Pleurectomy Through the Triangle of Auscultation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Vertebral Column and Thorax
Introduction to Human Osteology Chapter 4: Vertebral Column and Thorax Roberta Hall Kenneth Beals Holm Neumann Georg Neumann Gwyn Madden Revised in 1978, 1984, and 2008 The Vertebral Column and Thorax Sternum Manubrium – bone that is trapezoidal in shape, makes up the superior aspect of the sternum. Jugular notch – concave notches on either side of the superior aspect of the manubrium, for articulation with the clavicles. Corpus or body – flat, rectangular bone making up the major portion of the sternum. The lateral aspects contain the notches for the true ribs, called the costal notches. Xiphoid process – variably shaped bone found at the inferior aspect of the corpus. Process may fuse late in life to the corpus. Clavicle Sternal end – rounded end, articulates with manubrium. Acromial end – flat end, articulates with scapula. Conoid tuberosity – muscle attachment located on the inferior aspect of the shaft, pointing posteriorly. Ribs Scapulae Head Ventral surface Neck Dorsal surface Tubercle Spine Shaft Coracoid process Costal groove Acromion Glenoid fossa Axillary margin Medial angle Vertebral margin Manubrium. Left anterior aspect, right posterior aspect. Sternum and Xyphoid Process. Left anterior aspect, right posterior aspect. Clavicle. Left side. Top superior and bottom inferior. First Rib. Left superior and right inferior. Second Rib. Left inferior and right superior. Typical Rib. Left inferior and right superior. Eleventh Rib. Left posterior view and left superior view. Twelfth Rib. Top shows anterior view and bottom shows posterior view. Scapula. Left side. Top anterior and bottom posterior. Scapula. Top lateral and bottom superior. Clavicle Sternum Scapula Ribs Vertebrae Body - Development of the vertebrae can be used in aging of individuals. -
Part 1 the Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3
ECA1 7/18/06 6:30 PM Page 1 Part 1 The Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3 Surface anatomy and surface markings The experienced clinician spends much of his working life relating the surface anatomy of his patients to their deep structures (Fig. 1; see also Figs. 11 and 22). The following bony prominences can usually be palpated in the living subject (corresponding vertebral levels are given in brackets): •◊◊superior angle of the scapula (T2); •◊◊upper border of the manubrium sterni, the suprasternal notch (T2/3); •◊◊spine of the scapula (T3); •◊◊sternal angle (of Louis) — the transverse ridge at the manubrio-sternal junction (T4/5); •◊◊inferior angle of scapula (T8); •◊◊xiphisternal joint (T9); •◊◊lowest part of costal margin—10th rib (the subcostal line passes through L3). Note from Fig. 1 that the manubrium corresponds to the 3rd and 4th thoracic vertebrae and overlies the aortic arch, and that the sternum corre- sponds to the 5th to 8th vertebrae and neatly overlies the heart. Since the 1st and 12th ribs are difficult to feel, the ribs should be enu- merated from the 2nd costal cartilage, which articulates with the sternum at the angle of Louis. The spinous processes of all the thoracic vertebrae can be palpated in the midline posteriorly, but it should be remembered that the first spinous process that can be felt is that of C7 (the vertebra prominens). The position of the nipple varies considerably in the female, but in the male it usually lies in the 4th intercostal space about 4in (10cm) from the midline. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -
Skeletal System? Skeletal System Chapters 6 & 7 Skeletal System = Bones, Joints, Cartilages, Ligaments
Warm-Up Activity • Fill in the names of the bones in the skeleton diagram. Warm-Up 1. What are the 4 types of bones? Give an example of each. 2. Give 3 ways you can tell a female skeleton from a male skeleton. 3. What hormones are involved in the skeletal system? Skeletal System Chapters 6 & 7 Skeletal System = bones, joints, cartilages, ligaments • Axial skeleton: long axis (skull, vertebral column, rib cage) • Appendicular skeleton: limbs and girdles Appendicular Axial Skeleton Skeleton • Cranium (skull) • Clavicle (collarbone) • Mandible (jaw) • Scapula (shoulder blade) • Vertebral column (spine) • Coxal (pelvic girdle) ▫ Cervical vertebrae • Humerus (arm) ▫ Thoracic vertebrae • Radius, ulna (forearm) ▫ Lumbar vertebrae • Carpals (wrist) • Metacarpals (hand) ▫ Sacrum • Phalanges (fingers, toes) ▫ Coccyx • Femur (thigh) • Sternum (breastbone) • Tibia, fibula (leg) • Ribs • Tarsal, metatarsals (foot) • Calcaneus (heel) • Patella (knee) Functions of the Bones • Support body and cradle soft organs • Protect vital organs • Movement: muscles move bones • Storage of minerals (calcium, phosphorus) & growth factors • Blood cell formation in bone marrow • Triglyceride (fat) storage Classification of Bones 1. Long bones ▫ Longer than they are wide (eg. femur, metacarpels) 2. Short bones ▫ Cube-shaped bones (eg. wrist and ankle) ▫ Sesamoid bones (within tendons – eg. patella) 3. Flat bones ▫ Thin, flat, slightly curved (eg. sternum, skull) 4. Irregular bones ▫ Complicated shapes (eg. vertebrae, hips) Figure 6.2 • Adult = 206 bones • Types of bone -

The Influence of the Rib Cage on the Static and Dynamic Stability
www.nature.com/scientificreports OPEN The infuence of the rib cage on the static and dynamic stability responses of the scoliotic spine Shaowei Jia1,2, Liying Lin3, Hufei Yang2, Jie Fan2, Shunxin Zhang2 & Li Han3* The thoracic cage plays an important role in maintaining the stability of the thoracolumbar spine. In this study, the infuence of a rib cage on static and dynamic responses in normal and scoliotic spines was investigated. Four spinal fnite element (FE) models (T1–S), representing a normal spine with rib cage (N1), normal spine without rib cage (N2), a scoliotic spine with rib cage (S1) and a scoliotic spine without rib cage (S2), were established based on computed tomography (CT) images, and static, modal, and steady-state analyses were conducted. In S2, the Von Mises stress (VMS) was clearly decreased compared to S1 for four bending loadings. N2 and N1 showed a similar VMS to each other, and there was a signifcant increase in axial compression in N2 and S2 compared to N1 and S1, respectively. The U magnitude values of N2 and S2 were higher than in N1 and S1 for fve loadings, respectively. The resonant frequencies of N2 and S2 were lower than those in N1 and S1, respectively. In steady-state analysis, maximum amplitudes of vibration for N2 and S2 were signifcantly larger than N1 and S1, respectively. This study has revealed that the rib cage improves spinal stability in vibrating environments and contributes to stability in scoliotic spines under static and dynamic loadings. Scoliosis, a three-dimensional deformity, prevents healthy development. -

The Feasibility of Rib Grafts in Long Span Mandibular Defects Reconstruction: a Long Term Follow Up
Journal of Cranio-Maxillo-Facial Surgery 47 (2019) 15e22 Contents lists available at ScienceDirect Journal of Cranio-Maxillo-Facial Surgery journal homepage: www.jcmfs.com The feasibility of rib grafts in long span mandibular defects reconstruction: A long term follow up * Ahmed M.A. Habib , Shady A. Hassan Department of Maxillofacial and Plastic Surgery, Faculty of Dentistry, Alexandria University, Egypt article info abstract Article history: Aims: To evaluate the efficiency of reconstruction of long span mandibular defects using split rib bundle Paper received 10 June 2018 bone graft. Accepted 2 November 2018 Materials and methods: Six hundred patients with long span mandibular defects (more than 6 cm long), Available online 10 November 2018 following resection of aggressive mandibular tumours, were reconstructed with split rib bundle bone graft technique. Immediate reconstruction was performed in all patients. A reconstruction plate was used to Keywords: support the graft. Two ribs were harvested from the right side of the chest, split into four halves and used to Reconstruction restore the continuity of the mandible. The inclusion criterion was post-surgical mandibular bony defects Mandible fi Split rib without soft tissue de ciency. Defects with a history of previous or need of future irradiation were excluded. Results: The appearance of the patients was accepted in 550 patients. Functional reconstruction was done in 320 patients by osseointegrated dental implants (after 15 months), and removable prosthesis in 150 patients. Infection was minor in 31 patients, moderate in 47 patients and severe in 42 patients. Partial loss of graft, up to 25%, due to moderate infection was reported. -

Variations in Dimensions and Shape of Thoracic Cage with Aging: an Anatomical Review
REVIEW ARTICLE Anatomy Journal of Africa, 2014; 3 (2): 346 – 355 VARIATIONS IN DIMENSIONS AND SHAPE OF THORACIC CAGE WITH AGING: AN ANATOMICAL REVIEW ALLWYN JOSHUA, LATHIKA SHETTY, VIDYASHAMBHAVA PARE Correspondence author: S.Allwyn Joshua, Department of Anatomy, KVG Medical College, Sullia- 574327 DK, Karnataka,India. Email: [email protected]. Phone number; 09986380713. Fax number – 08257233408 ABSTRACT The thoracic cage variations in dimensions and proportions are influenced by age, sex and race. The objective of the present review was to describe the age related changes occurring in thoracic wall and its influence on the pattern of respiration in infants, adult and elderly. We had systematically reviewed, compared and analysed many original and review articles related to aging changes in chest wall images and with the aid of radiological findings recorded in a span of four years. We have concluded that alterations in the geometric dimensions of thoracic wall, change in the pattern and mechanism of respiration are influenced not only due to change in the inclination of the rib, curvature of the vertebral column even the position of the sternum plays a pivotal role. Awareness of basic anatomical changes in thoracic wall and respiratory physiology with aging would help clinicians in better understanding, interpretation and to differentiate between normal aging and chest wall deformation. Key words: Thoracic wall; Respiration; Ribs; Sternum; vertebral column INTRODUCTION The thoracic skeleton is an osteocartilaginous cage movement to the volume displacement of the frame around the principal organs of respiration lungs was evaluated by (Agostoni et al,m 1965; and circulation. It is narrow above and broad Grimby et al., 1968; Loring, 1982) for various below, flattened antero-posteriorly and longer human body postures. -
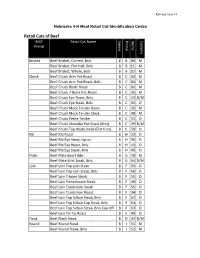
Retail Cuts of Beef BEEF Retail Cut Name Specie Primal Name Cookery Primal
Revised June 14 Nebraska 4-H Meat Retail Cut Identification Codes Retail Cuts of Beef BEEF Retail Cut Name Specie Primal Name Cookery Primal Brisket Beef Brisket, Corned, Bnls B B 89 M Beef Brisket, Flat Half, Bnls B B 15 M Beef Brisket, Whole, Bnls B B 10 M Chuck Beef Chuck Arm Pot-Roast B C 03 M Beef Chuck Arm Pot-Roast, Bnls B C 04 M Beef Chuck Blade Roast B C 06 M Beef Chuck 7-Bone Pot-Roast B C 26 M Beef Chuck Eye Roast, Bnls B C 13 D/M Beef Chuck Eye Steak, Bnls B C 45 D Beef Chuck Mock Tender Roast B C 20 M Beef Chuck Mock Tender Steak B C 48 M Beef Chuck Petite Tender B C 21 D Beef Chuck Shoulder Pot Roast (Bnls) B C 29 D/M Beef Chuck Top Blade Steak (Flat Iron) B C 58 D Rib Beef Rib Roast B H 22 D Beef Rib Eye Steak, Lip-on B H 50 D Beef Rib Eye Roast, Bnls B H 13 D Beef Rib Eye Steak, Bnls B H 45 D Plate Beef Plate Short Ribs B G 28 M Beef Plate Skirt Steak, Bnls B G 54 D/M Loin Beef Loin Top Loin Steak B F 59 D Beef Loin Top Loin Steak, Bnls B F 60 D Beef Loin T-bone Steak B F 55 D Beef Loin Porterhouse Steak B F 49 D Beef Loin Tenderloin Steak B F 56 D Beef Loin Tenderloin Roast B F 34 D Beef Loin Top Sirloin Steak, Bnls B F 62 D Beef Loin Top Sirloin Cap Steak, Bnls B F 64 D Beef Loin Top Sirloin Steak, Bnls Cap Off B F 63 D Beef Loin Tri-Tip Roast B F 40 D Flank Beef Flank Steak B D 47 D/M Round Beef Round Steak B I 51 M Beef Round Steak, Bnls B I 52 M BEEF Retail Cut Name Specie Primal Name Cookery Primal Beef Bottom Round Rump Roast B I 09 D/M Beef Round Top Round Steak B I 61 D Beef Round Top Round Roast B I 39 D Beef -

Respiratory Function of the Rib Cage Muscles
Copyright @ERS Journals Ltd 1993 Eur Respir J, 1993, 6, 722-728 European Respiratory Journal Printed In UK • all rights reserved ISSN 0903 • 1936 REVIEW Respiratory function of the rib cage muscles J.N. Han, G. Gayan-Ramirez, A. Dekhuijzen, M. Decramer Respiratory function of the rib cage muscles. J.N. Han, G. Gayan-Ramirez, R. Respiratory Muscle Research Unit, Labo Dekhuijzen, M. Decramer. ©ERS Journals Ltd 1993. ratory of Pneumology, Respiratory ABSTRACT: Elevation of the ribs and expansion of the rib cage result from the Division, Katholieke Universiteit Leuven, co-ordinated action of the rib cage muscles. We wished to review the action and Belgium. interaction of the rib cage muscles during ventilation. Correspondence: M. Decramer The parasternal intercostal muscles appear to play a predominant role during Respiratory Division quiet breathing, both in humans and in anaesthetized dogs. In humans, the para University Hospital sternal intercostals act in concert with the scalene muscles to expand the upper rib Weligerveld 1 cage, and/or to prevent it from being drawn inward by the action of the diaphragm. B-3212 Pellenberg The external intercostal muscles are considered to be active mainly during inspira Leuven tion, and the internal intercostal muscles during expiration. Belgium The respiratory activity of the external intercostals is minimal during quiet breathing both in man and in dogs, but increases with increasing ventilation. In Keywords: Chest wall mechanics contractile properties spiratory activity in the external intercostals can be enhanced in anaesthetized ani rib cage muscles mals and humans by inspiratory mechanical loading and by col stimulation, rib displacement suggesting that the external intercostals may constitute a reserve system, that may be recruited when the desired expansion of the rib cage is increased. -

General Production
Carcass Identification General Production Systems Operator Cattle Pusher The following positions are classified in the General Production job Cheeker Chiseler description for the Cargill Beef Chuck Cap Dropper facility in Schuyler, Nebraska. Chuck Cap Trimmer Chuck Cut Down Chuck Dropper 1st Hangoff Chuck Dropper To Saw 2nd Hangoff Chuck Flat Stager 3 4 Exchange Chuck Flat Trimmer Abomasum Boxer Chuck Hanger Abomasum Flusher Chuck Short Rib Trimmer Abomasum Trim Wash Chuck Skinner Operator Abomasum With Knife Chuck Trimmer Aorta Trimmer Clear Necks Armpit & Shanks Trimmer Clip Tails/Captive Shackle Back Strap Trimmer Clod Trimmer Bagger Loose Meats Cod Bag & Tail Trimmer Belly Ripper Cod Bag & Trail Trimmer Blade Meat Product Checker Combo Dumper Blade Meat Trimmer Combo Maker Blade Mt 81 Defect Trimmer Bone Hearts Defect Trimmer Whizard Box Product Knife Box Reject Line Double Cut Hock Cutter Box Room Down Puller Opeartor/Flush Boxers Heads Brisket Dropper Down Puller Operator/Flush Brisket Stager Heads Brisket Trimmer Ear & Eyelid Remover Bung Bag & Tie Ear Tag Bagger Bung Dropper Export Product Technician Button Bones/Whizard Faceplate Trimmer Knife-strips Feather Bone Popper Carcass Id Apply Tag Finger Meat Bagger Finger Meat Trimmer/Sizer Hotbox Unloader Flank Steak Trimmer Hs Hock Cutter Flap Meat Trim Inedible Ruffle Fat Flesher Inside Neck Trim Whizard Flume Opeator Knife Front Feet Hock Cutter Inside Skirt Trimmer Gn Flat Trim Inventory Control Grade Label Bag Person Kidney Popper Grade Stamper Knuckle Puller Ground Beef Boxer -

DEPARTMENT of ANATOMY IGMC SHIMLA Competency Based Under
DEPARTMENT OF ANATOMY IGMC SHIMLA Competency Based Under Graduate Curriculum - 2019 Number COMPETENCY Objective The student should be able to At the end of the session student should know AN1.1 Demonstrate normal anatomical position, various a) Define and demonstrate various positions and planes planes, relation, comparison, laterality & b) Anatomical terms used for lower trunk, limbs, joint movement in our body movements, bony features, blood vessels, nerves, fascia, muscles and clinical anatomy AN1.2 Describe composition of bone and bone marrow a) Various classifications of bones b) Structure of bone AN2.1 Describe parts, blood and nerve supply of a long bone a) Parts of young bone b) Types of epiphysis c) Blood supply of bone d) Nerve supply of bone AN2.2 Enumerate laws of ossification a) Development and ossification of bones with laws of ossification b) Medico legal and anthropological aspects of bones AN2.3 Enumerate special features of a sesamoid bone a) Enumerate various sesamoid bones with their features and functions AN2.4 Describe various types of cartilage with its structure & a) Differences between bones and cartilage distribution in body b) Characteristics features of cartilage c) Types of cartilage and their distribution in body AN2.5 Describe various joints with subtypes and examples a) Various classification of joints b) Features and different types of fibrous joints with examples c) Features of primary and secondary cartilaginous joints d) Different types of synovial joints e) Structure and function of typical synovial