Whenunexpected Compl Cat Onsar Se Dur Ngsurgeryò
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Uterine Rupture During Subsequent
ISSN: 2474-1353 Nishida et al. Int J Womens Health Wellness 2018, 4:070 DOI: 10.23937/2474-1353/1510070 Volume 4 | Issue 1 International Journal of Open Access Women’s Health and Wellness RESEARCH ARTICLE Uterine Rupture during Subsequent Pregnancy following Adeno- myomectomy - Report of Five Cases and Proposal for Prevention Masato Nishida1*, Yasuo Otsubo1, Yuko Arai1, Ryota Ichikawa1, Yuzuru Kondo2, Hiroya Itagaki1 and Miyako Sakanaka1 1Department of Obstetrics and Gynecology, National Hospital Organization, Kasumigaura Medical Center, Japan 2Department of Pathology, National Hospital Organization, Kasumigaura Medical Center, Tsuchiura, Japan *Corresponding author: Masato Nishida, Department of Obstetrics and Gynecology, National Hospital Organization, Kasumigaura Medical Center, 2-7-14 Shimotakatsu, Tsuchiura, Ibaraki, 300-8585, Japan, Check for Tel: +81-29-822-5050, Fax: +81-29-824-0494, E-mail: [email protected] updates Abstract taining the possibility of conception following surgery Purpose: The risk of uterine rupture is a major concern for [2,3]. Various perinatal complications are associated women who become pregnant after undergoing an adeno- with an adenomyomectomy [4], thus consensus for its myomectomy. The aim of this study was to investigate the indications among obstetricians has not been obtained. mechanism of uterine rupture and improve the surgical pro- Notably, uterine rupture is a lethal condition for both cedure used for prevention. mother and fetus [5]. Material and methods: Five patients who experienced uterine rupture during subsequent pregnancy after under- It is clinically important to investigate the mecha- going an adenomyomectomy performed with an open lapa- nism of uterine rupture in affected patients, and also rotomy were retrospectively investigated. -

FEMALE REPRODUCTIVE SYSTEM Female Reproduc�Ve System
Human Anatomy Unit 3 FEMALE REPRODUCTIVE SYSTEM Female Reproducve System • Gonads = ovaries – almond shaped – flank the uterus on either side – aached to the uterus and body wall by ligaments • Gametes = oocytes – released from the ovary during ovulaon – Develop within ovarian follicles Ligaments • Broad ligament – Aaches to walls and floor of pelvic cavity – Connuous with parietal peritoneum • Round ligament – Perpendicular to broad ligament • Ovarian ligament – Lateral surface of uterus ‐ ‐> medial surface of ovary • Suspensory ligament – Lateral surface of ovary ‐ ‐> pelvic wall Ovarian Follicles • Layers of epithelial cells surrounding ova • Primordial follicle – most immature of follicles • Primary follicle – single layer of follicular (granulosa) cells • Secondary – more than one layer and growing cavies • Graafian – Fluid filled antrum – ovum supported by many layers of follicular cells – Ovum surrounded by corona radiata Ovarian Follicles Corpus Luteum • Ovulaon releases the oocyte with the corona radiata • Leaves behind the rest of the Graafian follicle • Follicle becomes corpus luteum • Connues to secrete hormones to support possible pregnancy unl placenta becomes secretory or no implantaon • Becomes corpus albicans when no longer funconal Corpus Luteum and Corpus Albicans Uterine (Fallopian) Tubes • Ciliated tubes – Passage of the ovum to the uterus and – Passage of sperm toward the ovum • Fimbriae – finger like projecons that cover the ovary and sway, drawing the ovum inside aer ovulaon The Uterus • Muscular, hollow organ – supports -
CST-On-Demand-Binder.Pdf
Zander Perioperative Education Zander CST Exam Preparation Course Zander Perioperative Education Certification Preparation for CNOR, CAPA-CPAN, CST and CBSPD Wendy Zander MSN/Ed, RN, CNOR [email protected] Test Taking Strategies Objectives: 1. Apply Test Taking Strategies for the CST exam 2. Create a Personal Study Plan 3. Eligibility • Registering for the exam • Exam Format • Time Management • Test Taking Strategies Eligibility • Current or previously Certified Surgical Technologist (CST) ▫ Evidence of CST Certification • Graduate of a surgical technology program accredited by CAAHEP ▫ Evidence of proof of graduation • Graduate of a surgical technology accredited by ABHES ▫ Evidence of proof of graduation www.periop-ed.com 1 Zander Perioperative Education Military Eligible • A graduate of a military training program in surgical technology is always eligible whether it was before, during or after having CAAHEP accreditation. ▫ a copy of your DD214 (must state location of the base where program was completed), ▫ a copy of your graduation certificate from the surgical technology training program ▫ a smart transcript Accelerated Alternate Delivery (AAD) Pathway • Have on-the-job training in surgical technology • Are a graduate from a surgical technology program that did not hold CAAHEP accreditation during your enrollment CST Testing Fees First Time Test Takers Exam Fee (AST Members) Exam Fee (Non Members) $190 $290 Current or Previous Certified Surgical Technologist Renewing First Time Test Takers Certification by Examination Exam Fee -

Aspiration System and Suction Tip Yankauer
ILE R S E T E T R S I E L Mechanical Irrigation Kits: Physiodispenser and Piezoelectric Surgery 32.F0106.00 Irrigation set 1/2Y Aseptico Aeu 1000 -70/V, Aseptico Aeu 1070-70V 10 pcs 32.F0090.00 Irrigation set 1/2Y Dental Unit Sirona 10 pcs 32.F0019.00 Irrigation set 1/2Y ATR Plus /3000 /5000 10 pcs 32.F0090.00 32.F0106.00 Aspiration System and Suction Tip Yankauer The surgical aspirator with Yankauer suction tip is suitable for all those surgical operations, where an accurate aspiration is needed, so as not to impair the visibility of the operation field. The special nozzles that are placed all around the apical perimeter of the suction tip avoid any accidental suction of small edges of tissue during gingivoplasty. The aspirator is made of medical grade transparent PVC, so as not to absorb the light of shadow-free operating lamps obscuring the surgical site. It is supplied with bending-resistant flexible connectors. Surgical aspirator, 2.50, m with Yankauer suction tip and aspiration control 32.F2044.00 PVC 10 pcs system. (each pack contains 1 adapter Adat. 05) 32.F6361.00 Yankauer sterile suction tip (tip length: 24,5 cm) with aspiration control system PVC 10 pcs 1 Omnia® PTFE Sutures - Black Needle Omnia surgical PTFE sutures are ideal for any implant, periodontal and bone graft surgery where the usage of a monofilament suture with low bacterial adhesion is recommended. Omnia PTFE sutures are soft, biologi- cally inert and chemically non reactive. Compared to other monofilament synthetic sutures, this material is highly tolerated in the oral cavity. -

4 Lecture Uterus Gross Anatomy
Body: major portion Uterine body Fundus: rounded superior region Fundus Isthmus: narrowed inferior region Lumen of uterus Cervix: narrow neck (cavity) of uterus Wall of uterus Body of uterus • Endometrium • Myometrium • Perimetrium Isthmus Cervical canal Vagina Cervix Posterior view © 2016 Pearson Education, Inc. Uterus: ligaments (woman) The ligaments of the uterus are 10 in number: one anterior (vesicouterine fold of peritoneum); one posterior (rectouterine fold of peritoneum); two lateral or broad; two uterosacral; two cardinal (lateral cervical) ligaments; and two round ligaments. Anterior ligament: consists of the vesicouterine fold of peritoneum, which is reflected on to the bladder from the front of the uterus Posterior ligament: consists of the rectouterine fold of peritoneum, which is reflected from cervix on to the front of the rectum. Uterosacral ligaments: secure uterus to sacrum Suspensory ligament of ovary Peritoneum Uterine tube Ovary Uterosacral ligament Uterus Rectouterine Round ligament pouch Vesicouterine pouch Rectum Urinary bladder Pubic symphysis Mons pubis Cervix Urethra Clitoris Vagina External urethral orifice Anus © 2016 Pearson Education, Inc. Domestic animals Rectum rectouterine fold vesicouterine fold Bladder cardinal (lateral cervical) ligaments: from cervix and superior vagina to pelvic lateral walls Suspensory ligament of Uterine ovary (fallopian) tube Fundus Lumen of uterus Ovarian (cavity) blood vessels of uterus Uterine tube Broad ligament Ovary • Ampulla • Isthmus • Mesosalpinx • Infundibulum • Mesovarium -

Chargemaster
Charge Code Description Price Medicare CPT 400481 OR 481 TO 540 MIN 9100 SURG 400777 SUTURES-RUN 92 400778 SUTURE-POP OFF 128 400779 SUTURE-REEL 33 400780 SUTURE-TIES 84 440002 STALEVO 150 11.2 3000817 PNEUM VACCINE ADMINI 57 G0009 3000819 CA SCREEN; PELVIC/BR 103 G0101 3000823 COLORECTAL SCR SCOPE 1030 G0105 3001087 APPLICATION FOREARM 200 29085 3001104 TECH COMP EXC DEB 42 376 11042 3001297 HIPPS 0 MANUL 3001740 CENTRAL VENOUS LINE 1500 36556 3001741 TECH COMP REPLACMENT 1500 36580 3001742 TECH COMP REMOVAL HI 1000 36589 3001745 TECH COMP GASTROSTOM 325 3001746 TECH COMP I&D SCROTA 1700 55100 3001913 PRIVATE ROOM W/BATH 982 3002874 SEMI-PRIVATE 960 3002879 TECH COMP TUBE THORA 900 32551 3002882 TECH COMP REPLACEMEN 1500 36580 3003298 CVP TECHNICAL COMPON 1500 36556 3003882 ADMIN BLD/BLD PRDUCT 565 36430 3004250 TECH COMP INS ART LN 515 36245 3004251 CVP TECHNICAL COMPON 1500 36556 3004253 TECH COMP REPLACEMEN 1500 36580 3004256 TECH COMP BX 45100 3300 45100 3004259 TECH COMP PARACENTES 815 49082 3004261 INSERTION TEMP BLADD 200 51702 3004263 DILATION URETHRA SUB 275 53621 3004264 TECH COMP DILATION U 150 53661 3004538 NURSERY/SICK BABY 450 3004850 TREATMENT ROOM LVL 1 150 99211 3004853 TREATMENT RM LVL 3 250 99213 3004995 TECH COMP PARA REPEA 815 49082 3005022 OBS DIRECT ADMIT 1ST 600 G0379 3005110 SWING BED 441 3005209 OBSERV RM. EACH HR 50 G0378 3005845 INJ INTRA-A THERAPEU 200 96373 3005933 IMMUN ADMIN ONE VACC 53 90471 3005938 IV INF HYDRATION INI 215 96360 3005939 IV INF HYDRATION EAC 65 96361 3005940 IV INF THER PROPH DI 300 96365 -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Uterine Blood Flow and Perfusion in Mares with Uterine Cysts
REPRODUCTIONRESEARCH Uterine blood flow and perfusion in mares with uterine cysts: effect of the size of the cystic area and age J C Ferreira1, E L Gastal2 and O J Ginther1,2 1Eutheria Foundation, Cross Plains, Wisconsin 53528, USA and 2Department of Pathobiological Sciences, School of Veterinary Medicine, University of Wisconsin, 1656 Linden Drive, Madison, Wisconsin 53706, USA Correspondence should be addressed to E L Gastal; Email: [email protected] Abstract Transrectal color and power Doppler ultrasonography was used to study uterine blood flow and perfusion in mares with and without uterine cysts. Vascular perfusion of the uterus and blood flow velocities, vascular perfusion, diameter,circumference, and area of a cross section of the mesometrial attachment were evaluated. To study the effect of internal cysts, two matched groups (cystic and control, nZ21 mares/group) were used. Uterine vascular perfusion in mares with cysts was less (P!0.0001) in the cystic than the noncystic region and less (P!0.0009) than that for controls. Mares with cysts had lower (P!0.04) pulsatility index (PI) and greater end diastolic velocity (EDV; P!0.03) and time-averaged maximum velocity (TAMV; P!0.05) of the mesometrial vessels than the controls. To study the effect of the size of internal uterine cystic area, paired mares were arranged in four groups (nZ8–11/group): small uterine cystic area (%275 mm2) versus controls and large uterine cystic area (O410 mm2) versus controls. A small uterine cystic area did not affect uterine hemodynamics. Mares with large uterine cystic area had lower PI (P!0.05) and greater peak systolic velocity (P%0.05), EDV (P!0.009), and TAMV (P!0.005). -
Study Guide Anatomy Second Year Mbbs Session 2018-23
STUDY GUIDE ANATOMY SECOND YEAR MBBS SESSION 2018-23 INTRODUCTION Human anatomy is the branch of science concerned with their bodily structure. It deals with the way the parts of human, from molecules to bones, interact to form a functional unit. It is studied at three levels, macroanatomy or gross anatomy, microanatomy or histology, and developmental anatomy or embryology. Anatomy is an important lesson for medical students worldwide. Many of the clinical specialists consider having enough knowledge ofanatomy a prerequisite for performing safe and competent interventions in medicine. Learning anatomy practically and with clinical approach is necessary for medical students for flawless medical practice..Knowing the importance and clinical uses of anatomy, on the other hand, could help students improve their clinical acumen. TARGET 2nd year MBBS STUDENTS COURSE TO BE 1. Gross Anatomy: STUDIED IN a. Abdomen, Pelvis & Perineum, SECOND YEAR b. Head & Neck MBBS c. Neuroanatomy 2. Special Histology 3. Special Embryology COURSE TITLE ABDOMEN, PELVIS & PERINEUM DURATION 12 weeks OUT COMES At the end of the module, the students will be able to: • Explain the normal and abnormal gross and microscopic structures related to the abdomen, pelvis & perineal regions. OBJECTIVES At the end of the course student must be able to: 1: Anterolateral abdominal Walls • Give overview about walls, cavities, regions, and planes of anterolateral abdominal wall • Describe the layers, attachments & extent of fascia of the anterolateral abdominal wall • Enumerate muscles -
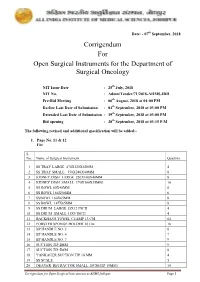
Corrigendum for Open Surgical Instruments for the Department Of
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST. -

Alekls0201b.Pdf
Female genital system Miloš Grim Institute of Anatomy, First Faculty of Medicine, Summer semester 2017 / 2018 Female genital system Internal genital organs Ovary, Uterine tube- Salpinx, Fallopian tube, Uterus - Metra, Hystera, Vagina, colpos External genital organs Pudendum- vulva, cunnus Mons pubis Labium majus Pudendal cleft Labium minus Vestibule Bulb of vestibule Clitoris MRI of female pelvis in sagittal plane Female pelvis in sagittal plane Internal genital organs of female genital system Ovary, Uterine tube, Uterus, Broad ligament of uterus, Round lig. of uterus Anteflexion, anteversion of uterus Transverse section through the lumbar region of a 6-week embryo, colonization of primitive gonade by primordial germ cells Primordial germ cells migrate into gonads from the yolk sac Differentiation of indifferent gonads into ovary and testis Ovary: ovarian follicles Testis: seminiferous tubules, tunica albuginea Development of broad ligament of uterus from urogenital ridge Development of uterine tube, uterus and part of vagina from paramesonephric (Mullerian) duct Development of position of female internal genital organs, ureter Broad ligament of uterus Transverse section of female pelvis Parametrium Supporting apparatus of uterus, cardinal lig. (broad ligament) round ligament pubocervical lig. recto-uterine lig. Descent of ovary. Development of uterine tube , uterus and part of vagina from paramesonephric (Mullerian) duct External genital organs develop from: genital eminence, genital folds, genital ridges and urogenital sinus ureter Broad ligament of uterus Transverse section of female pelvis Ovary (posterior view) Tubal + uterine extremity, Medial + lateral surface Free + mesovarian border, Mesovarium, Uteroovaric lig., Suspensory lig. of ovary, Mesosalpinx, Mesometrium Ovary, uterine tube, fimbrie of the tube, fundus of uterus Ovaric fossa between internal nd external iliac artery Sagittal section of plica lata uteri (broad lig.