, its ligaments, and its surrounding skeletal muscle of the urogenital and anal triangles, whereas the visceral pelvis includes the endopelvic fascial lining of the levator ani and the organ systems that it surrounds such as the rectum, reproductive organs, and urinary bladder. Uncovering the origin of pelvic pain patterns created by the convergence of these two separate primary afferent fi ber systems – somatic and visceral – on common neuronal circuitry in the sacral and thoracolumbar spinal cord can be a very dif fi cult process. Diagnosing these blended somatovisceral pelvic pain patterns in the female is further complicated by the strong descending signals from the cerebrum and brainstem to the dorsal horn neurons that can signi fi cantly modulate the perception of pain. These descending systems are themselves signi fi cantly in fl uenced by both the physiological (such as hormonal) and psychological (such as emotional) states of the individual further distorting the intensity, quality, and localization of pain from the pelvis. The interpretation of pelvic pain patterns requires a sound knowledge of the innervation of somatic and visceral pelvic structures coupled with an understand- ing of the interactions occurring in the dorsal horn of the lower spinal cord as well as in the brainstem and forebrain. This review will examine the somatic and vis- ceral innervation of the major structures and organ systems in and around the female pelvis. -

Lower Respiratory Tract – Larynx – Trachea – Tracheobronchial Tree – Respiratory Compartment
Respiratory system II. © David Kachlík 30.9.2015 Anatomical division • upper respiratory tract – nasal cavity – paranasal cavities – nasopharynx • lower respiratory tract – larynx – trachea – tracheobronchial tree – respiratory compartment © David Kachlík 30.9.2015 Anatomical Surgical division division • upper respiratory tract • upper respiratory tract – nasal cavity – nasal cavity – paranasal cavities – paranasal cavities – nasopharynx – nasopharynx – larynx • lower respiratory tract • lower respiratory tract – larynx border: apertura thoracis sup. – trachea – trachea – tracheobronchial tree – tracheobronchial tree – respiratory compartment – respiratory compartment © David Kachlík 30.9.2015 General structure of respiratory system wall • tunica mucosa (mucosa) – epithelium - ciliated pseudostratified columnar (respiratory epithelium) - non-keratinized stratified squamous - lamina basalis – lamina propria • glands (seromucinous tuboalveolar), lymph nodes (noduli lymphoidei) • tunica fibromusculocartilaginea – collagenous and elastic tissue (and its ligaments – larynx, trachea) – smooth muscles (trachea, bronchi, bronchioli) – skeletal muscles (larynx) • tunica serosa or tunica adventitia – tunica serosa (pleura) has three layers: • mesothelium – lamina basalis • lamina propria • tela subserosa © David Kachlík 30.9.2015 © David Kachlík 30.9.2015 Trachea • pars cervicalis (C6- C7) • pars thoracica (T1-T4) newborn at the level of C4, child C5 • bifurcatio tracheae (T4) = 1st branching of tracheobronchial tree • carina tracheae • calibers: