The Pleura1 with Special Reference to Fibrothorax
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pubid-1446077038.Pdf
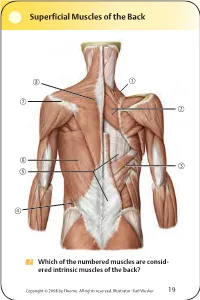
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

Treatment of Established Volkmann's Contracture*
~hop. Acta Treatment of Established Volkmann’sContracture* BY KENYA TSUGE, M.D.’J’, HIROSHIMA, JAPAN ldon, From the Department of Orthopaedic Surgery, Hiroshima Universi~.’ 1-76, School of Medicine, Hiroshima 38. The disease first described by Volkmann in 1881 is the extent of the disease: mild, moderate, and severe. In generally considered to result from spasm of the main ar- the mild type, also called the localized type, there was de- ~ts of teries of the forearm, and their branches as a consequence generation of part of the flexor digitorum profundus mus- Acta of trauma to the elbow or forearm. The severe and pro- cle, causing contractures in only two or three fingers. longed but incomplete interruption of arterial blood sup- There were hardly any neurological signs, and when pres- ~. (in ply, together with venostasis, produces acute ischemic ent they were minimum. In the moderate type, the muscle z and necrosis of the flexor muscles. The most marked ischemia degeneration involved all or nearly all of the flexor digito- occurs in the deeply situated muscles such as the flexor rum profundus and flexor pollicis longus, with partial pollicis longus and flexor digitorum profundus, but severe degeneration of the superficial muscles as well. The neu- ischemia is evident in the pronator teres and flexor rological signs were invariably present and generally -484, digitorum superficialis muscles, and comparatively mild the median nerve was more severely affected than the :rtag, ischemia occurs in the superficially located muscles such ulnar nerve. In the severe type, there was degeneration as the wrist flexors. The muscle degeneration which fol- of all the flexor muscles with necrosis in the center ). -

Rotator Cuff Tear Arthropathy: Pathophysiology, Diagnosis And
yst ar S em ul : C c u s r u r e M n t & R Orthopedic & Muscular System: c e Aydin, et al., Orthopedic Muscul Syst 2014, 3:2 i s d e e a p ISSN: 2161-0533r o c DOI: 10.4172/2161-0533-3-1000159 h h t r O Current Research Review Article Open Access Rotator Cuff Tear Arthropathy: Pathophysiology, Diagnosis and Treatment Nuri Aydin*, Okan Tok and Bariş Görgün Istanbul University Cerrahpaşa, School of Medicine, Istanbul, Turkey *Corresponding author: Nuri Aydin, Istanbul University Cerrahpaşa, School of Medicine, Orthopaedics and Traumatology, Istanbul, Turkey, Tel: +905325986232; E- mail: [email protected] Rec Date: Jan 25, 2014, Acc Date: Mar 22, 2014, Pub Date: Mar 28, 2014 Copyright: © 2014 Aydin N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract The term rotator cuff tear arthropathy is a broad spectrum pathology but it involves common characteristic features as rotator cuff tear, leading to glenohumeral joint arthritis and superior migration of the humeral head. Although there are several factors described causing rotator cuff tear arthropathy, the exact mechanism is still unknown because the rotator cuff tear arthropathy develops in only a group of patients with chronic rotator cuff tear. The aim of this article is to review pathophysiology of rotator cuff tear arthropathy, to explain the diagnostic features and to discuss the management of the disease. Keywords: Arthropathy; Glenohumeral joint; Articular fluid Rotator cuff tear not only plays a role at the beginning of the disease, but also a developed rotator cuff tear is a result of the inflammatory Introduction process. -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

Table of Contents 1
GENERAL THORACIC SURGERY DATABASE v.2.3 TRAINING MANUAL August 2017 Table of Contents 1. Demographics ................................................................................................................................................................. 2 2. Follow Up ........................................................................................................................................................................ 9 3. Admission ..................................................................................................................................................................... 10 4. Pre-Operative Evaluation ............................................................................................................................................. 14 5. Diagnosis (Category of Disease) ................................................................................................................................... 48 6. Procedure ..................................................................................................................................................................... 70 7. Post-Operative Events ................................................................................................................................................ 111 8. Discharge .................................................................................................................................................................... 135 9. Quality Measures ...................................................................................................................................................... -

On the Anatomy of Intercostal Spaces in Man and Certain Other Mammals1 by Prof
ON THE ANATOMY OF INTERCOSTAL SPACES IN MAN AND CERTAIN OTHER MAMMALS1 BY PROF. M. A. H. SIDDIQI, M.B., D.L.O., M.S., F.R.C.S. (ENG.) AND DR A. N. MULLICK, M.B., B.S. Anatomy Department, King George's Medical College, Lucknow (India) TIHE standard description of the anatomy of the intercostal space has been discussed by Stibbe in a paper recently published in this Journal(2,3). Prof. Walmsley in 1916(1) showed that the intercostal nerves do not lie in the plane between the internal and external intercostal muscles but deep to the internal intercostal, and that they are separated from the pleura by a deeper musculo-fascial plane consisting of subcostal, intercostal and transversus thoracis muscles from behind forwards. According to Davies, Gladstone and Stibbe (3) there are four musculo-fascial planes in each space and in each space the main nerve lies with a collateral nerve deep to the internal intercostal. As the above paper effected a change in the teaching of the anatomy of intercostal space, we carried out the following investigations on human as well as on certain other Mammalian intercostal spaces. DISSECTION OF HUMAN INTERCOSTAL SPACES Sixty thoraces of different ages were dissected. From some of them the intercostal spaces were cut out en bloc to facilitate dissection; in others the thoracic wall was dissected as a whole. In the case of the foetuses microscopic sections were made to locate the muscular planes and the nerves. The results of our dissection were as follows: I. Intercostal muscles (fig. -

Annals Royal College of Surgeons
ANNALS OF THE ROYAL COLLEGE OF SURGEONS OF ENGLAND Editor: SIR CECIL WAKELEY, BT., K.B.E., C.B., LL.D., M.Ch., D.SC., F.R.C.S., F.R.S.E., F.F.R., F.D.S.R.C.S. VOLUME 35 JULY-DECEMBER 1964 Published by THE ROYAL COLLEGE OF SURGEONS OF ENGLAND LINCOLN'S INN FIELDS LONDON, W.C.2 CONTENTS VOLUME 35 . JULY-DECEMBER 1964 JULY 1964 Page ON THE INTERDEPENDENCE OF SCIENCE AND THE HEALING ART Sir Charles Illingworth 1 HONOURS CONFERRED ON FELLOWS AND MEMBERS 14 THE GUBERNACULUM TESTIS HUNTERI: TESTICULAR DESCENT AND MALDESCENT .. K. M. Backhouse 15 PLASMA PEPSINOGEN: NORMAL AND ABNORMAL SECRETION A. R. Anscombe 34 GRANT OF FELLOWSHIP DIPLOMAS .. .. 49 CEREMONY OF PRESENTATION OF DIPLOMATES 52 APPOINTMENT OF FELLOWS AND MEMBERS TO CONSULTANT POSTS 56 COUNCIL AND COURT DINNER 57 PROCEEDINGS OF THE COUNCIL IN JUNE 60 IMPERIAL CANCER RESEARCH FUND .. 64 BINDING OF THE ANNALS .. 66 DIARY FOR JULY .. .. 66 DIARY FOR AUGUST .. .. 66 AUGUST 1964 PULMONARY TUBERCULOSIS IN RETROSPECT AND PROSPECT Sir Clement Price Thomas 67 ELECTION TO THE COUNCIL .. .. .. 83 PERMANENT URINARY DIVERSION IN CHILDHOOD P. P. Rickham 84 SIR HUGH LETT, BT... .. .. .. .. 105 TiHE BRITISH CLUB FOR SURGERY OF THE HAND .. 105 THE SEGMENTAL INNERVATION OF THE LOWER LIMB MUSCLES IN MAN .. .. .. .. .. W. J. W. SHARRARD 106 APPOINTMENT OF FELLOWS AND MEMBERS TO CONSULTANT POSTS 122 IN MEMORIAM: JAMES J. MASON BROWN .. .. 123 PROCEEDINGS OF THE COUNCIL IN JULY .. .. 125 BOOKS ADDED TO THE LIBRARY: JANUARY-MARCH 1964 127 DONATIONS .. .. .. .. .. .. 129 DIARY FOR AUGUST .. .. .. 130 DIARY FOR SEPTEMBER . -
Page 1 of 4 COPYRIGHT © by the JOURNAL of BONE and JOINT SURGERY, INCORPORATED LAMPLOT ET AL
COPYRIGHT © BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED LAMPLOT ET AL. RISK OF SUBSEQUENT JOINT ARTHROPLASTY IN CONTRALATERAL OR DIFFERENT JOINT AFTER INDEX SHOULDER, HIP, OR KNEE ARTHROPLASTY http://dx.doi.org/10.2106/JBJS.17.00948 Page 1 Appendix TABLE E-1 Included Alternative Primary Diagnoses ICD-9-CM Code Diagnosis* 716.91 Arthropathy NOS, shoulder 716.95 Arthropathy NOS, pelvis 716.96 Arthropathy NOS, lower leg 719.45 Joint pain, pelvis 719.91 Joint disease NOS, shoulder *NOS = not otherwise specified. Page 1 of 4 COPYRIGHT © BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED LAMPLOT ET AL. RISK OF SUBSEQUENT JOINT ARTHROPLASTY IN CONTRALATERAL OR DIFFERENT JOINT AFTER INDEX SHOULDER, HIP, OR KNEE ARTHROPLASTY http://dx.doi.org/10.2106/JBJS.17.00948 Page 2 TABLE E-2 Excluded Diagnoses* ICD-9- ICD-9- ICD-9- ICD-9- CM Code Diagnosis CM Code Diagnosis CM Code Diagnosis CM Code Diagnosis 274 Gouty arthropathy NOS 696 Psoriatic 711.03 Pyogen 711.38 Dysenter arthropathy arthritis- arthritis NEC forearm 274.01 Acute gouty arthropathy 696.1 Other psoriasis 711.04 Pyogen 711.4 Bact arthritis- arthritis-hand unspec 274.02 Chr gouty arthropathy 696.2 Parapsoriasis 711.05 Pyogen 711.46 Bact arthritis- w/o tophi arthritis-pelvis l/leg 274.03 Chr gouty arthropathy w 696.3 Pityriasis rosea 711.06 Pyogen 711.5 Viral arthritis- tophi arthritis-l/leg unspec 274.1 Gouty nephropathy NOS 696.4 Pityriasis rubra 711.07 Pyogen 711.55 Viral arthritis- pilaris arthritis-ankle pelvis 274.11 Uric acid nephrolithiasis 696.5 Pityriasis NEC & 711.08 -

Total Knee Arthroplasty in Hemophiliacs: Gains in Range of Motion Realized Beyond Twelve Months Postoperatively Atul F
Original Article Clinics in Orthopedic Surgery 2012;4:121-128 • http://dx.doi.org/10.4055/cios.2012.4.2.121 Total Knee Arthroplasty in Hemophiliacs: Gains in Range of Motion Realized beyond Twelve Months Postoperatively Atul F. Kamath, MD, John G. Horneff , MD, Angela Forsyth, DPT*,†, Valdet Nikci, BS‡, Charles L. Nelson, MD‡ Departments of Orthopaedic Surgery, *Physical Th erapy, †Hematology & Oncology, Hospital of the University of Pennsylvania, ‡Department of Orthopaedic Surgery, Penn Presbyterian Medical Center, Philadelphia, PA, USA Background: Hemophiliacs have extrinsic tightness from quadriceps and fl exion contractures. We sought to examine the effect of a focused physical therapy regimen geared to hemophilic total knee arthroplasty. Methods: Twenty-four knees undergoing intensive hemophiliac-specifi c physical therapy after total knee arthroplasty, at an aver- age age of 46 years, were followed to an average 50 months. Results: For all patients, fl exion contracture improved from −10.5 degrees preoperatively to −5.1 degrees at fi nal follow-up (p = 0.02). Knees with preoperative fl exion less than 90 degrees were compared to knees with preoperative fl exion greater than 90 degrees. Patients with preoperative fl exion less than 90 degrees experienced improved fl exion (p = 0.02), along with improved arc range of motion (ROM) and decreased fl exion contracture. For those patients with specifi c twelve-month and fi nal follow-up data points, there was a signifi cant gain in fl exion between twelve months and fi nal follow-up (p = 0.02). Conclusions: Hemophiliacs with the poorest fl exion benefi ted most from focused quadriceps stretching to a more functional length, with gains not usually seen in the osteoarthritic population. -

Management of Rhabdomyolysis Complicating Traditional Bone Setters Treatment of Fracture
Volume : 4 | Issue : 5 | May 2015 ISSN - 2250-1991 Research Paper Medical Science Management of Rhabdomyolysis Complicating Traditional Bone Setters Treatment of Fracture Enemudo RE AIM: To highlight the complications of rhabdomyolysis caused by the use of tight splint for the treatment of humeral and femoral fractures by traditional bone setter in Delta State, Nigeria. PATIENTS AND METHODS: A retrospective study of patients treated for rhabdomyolysis complicating traditional bone setter treatment of humeral and femoral fractures with tight splint in DELSUTH from August 2012 to December2014. Inclusion criterion was those with rhabdomyolysis caused by TBS treatment of humeral and femoral fracture with tight splint. Exclusion criteria were patients with ischemic gangrene, Volkmann ischemic contracture (VIC), sickle cell and diabetic mellitus patients. Investigations done were limb x-ray, electrocardiography, chest x-ray, serum electrolyte, urea and creatinine, urinalysis with dip-stick test, creatine kinase assay and serum calcium. Treatment protocol used was fluid resuscitation with normal saline, frusemide + mannitol-alkaline diuresis. RESULTS: A total of 6 patients were seen in the study. 4 males and 2 female with M:F ratio of 2:1. The age range of patients ABSTRACT seen was 36-77 years (mean=54.3years). Five patients used the treatment protocol and survived while one did not use the protocol and eventually died because the diagnosis of rhabdomyolysis was not made on time. CONCLUSION: Rhabdomyolysis is a fatal complication of reperfusion injury of muscles following release of the very tight splint used by TBS for the treatment of limb fractures. A good knowledge of the mode of presentation of the patients and necessary investigations plus the immediate commencement of treatment or amputation of the affected limb will avert the associated mortality from cardiac arrest and acute renal failure. -

Dupuytren's Contracture
n interview Dupuytren’s Contracture Steven Beldner, MD In this issue of ORTHOPEDICS, Dr Steven Beldner discusses Dupuy- tren’s contracture and the available nonsurgical and surgical treat- ments. among northern Europeans and in regions that were populated by Viking conquest. Because its expression is increased in diabe- tes mellitus, some argue that it is metabolic. Because its expres- sion is increased in human immunodeficiency infection, some argue that it is associated with the immune system. Because its expression is increased with hepatic disease or administration of phenytoin, some argue that it is associated with the cytochrome P450 system. Many patients report that it started after trauma or What is Dupuytren’s contracture? is accentuated by physical tension placed on the tissue. There- Dupuytren’s contracture is a fibroproliferative condition in fore, some argue that this is the cause. Most agree that Dupuy- which normal collagen is placed in abnormal amounts. It has tren’s contracture has a multifactorial etiology. different names depending on location. When in the feet, it is re- ferred to as Ledderhose disease. When on the penis, it is referred What are the symptoms of Dupuytren’s contracture? to as Peyronie’s disease. When on the back of the knuckles, it is Dupuytren’s contracture is a painless condition. In the early called Garrod’s nodules. Under the microscope, a normal cell phases, a small area of thickening, usually on the ulnar side of called the myofibroblast that is producing normal collagen in the hand in the palm, may be noted. As it progresses into cords, abnormal amounts is seen. -

Modern Cardiac Surgery Modern Cardiac Surgery
Modern Cardiac Surgery Modern Cardiac Surgery Based on the Proceedings of the Eighth Annual Course on Cardiac Surgery, organised by the British Postgraduate Medical Federation Edited by D. B. Longmore Consultant Clinical Physiologist, The National Heart Hospital, London ~~ MTPPRESS LIMITED intl'nllltiOllll/ MediclI/ nlWshers Published by MTP Press Limited Falcon House Lancaster England Copyright © 1978 MTP Press Limited Softcover reprint of the hardcover 1st edition 1978 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without prior permission from the publishers. ISBN-13: 978-94-011-6202-9 e-ISBN-13: 978-94-011-6200-5 DOl: 10.1007/978-94-011-6200-5 Contents List of Contributors x Foreword Xlii SECTION I INVITED LECTURES The National Heart Hospital Surgical Lecture 'Transplantation of the heart' 3 E. B. Stinson and N. E. Shumway The Hammersmith Cardiac Surgery~ Lecture 'Tissue valve grafting'. Aortic valve replacement with autologous fascia lata 19 A. Senning SECTION II THE MITRAL VALVE I. Echocardiography 27 T. A. Traill 2. Mitral valve disease: the case for cardiac catheterization 37 Celia M. Oakley 3. Closed mitral valvotomy 45 W. P. Cleland 4. Open mitral valvotomy 49 S. C. Lennox 5. Reconstruction of the mitral valve 53 M. Paneth 6. Fluid dynamics of prosthetic heart valves 59 D. E. M. Taylor 7. Aortic homograft valves for mitral valve replacement 67 M. Yacoub 8. Echocardiographic studies after mitral valve replacement 75 D. G. Gibson v MODERN CARDIAC SURGERY 9.