1. Anatomical Basis of Thoracic Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Corporate Medical Policy Surgery for Groin Pain in Athletes
Corporate Medical Policy Surgery for Groin Pain in Athletes File Name: surgery_for_groin_pain_in_athletes Origination: 8/2014 Last CAP Review: 6/2020 Next CAP Review: 6/2021 Last Review: 6/2020 Description of Procedure or Service Sports-related groin pain, commonly known as athletic pubalgia or sports hernia, is characterized by disabling activity-dependent lower abdominal and groin pain that is not attributable to any other cause. Athletic pubalgia is most frequently diagnosed in high-performance male athletes, particularly those who participate in sports that involve rapid twisting and turning such as soccer, hockey, and football. Alternative names include Gilmore’s groin, osteitis pubis, pubic inguinal pain syndrome, inguinal disruption, slap shot gut, sportsmen’s groin, footballers groin injury complex, hockey groin syndrome, athletic hernia, sports hernia and core muscle injury. For patients who fail conservative therapy, surgical repair of any defects identified in the muscles, tendons or nerves has been proposed. Groin pain in athletes is a poorly defined condition, for which there is not a consensus regarding the cause and/or treatment. Some believe the groin pain is an occult hernia process, a prehernia condition, or an incipient hernia, with the major abnormality being a defect in the transversalis fascia, which forms the posterior wall of the inguinal canal. Another theory is that injury to soft tissues that attach to or cross the pubic symphysis is the primary abnormality. The most common of these injuries is thought to be at the insertion of the rectus abdominis onto the pubis, with either primary or secondary pain arising from the adductor insertion sites onto the pubis. -

Copyrighted Material
C01 10/31/2017 11:23:53 Page 1 1 1 The Normal Anatomy of the Neck David Bainbridge Introduction component’ of the neck is a common site of pathology, and the diverse forms of neck The neck is a common derived characteristic disease reflect the sometimes complex and of land vertebrates, not shared by their aquatic conflicting regional variations and functional ancestors. In fish, the thoracic fin girdle, the constraints so evident in this region [2]. precursor of the scapula, coracoid and clavi- Unlike the abdomen and thorax, there is no cle, is frequently fused to the caudal aspect of coelomic cavity in the neck, yet its ventral part the skull. In contrast, as vertebrates emerged is taken up by a relatively small ‘visceral on to the dry land, the forelimb separated from compartment’, containing the larynx, trachea, the head and the intervening vertebrae speci- oesophagus and many important vessels, alised to form a relatively mobile region – the nerves and endocrine glands. However, I neck – to allow the head to be freely steered in will not review these structures, as they do many directions. not represent an extension of the equine ‘back’ With the exception of the tail, the neck in the same way that the more dorsal locomo- remains the most mobile region of the spinal tor region does. column in modern-day horses. It permits a wide range of sagittal plane flexion and exten- sion to allow alternating periods of grazing Cervical Vertebrae 3–7 and predator surveillance, as well as frontal plane flexion to allow the horizon to be scan- Almost all mammals, including the horse, ned, and rotational movement to allow possess seven cervical vertebrae, C1 to C7 nuisance insects to be flicked off. -
Pubid-1446077038.Pdf
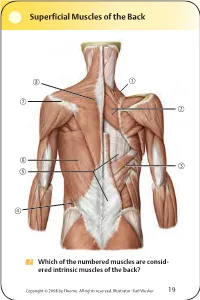
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

Of the Pediatric Mediastinum
MRI of the Pediatric Mediastinum Dianna M. E. Bardo, MD Director of Body MR & Co-Director of the 3D Innovation Lab Disclosures Consultant & Speakers Bureau – honoraria Koninklijke Philips Healthcare N V Author – royalties Thieme Publishing Springer Publishing Mediastinum - Anatomy Superior Mediastinum thoracic inlet to thoracic plane thoracic plane to diaphragm Inferior Mediastinum lateral – pleural surface anterior – sternum posterior – vertebral bodies Mediastinum - Anatomy Anterior T4 Mediastinum pericardium to sternum Middle Mediastinum pericardial sac Posterior Mediastinum vertebral bodies to pericardium lateral – pleural surface superior – thoracic inlet inferior - diaphragm Mediastinum – MR Challenges Motion Cardiac ECG – gating/triggering Breathing Respiratory navigation Artifacts Intubation – LMA Surgical / Interventional materials Mediastinum – MR Sequences ECG gated/triggered sequences SSFP – black blood SE – IR – GRE Non- ECG gated/triggered sequences mDIXON (W, F, IP, OP), eTHRIVE, turbo SE, STIR, DWI Respiratory – triggered, radially acquired T2W MultiVane, BLADE, PROPELLER Mediastinum – MR Sequences MRA / MRV REACT – non Gd enhanced Gd enhanced sequences THRIVE, mDIXON, mDIXON XD Mediastinum – Contents Superior Mediastinum PVT Left BATTLE: Phrenic nerve Vagus nerve Structures at the level of the sternal angle Thoracic duct Left recurrent laryngeal nerve (not the right) CLAPTRAP Brachiocephalic veins Cardiac plexus Aortic arch (and its 3 branches) Ligamentum arteriosum Thymus Aortic arch (inner concavity) Trachea Pulmonary -

Groin and Buttock Claudication Associated with Vascular Origin Due to Chronic Occlusion of Internal Iliac Artery -A Case Report
Anesth Pain Med 2015; 10: 93-96 http://dx.doi.org/10.17085/apm.2015.10.2.93 ■Case Report■ Groin and buttock claudication associated with vascular origin due to chronic occlusion of internal iliac artery -A case report- Departments of Anesthesiology and Pain Medicine, *Internal Medicine, Kangdong Sacred Heart Hospital, Hallym University College of † Medicine, Seoul, Ire Pain Clinic, Incheon, Korea Hyun Mo Chung, Sang-Soo Kang, Keun-Man Shin, Sang-hoon Lee, Sung Eun Kim*, and Hong-Seong Yoo† Neurogenic and vascular claudication is sometimes difficult to When concomitant symptoms such as radiating pain are distinguish from each other due to similarities in symptoms. present, a herniated disc could be considered first [3]. We Symptoms and physical examinations may not always match the report a rare case of severe groin pain of vascular origin, severity in both diseases, and when atypical symptoms, such as groin pain, are present, diagnosis can be more challenging. Proper associated with mild pain in the buttock and lower leg, differential diagnosis of the two is important because of the without the typical vascular symptoms due to well developed invasiveness of treatment in both diseases. We report a rare case collateral flow of abdominal wall vessels. of a patient with severe groin and buttock pain due to chronic occlusion of the internal iliac artery, along with a review of the relevant literature. (Anesth Pain Med 2015; 10: 93-96) CASE REPORT Key Words: Claudication, Groin, Internal iliac artery, Pain. A 70-year-old male with persistent bilateral groin pain, more severe on the left, visited our department of pain medicine. -

Sportsmans Groin: the Inguinal Ligament and the Lloyd Technique
Rennie, WJ and Lloyd, DM. Sportsmans Groin: The Inguinal Ligament and the Lloyd Technique. Journal of the Belgian Society of Radiology. 2017; 101(S2): 16, pp. 1–4. DOI: https://doi.org/10.5334/jbr-btr.1404 OPINION ARTICLE Sportsmans Groin: The Inguinal Ligament and the Lloyd Technique WJ Rennie and DM Lloyd Groin pain is a catch all phrase used to define a common set of symptoms that affect many individuals. It is a common condition affecting sportsmen and women (1, 2) and is often referred to as the sportsman groin (SG). Multiple surgical operations have been developed to treat these symptoms yet no definitive imaging modalities exist to diagnose or predict prognosis. This article aims to discuss the anatomy of the groin, suggest a biomechanical pathophysiology and outline a logical surgical solution to treat the underlying pathology. A systematic clinical and imaging approach with inguinal ligament and pubic specific MRI assessment, can result in accurate selection for intervention. Close correlation with clinical examination and imaging in series is recommended to avoid misinterpretation of chronic changes in athletes. Keywords: Groin pain; Inguinal Ligament; MRI; Surgery; Lloyd release Introduction from SG is due to altered biomechanics, with specific pain Groin pain is a catch all phrase used to define a common symptoms that differ from those caused by inguinal or set of symptoms that affect many individuals. It is a com- femoral hernias. mon condition affecting sportsmen and women [1, 2] and is often referred to as the sportsman groin (SG). Multiple Anatomy of Sportsman’s Groin surgical operations have been developed to treat these The anatomical central structure in the groin is the pubic symptoms, yet no definitive imaging modalities exist to bone. -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

E Pleura and Lungs
Bailey & Love · Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy · Bailey & Love Bailey & Love · Essential Clinical Anatomy · Bailey & Love · EssentialChapter Clinical4 Anatomy e pleura and lungs • The pleura ............................................................................63 • MCQs .....................................................................................75 • The lungs .............................................................................64 • USMLE MCQs ....................................................................77 • Lymphatic drainage of the thorax ..............................70 • EMQs ......................................................................................77 • Autonomic nervous system ...........................................71 • Applied questions .............................................................78 THE PLEURA reections pass laterally behind the costal margin to reach the 8th rib in the midclavicular line and the 10th rib in the The pleura is a broelastic serous membrane lined by squa- midaxillary line, and along the 12th rib and the paravertebral mous epithelium forming a sac on each side of the chest. Each line (lying over the tips of the transverse processes, about 3 pleural sac is a closed cavity invaginated by a lung. Parietal cm from the midline). pleura lines the chest wall, and visceral (pulmonary) pleura Visceral pleura has no pain bres, but the parietal pleura covers -

The Digestive System
69 chapter four THE DIGESTIVE SYSTEM THE DIGESTIVE SYSTEM The digestive system is structurally divided into two main parts: a long, winding tube that carries food through its length, and a series of supportive organs outside of the tube. The long tube is called the gastrointestinal (GI) tract. The GI tract extends from the mouth to the anus, and consists of the mouth, or oral cavity, the pharynx, the esophagus, the stomach, the small intestine, and the large intes- tine. It is here that the functions of mechanical digestion, chemical digestion, absorption of nutrients and water, and release of solid waste material take place. The supportive organs that lie outside the GI tract are known as accessory organs, and include the teeth, salivary glands, liver, gallbladder, and pancreas. Because most organs of the digestive system lie within body cavities, you will perform a dissection procedure that exposes the cavities before you begin identifying individual organs. You will also observe the cavities and their associated membranes before proceeding with your study of the digestive system. EXPOSING THE BODY CAVITIES should feel like the wall of a stretched balloon. With your skinned cat on its dorsal side, examine the cutting lines shown in Figure 4.1 and plan 2. Extend the cut laterally in both direc- out your dissection. Note that the numbers tions, roughly 4 inches, still working with indicate the sequence of the cutting procedure. your scissors. Cut in a curved pattern as Palpate the long, bony sternum and the softer, shown in Figure 4.1, which follows the cartilaginous xiphoid process to find the ventral contour of the diaphragm. -

Pleurectomy Through the Triangle of Auscultation
Thorax: first published as 10.1136/thx.37.12.945 on 1 December 1982. Downloaded from Thorax 1982;37:945-946 Pleurectomy through the triangle of auscultation OJ LAU, S SHAWKAT From the Thoracic Surgical Unit, Preston Hall Hospital, Aylesford, Kent The aetiology of primary spontaneous pneumothorax is Outpatient follow-up for one to three years has shown no unknown, though several theories have been proposed. The recurrence of pneumothorax. formation and rupture of "blebs" in the lung are frequently associated with primary pneumothorax, 1-3 but the manage- Discussion ment of the condition remains controversial and depends on its severity and the patient's previous medical history. For For most cases of primary spontaneous pneumothorax, definitive treatment pleurectomy still remains the treatment observation, bed rest, or intercostal tube drainage are of choice.4 5 We have treated 25 young patients with primary adequate; but for patients with persistent air leak, and for spontaneous pneumothorax with apical pleurectomy those with a history of recurrent attacks, some form of through the auscultation triangle, without incision of the definitive treatment is necessary. Various methods have muscles of the chest wall. We have found that this approach been recommended, from artificial obliteration of the has several advantages over a full thoracotomy. pleural space with various chemicals or oils to the stripping of the parietal pleura and closure of the air leak through a Operative technique and results formal thoracotomy. In our experience, these forms of treatment are often Twenty-five young patients with primary spontaneous associated with unnecessary pain and discomfort for the pneumothorax have been treated, of whom 15 were men. -

Congenital Bone Deformities and the Inbred Wolves (Canis Lupus) of Isle Royale
ARTICLE IN PRESS Biological Conservation xxx (2009) xxx–xxx Contents lists available at ScienceDirect Biological Conservation journal homepage: www.elsevier.com/locate/biocon Congenital bone deformities and the inbred wolves (Canis lupus) of Isle Royale Jannikke Räikkönen a,*, John A. Vucetich b, Rolf O. Peterson b, Michael P. Nelson c a Swedish Museum of Natural History, Department of Contaminant Research, Frescativägen 44, P.O. Box 50007, S-104 05 Stockholm, Sweden b School of Forest Resources and Environmental Science, Michigan Technological University, Houghton, MI 49931, USA c Lyman Briggs College, Department of Fisheries and Wildlife, and Department of Philosophy, Michigan State University, East Lansing, MI 48825, USA a r t i c l e i n f o a b s t r a c t Article history: The wolf (Canis lupus) population on Isle Royale, a remote island in Lake Superior, North America, is extre- Received 26 October 2008 mely inbred. Nevertheless, the consequences of genetic deterioration have not been detected for this Received in revised form 21 January 2009 intensively studied population, until now. We found that 58% (n = 36) of Isle Royale wolves exhibited Accepted 24 January 2009 some kind of congenital malformation in the lumbosacral region of the vertebral column and 33% exhib- Available online xxxx ited a specific malformity, lumbosacral transitional vertebrae. By contrast, only 1% (1 of 99) of wolves sampled from two outbred, wolf populations exhibited this malformity. Moreover, in domestic dogs Keywords: (Canis lupus familiaris) lumbosacral transitional vertebrae are associated with cauda equina syndrome, Canis lupus which can cause paresis, paralysis, locomotor difficulties in the rear legs and tail, and back pain.