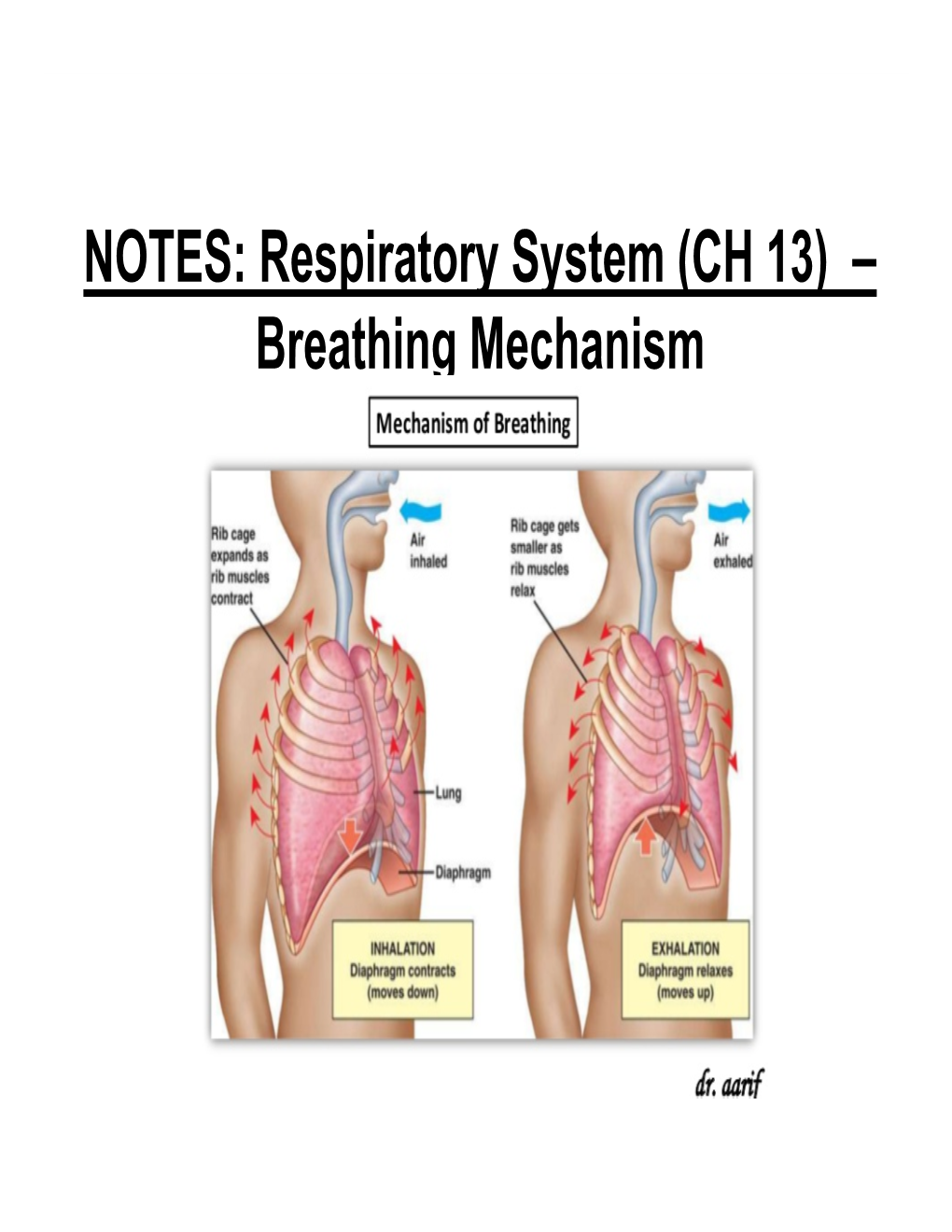
NOTES: Respiratory System (CH 13) – Breathing Mechanism *Changes in the Size of the Thoracic Cavity Accompany INSPIRATION and EXPIRATION
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Physiology H Digestive
2/28/18 Introduction • Provides processes to break down molecules into a state easily used by cells - A disassembly line: Starts at the mouth and ends Digestive System at the anus • Digestive functions are initiated by the parasympathetic division Chapter 29 - Digestion occurs during periods of low activity - Produces more energy than it uses Copyright © 2016 by Elsevier Inc. All rights reserved. 1 Copyright © 2016 by Elsevier Inc. All rights reserved. 2 Anatomy The Digestive System • Oral cavity • Pharynx • Esophagus • Stomach • Small intestine and large intestine • Accessory organs: Pancreas, liver, and gallbladder From Herlihy B: The human body in health and illness, ed 4, St. Louis, 2011, Saunders. Copyright © 2016 by Elsevier Inc. All rights reserved. 3 Copyright © 2016 by Elsevier Inc. All rights reserved. 4 Physiology Gastrointestinal Tract • Ingestion: Taking materials into mouth by • Muscular tube throughout digestive system eating/drinking • Accessory organs and glands secrete • Digestion: Breaking down food into molecules substance to aid in digestion that can be used by the body • GI tract wall has four layers: - Includes mechanical and enzymatic action - Mucosa • Absorption: Simple molecules from the - Submucosa gastrointestinal (GI) tract move into the - Muscle layer: Responsible for peristalsis bloodstream or lymph vessels and then into - Serosa body cells • Defecation: Eliminating indigestible or unabsorbed material from the body Copyright © 2016 by Elsevier Inc. All rights reserved. 5 Copyright © 2016 by Elsevier Inc. All rights reserved. 6 1 2/28/18 Peristalsis Oral Cavity • First portion of GI tract • Contains: - Teeth - Tongue - Openings for salivary glands From Thibodeau GA, Patton KT: Anatomy & physiology, ed 6, St. -

Malignant Pleural Mesothelioma
CLINICAL PRACTICE GUIDELINE LU-009 Version 2 MALIGNANT PLEURAL MESOTHELIOMA Effective Date: December, 2012 The recommendations contained in this guideline are a consensus of the Alberta Provincial Thoracic Malignancies Tumour Team synthesis of currently accepted approaches to management, derived from a review of relevant scientific literature. Clinicians applying these guidelines should, in consultation with the patient, use independent medical judgment in the context of individual clinical circumstances to direct care. CLINICAL PRACTICE GUIDELINE LU-009 Version 2 BACKGROUND Mesothelioma is a rare asbestos-related tumour that arises from mesenchymal cells that are found in the lining of the pleural cavity (Malignant Pleural Mesothelioma; MPM) in 70 to 90 percent of cases, and the peritoneal cavity in 10 to 30 percent of cases.1, 2 Due to the long latency period between exposure and disease, which has been reported to be between 30 and 50 years, most cases of mesothelioma being diagnosed today are the result of asbestos exposure in the 1960s and 1970s.3 Although safety measures for the use of asbestos were adopted in most countries several decades ago, the incidence rates, which are highly age-specific, are still rising, and are expected to peak over the next two decades.4-6 In Canada, the number of men diagnosed with mesothelioma has been steadily increasing over the past 20 years: there were 153 cases reported in 1984 versus 344 cases reported in 2003.3 Mesothelioma is less common in women: there were 78 Canadian women diagnosed with mesothelioma in 2003.3 In the United States, the peak mesothelioma incidence occurred in the early to mid-1990s and has possibly started to decline since then. -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

E Pleura and Lungs
Bailey & Love · Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy · Bailey & Love Bailey & Love · Essential Clinical Anatomy · Bailey & Love · EssentialChapter Clinical4 Anatomy e pleura and lungs • The pleura ............................................................................63 • MCQs .....................................................................................75 • The lungs .............................................................................64 • USMLE MCQs ....................................................................77 • Lymphatic drainage of the thorax ..............................70 • EMQs ......................................................................................77 • Autonomic nervous system ...........................................71 • Applied questions .............................................................78 THE PLEURA reections pass laterally behind the costal margin to reach the 8th rib in the midclavicular line and the 10th rib in the The pleura is a broelastic serous membrane lined by squa- midaxillary line, and along the 12th rib and the paravertebral mous epithelium forming a sac on each side of the chest. Each line (lying over the tips of the transverse processes, about 3 pleural sac is a closed cavity invaginated by a lung. Parietal cm from the midline). pleura lines the chest wall, and visceral (pulmonary) pleura Visceral pleura has no pain bres, but the parietal pleura covers -

Nasal Cavity Trachea Right Main (Primary) Bronchus Left Main (Primary) Bronchus Nostril Oral Cavity Pharynx Larynx Right Lung
Nasal cavity Oral cavity Nostril Pharynx Larynx Trachea Left main Right main (primary) (primary) bronchus bronchus Left lung Right lung Diaphragm © 2018 Pearson Education, Inc. 1 Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, Nasopharynx middle, and inferior) • Pharyngeal tonsil • Nasal meatuses (superior, middle, and inferior) • Opening of pharyngotympanic • Nasal vestibule tube • Nostril • Uvula Hard palate Oropharynx • Palatine tonsil Soft palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Larynx Esophagus • Epiglottis • Thyroid cartilage Trachea • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract © 2018 Pearson Education, Inc. 2 Pharynx • Nasopharynx • Oropharynx • Laryngopharynx (a) Regions of the pharynx © 2018 Pearson Education, Inc. 3 Posterior Mucosa Esophagus Submucosa Trachealis Lumen of Seromucous muscle trachea gland in submucosa Hyaline cartilage Adventitia (a) Anterior © 2018 Pearson Education, Inc. 4 Intercostal muscle Rib Parietal pleura Lung Pleural cavity Trachea Visceral pleura Thymus Apex of lung Left superior lobe Right superior lobe Oblique Horizontal fissure fissure Right middle lobe Left inferior lobe Oblique fissure Right inferior lobe Heart (in pericardial cavity of mediastinum) Diaphragm Base of lung (a) Anterior view. The lungs flank mediastinal structures laterally. © 2018 Pearson Education, Inc. 5 Posterior Vertebra Esophagus (in posterior mediastinum) Root of lung at hilum Right lung • Left main bronchus Parietal pleura • Left pulmonary artery • Left pulmonary vein Visceral pleura Pleural cavity Left lung Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Sternum Anterior mediastinum Anterior (b) Transverse section through the thorax, viewed from above © 2018 Pearson Education, Inc. 6 Alveolar duct Alveoli Respiratory bronchioles Alveolar duct Terminal bronchiole Alveolar sac (a) Diagrammatic view of respiratory bronchioles, alveolar ducts, and alveoli © 2018 Pearson Education, Inc. -

Variations in Dimensions and Shape of Thoracic Cage with Aging: an Anatomical Review
REVIEW ARTICLE Anatomy Journal of Africa, 2014; 3 (2): 346 – 355 VARIATIONS IN DIMENSIONS AND SHAPE OF THORACIC CAGE WITH AGING: AN ANATOMICAL REVIEW ALLWYN JOSHUA, LATHIKA SHETTY, VIDYASHAMBHAVA PARE Correspondence author: S.Allwyn Joshua, Department of Anatomy, KVG Medical College, Sullia- 574327 DK, Karnataka,India. Email: [email protected]. Phone number; 09986380713. Fax number – 08257233408 ABSTRACT The thoracic cage variations in dimensions and proportions are influenced by age, sex and race. The objective of the present review was to describe the age related changes occurring in thoracic wall and its influence on the pattern of respiration in infants, adult and elderly. We had systematically reviewed, compared and analysed many original and review articles related to aging changes in chest wall images and with the aid of radiological findings recorded in a span of four years. We have concluded that alterations in the geometric dimensions of thoracic wall, change in the pattern and mechanism of respiration are influenced not only due to change in the inclination of the rib, curvature of the vertebral column even the position of the sternum plays a pivotal role. Awareness of basic anatomical changes in thoracic wall and respiratory physiology with aging would help clinicians in better understanding, interpretation and to differentiate between normal aging and chest wall deformation. Key words: Thoracic wall; Respiration; Ribs; Sternum; vertebral column INTRODUCTION The thoracic skeleton is an osteocartilaginous cage movement to the volume displacement of the frame around the principal organs of respiration lungs was evaluated by (Agostoni et al,m 1965; and circulation. It is narrow above and broad Grimby et al., 1968; Loring, 1982) for various below, flattened antero-posteriorly and longer human body postures. -

The Digestive System
69 chapter four THE DIGESTIVE SYSTEM THE DIGESTIVE SYSTEM The digestive system is structurally divided into two main parts: a long, winding tube that carries food through its length, and a series of supportive organs outside of the tube. The long tube is called the gastrointestinal (GI) tract. The GI tract extends from the mouth to the anus, and consists of the mouth, or oral cavity, the pharynx, the esophagus, the stomach, the small intestine, and the large intes- tine. It is here that the functions of mechanical digestion, chemical digestion, absorption of nutrients and water, and release of solid waste material take place. The supportive organs that lie outside the GI tract are known as accessory organs, and include the teeth, salivary glands, liver, gallbladder, and pancreas. Because most organs of the digestive system lie within body cavities, you will perform a dissection procedure that exposes the cavities before you begin identifying individual organs. You will also observe the cavities and their associated membranes before proceeding with your study of the digestive system. EXPOSING THE BODY CAVITIES should feel like the wall of a stretched balloon. With your skinned cat on its dorsal side, examine the cutting lines shown in Figure 4.1 and plan 2. Extend the cut laterally in both direc- out your dissection. Note that the numbers tions, roughly 4 inches, still working with indicate the sequence of the cutting procedure. your scissors. Cut in a curved pattern as Palpate the long, bony sternum and the softer, shown in Figure 4.1, which follows the cartilaginous xiphoid process to find the ventral contour of the diaphragm. -

Lab #2: Organs of the Thoracic and Abdominal Cavities. Important: All Dissections of the Thoracic and Abdominal Cavities Will Be Done As a Class
Lab #2: Organs of the thoracic and abdominal cavities. Important: All dissections of the thoracic and abdominal cavities will be done as a class. Do Not get ahead of the class for you may cut into something that we will want to examine later. Goals: Be able to …. Locate and explain the functions of the structures listed below: Neck Region: Abdominal Cavity: thymus gland umbilical chord thyroid gland peritoneum larynx mesenteries trachea liver esophagus stomach thoracic Cavity: spleen right and left pleural cavities small intestine (locate duodenum) right and left lungs pancreas pericardial cavity large intestines heart cecum Thoracic/Abdominal Division: colon diaphragm 13.3 Thoracic and Abdominal Incisions Pp. 164 – 165 Make incisions with class and instructor!!! 13.4 Neck Region, Thoracic Cavity and Abdominal Cavity Pp. 166-170 – Read all introductions, follow the procedures to locate the organs specified and answer all the questions. Pp. 172 – Answer questions #6-8, 11-17, 19 Arrange the organs in order by the way food travels through them: Stomach, esophagus, large intestines, mouth, small intestines, anus, rectum The inhalation of a breath of travels through several organs. Put the following organs in their proper order: Bronchi, nasal passages, bronchioles, larynx, pharynx, alveoli, trachea II. Respiration and Digestion Stations Goals: After this lab you should be able to………….. 1. Describe the appearance of villi and explain how the structure of villi supports their function. 2. Describe the internal structure of the lungs and explain the process of gas exchange. 3. Explain the difference in appearance and function between healthy alveoli and diseased alveoli. -

Human Anatomy and Physiology
LECTURE NOTES For Nursing Students Human Anatomy and Physiology Nega Assefa Alemaya University Yosief Tsige Jimma University In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education 2003 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2003 by Nega Assefa and Yosief Tsige All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. Human Anatomy and Physiology Preface There is a shortage in Ethiopia of teaching / learning material in the area of anatomy and physicalogy for nurses. The Carter Center EPHTI appreciating the problem and promoted the development of this lecture note that could help both the teachers and students. -

Study 1: Effect of Saliva on B2T
Stability of b2-transferrin and b-trace protein Lyn Boscato Chemical Pathology, St Vincent’s Hospital, Sydney, Australia. [email protected]; Introduction and Aim Study 1: Effect of saliva on B2T b2-transferrin (B2T) and b-trace protein (BTP) are useful markers for SUSPECTED SAMPLE PROBLEM the diagnosis of CSF leakage. A sample received for routine investigation of a suspected CSF Specimens received for analysis are often heavily contaminated with leak was negative for BTP but the transferrin isoform pattern other substances (eg blood, serous fluid, saliva, bacteria, mucus) and suggested CSF presence. Sample was an oral fluid collection so stored under non-ideal conditions (not frozen, large container, very small sample volume, on swabs). sialidase presence was suspected as the oral cavity can have a high bacterial load The aim of this study was to investigate the stability of B2T and BTP in 1 2 3 4 5 the presence of potential contaminants. 1 - CSF 4 - serum+ saliva STUDY 2 - CSF + saliva 5 - serum To determine if saliva contains sialidase 3 - saliva • • Saliva collected by passive drooling and microfuged to remove Figure 1. Transferrin isoforms detected following particulates. Methods IEF- western blotting for CSF and serum incubated • Equal volumes of saliva and serum or CSF were incubated with and without saliva. overnight at RT • Transferrin isoforms detected STUDIES Investigation of the stability of B2T and BTP incubated in the presence of a. saliva as a source of sialidase (enzyme which removes sialic acid from glycoproteins. Normally arises from bacterial or viral Study 2: Stability of B2T and BTP sources). -
2.05 Remember the Structures of the Respiratory System 2.05 Remember the Structures of the Respiratory System
2.05 Remember the structures of the respiratory system 2.05 Remember the structures of the respiratory system Essential question What are the structures of the respiratory system? 2.05 Remember the structures of the respiratory system 2 Structures of the respiratory system Upper Respiratory System Nose Sinuses Pharynx Epiglottis Larynx Lower Respiratory System Trachea Lungs 2.05 Remember the structures of the respiratory system 3 Structures of the Upper Respiratory System Nose Nasal cavity – space behind the nose Vestibular region Olfactory region Respiratory region Nasal septum – cartilage that divides the nose into right and left sides Turbinates – scroll-like bones in the respiratory region Cilia – nose hairs 2.05 Remember the structures of the respiratory system 4 Structures of the Upper Respiratory System Sinuses - Cavities in the skull. Ducts connect sinuses to the nasal cavity Lined with mucous membrane to warm and moisten the air Provide resonance to the voice 2.05 Remember the structures of the respiratory system 5 Structures of the Upper Respiratory System Pharynx Throat Nasopharynx Oropharynx Laryngopharynx About 5” long 2.05 Remember the structures of the respiratory system 6 Structures of the Upper Respiratory System Epiglottis A flap or lid that closes over the opening to the larynx when food is swallowed 2.05 Remember the structures of the respiratory system 7 Structures of the Upper Respiratory System Larynx Voice Box Triangular chamber below pharynx Within the larynx are vocal cords, the glottis Also called the Adam’s Apple 2.05 Remember the structures of the respiratory system 8 Structures of the Lower Respiratory System Trachea Windpipe Approximately 4 ½” long The walls are composed of alternate bands of membrane and C-shaped rings of hyaline cartilage.