CST-On-Demand-Binder.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Minimal Endoscope-Assisted Thyroidectomy Through a Retroauricular Approach: an Evolving Solo Surgery Technique
ORIGINAL ARTICLE Minimal Endoscope-assisted Thyroidectomy Through a Retroauricular Approach: An Evolving Solo Surgery Technique Myung Jin Ban, MD,*w Jae Won Chang, MD,z Won Shik Kim, MD,y Hyung Kwon Byeon, MD, PhD,y Yoon Woo Koh, MD, PhD,y and Jae Hong Park, MD, PhD* (RA), or transoral approach.1–5 Endoscopic thyroidectomy Abstract: This study aimed to evaluate the feasibility and efficacy of through an RA approach is an especially excellent choice minimal endoscope-assisted thyroidectomy (MEAT) through a for head and neck surgeons because of their familiarity with retroauricular (RA) approach. Most of the thyroidectomy oper- the direction of the approach, the short distance to the ative time was accounted for by direct visualization through the thyroid gland, and a good cosmetic outcome without the RA window, minimizing interference between surgical instruments. 6 Endoscope use was minimized and limited to critical surgical need for additional incisions. aspects, including preservation of the recurrent laryngeal nerve and Despite the advantages of the RA approach, funda- parathyroid glands. The recurrent laryngeal nerve was neuro- mental limitations of endoscopic surgery still exist, includ- monitored throughout the procedure. MEAT through an RA ing a narrow operative field that restricts the free movement approach was performed in 8 patients with papillary thyroid car- of instruments. Gas insufflation, an additional incision for cinoma (mean tumor size, 1.2 ± 0.5 cm). The mean patient age was the endoscope port, robotic arm assistance, and a flexible 41.1 ± 7.5 years. The endoscopic operating time was endoscope holder for solo surgery have all been used to 19 ± 3.4 minutes, and no postoperative hematoma, seroma, or overcome this limitation.3,7,8 vocal cord paralysis was observed. -

Aspiration System and Suction Tip Yankauer
ILE R S E T E T R S I E L Mechanical Irrigation Kits: Physiodispenser and Piezoelectric Surgery 32.F0106.00 Irrigation set 1/2Y Aseptico Aeu 1000 -70/V, Aseptico Aeu 1070-70V 10 pcs 32.F0090.00 Irrigation set 1/2Y Dental Unit Sirona 10 pcs 32.F0019.00 Irrigation set 1/2Y ATR Plus /3000 /5000 10 pcs 32.F0090.00 32.F0106.00 Aspiration System and Suction Tip Yankauer The surgical aspirator with Yankauer suction tip is suitable for all those surgical operations, where an accurate aspiration is needed, so as not to impair the visibility of the operation field. The special nozzles that are placed all around the apical perimeter of the suction tip avoid any accidental suction of small edges of tissue during gingivoplasty. The aspirator is made of medical grade transparent PVC, so as not to absorb the light of shadow-free operating lamps obscuring the surgical site. It is supplied with bending-resistant flexible connectors. Surgical aspirator, 2.50, m with Yankauer suction tip and aspiration control 32.F2044.00 PVC 10 pcs system. (each pack contains 1 adapter Adat. 05) 32.F6361.00 Yankauer sterile suction tip (tip length: 24,5 cm) with aspiration control system PVC 10 pcs 1 Omnia® PTFE Sutures - Black Needle Omnia surgical PTFE sutures are ideal for any implant, periodontal and bone graft surgery where the usage of a monofilament suture with low bacterial adhesion is recommended. Omnia PTFE sutures are soft, biologi- cally inert and chemically non reactive. Compared to other monofilament synthetic sutures, this material is highly tolerated in the oral cavity. -

Chargemaster
Charge Code Description Price Medicare CPT 400481 OR 481 TO 540 MIN 9100 SURG 400777 SUTURES-RUN 92 400778 SUTURE-POP OFF 128 400779 SUTURE-REEL 33 400780 SUTURE-TIES 84 440002 STALEVO 150 11.2 3000817 PNEUM VACCINE ADMINI 57 G0009 3000819 CA SCREEN; PELVIC/BR 103 G0101 3000823 COLORECTAL SCR SCOPE 1030 G0105 3001087 APPLICATION FOREARM 200 29085 3001104 TECH COMP EXC DEB 42 376 11042 3001297 HIPPS 0 MANUL 3001740 CENTRAL VENOUS LINE 1500 36556 3001741 TECH COMP REPLACMENT 1500 36580 3001742 TECH COMP REMOVAL HI 1000 36589 3001745 TECH COMP GASTROSTOM 325 3001746 TECH COMP I&D SCROTA 1700 55100 3001913 PRIVATE ROOM W/BATH 982 3002874 SEMI-PRIVATE 960 3002879 TECH COMP TUBE THORA 900 32551 3002882 TECH COMP REPLACEMEN 1500 36580 3003298 CVP TECHNICAL COMPON 1500 36556 3003882 ADMIN BLD/BLD PRDUCT 565 36430 3004250 TECH COMP INS ART LN 515 36245 3004251 CVP TECHNICAL COMPON 1500 36556 3004253 TECH COMP REPLACEMEN 1500 36580 3004256 TECH COMP BX 45100 3300 45100 3004259 TECH COMP PARACENTES 815 49082 3004261 INSERTION TEMP BLADD 200 51702 3004263 DILATION URETHRA SUB 275 53621 3004264 TECH COMP DILATION U 150 53661 3004538 NURSERY/SICK BABY 450 3004850 TREATMENT ROOM LVL 1 150 99211 3004853 TREATMENT RM LVL 3 250 99213 3004995 TECH COMP PARA REPEA 815 49082 3005022 OBS DIRECT ADMIT 1ST 600 G0379 3005110 SWING BED 441 3005209 OBSERV RM. EACH HR 50 G0378 3005845 INJ INTRA-A THERAPEU 200 96373 3005933 IMMUN ADMIN ONE VACC 53 90471 3005938 IV INF HYDRATION INI 215 96360 3005939 IV INF HYDRATION EAC 65 96361 3005940 IV INF THER PROPH DI 300 96365 -

Rapid HTA Report Ultrasonic Energy Devices for Surgery July 2014
Rapid HTA report 1 Ultrasonic energy devices for surgery July 2014 1 This report should be cited as: Migliore A, Corio M, Perrini MR, Rivoiro C, Jefferson T. Ultrasonic energy devices for surgery: rapid HTA report. Agenas, Agenzia nazionale per i servizi sanitari regionali. Rome, July 2014. Contributions Authors Antonio Migliore, Mirella Corio, Maria Rosaria Perrini, Chiara Rivoiro, and Tom Jefferson Agenas, Agenzia nazionale per i servizi sanitari regionali, Area Funzionale Innovazione, Sperimentazione e Sviluppo, via Puglie 23, 00187 Rome (Italy) Corresponding author Antonio Migliore, MSc ([email protected]) Clinical experts Mario Alessiani, MD FACS Division of General Surgery, Varzi Hospital, University of Pavia (Italy) Marco Filauro, MD Division of General and Hepatobiliopancreatic Surgery, Galliera Hospital, Genova (Italy) Invited reviewers Chuong Ho, MD MSc Canadian Agency for Drugs and Technologies in Health (CADTH), Ottawa (Canada) Björn Fahlgren, MSc 2 Comité d’évaluation des technologies de santé (CEDIT), Paris (France) Acknowledgements Authors would like to thank Marina Cerbo (Agenas) and Simona Paone (Agenas), for the valuable help in reviewing the research protocol and the first draft of the report, Patrizia Brigoni (Agenas) for performing the systematic literature searches, Fabio Bernardini (Agenas) for his relevant support in retrieving the publications, and Laura Velardi (Agenas) for supporting consultation and analysis of databases. Declaration on the conflict of interest and privacy Authors, Clinical expert and External Reviewers declare that they do not receive benefits or harms from the publication of this report. None of the authors have or have held shares, consultancies or personal relationships with any of the producers of the devices assessed in this document. -
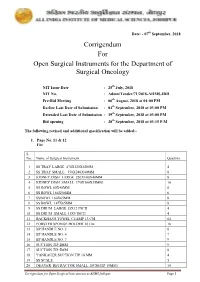
Corrigendum for Open Surgical Instruments for the Department Of
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST. -

Case Report Management of Total Transection of Nasoendotracheal Tube During Lefort I Osteotomy
Hindawi Case Reports in Anesthesiology Volume 2020, Article ID 2097240, 4 pages https://doi.org/10.1155/2020/2097240 Case Report Management of Total Transection of Nasoendotracheal Tube during LeFort I Osteotomy Miles Somers ,1 Peter Tsakiris,1 Peter Isert,2 and Samuel Kim 1 1Department of Oral and Maxillofacial Surgery, Prince of Wales Hospital, Randwick, NSW, Australia 2VMO Anaesthetist, Prince of Wales Private Hospital, Randwick, NSW, Australia Correspondence should be addressed to Miles Somers; [email protected] Received 10 March 2020; Revised 8 August 2020; Accepted 26 October 2020; Published 17 November 2020 Academic Editor: Pavel Michalek Copyright © 2020 Miles Somers et al. *is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Transection of the nasoendotracheal tube during orthognathic surgery is a rare, but life-threatening complication. We present a case of complete nasoendotracheal tube transection during a LeFort 1 osteotomy and discuss appropriate preventative and management techniques. 1. Introduction 2. Case Report Complete transection of the nasoendotracheal tube (NET) A 28-year-old male underwent a 2-piece maxillary osteot- during surgery is rare [1]. However, it poses a potentially life- omy plus right ramus graft for genioplasty. *e aim of the threatening complication that must be managed effectively. surgery was orthognathic correction of a dentoskeletal class *ere are several reported cases in the literature reporting III malocclusion related to hypoplasia of the maxilla sec- both complete [2, 3] and partial transection [4–7]. Maxil- ondary to cleft lip and palate. -

Thoracoscopic Spine Surgery for Decompression and Stabilization of the Anterolateral Thoracolumbar Spine
Neurosurg Focus 19 (6):E4, 2005 Thoracoscopic spine surgery for decompression and stabilization of the anterolateral thoracolumbar spine AMIN AMINI, M.D., M.SC., RUDOLF BEISSE, M.D., AND MEIC H. SCHMIDT, M.D. Department of Neurosurgery, University of Utah, Salt Lake City, Utah; and Department of Trauma Surgery, Berufsgenossenschaftliche Unfallklinik Murnau, Germany The anterior thoracolumbar spine can be exposed via a variety of approaches. Historically, open anterolateral or pos- terolateral approaches have been used to gain access to the anterior thoracolumbar spinal column. Although the expo- sure is excellent, open approaches are associated with significant pain and respiratory problems, substantial blood loss, poor cosmesis, and prolonged hospitalization. With the increasing use of the endoscope in surgical procedures and recent advances in video-assisted thoracoscopic surgery, minimally invasive thoracoscopic spine surgery has been developed to decrease the morbidity associated with open thoracotomy. The purpose of this article is to illustrate the surgical technique of a minimally invasive thoracoscopic approach to the anterolateral thoracolumbar spine and to dis- cuss its potential indications and contraindications in patients with diseases involving the anterior thoracic and lumbar regions. KEY WORDS • endoscopic spinal surgery • thoracoscopy • thoracic spine • lumbar spine • thoracoscopic spinal instrumentation Since the introduction of thoracoscopic surgery by Jaco- Minimal access surgical techniques can potentially de- baeus15 in 1910, the technique has undergone enormous crease spinal access morbidity and speed recovery and advances. With the development of high-quality video im- healing.4,7,16,17 At the University of Utah Medical Center, we aging, small endoscopes, and modified new instruments, have performed 30 thoracoscopic spine surgeries for tho- video-assisted thoracic surgery has become the minimally racolumbar trauma, tumors, and infection. -

2Fde87e0691f6f570e2a63cb3c9
Hindawi Minimally Invasive Surgery Volume 2018, Article ID 4256570, 5 pages https://doi.org/10.1155/2018/4256570 Research Article Challenges and Results of Laparoscopic Splenectomy for Hematological Diseases in a Developing Country Vikal Chandra Shakya ,1 Bikram Byanjankar,1 Rabin Pandit,1 Anang Pangeni,1 Anir Ram Moh Shrestha,1 and Bishesh Poudyal2 1 Department of Surgery, Civil Service Hospital of Nepal, Kathmandu, Nepal 2Clinical Hematology and Bone Marrow Transplant Unit, Department of Medicine, Civil Service Hospital of Nepal, Kathmandu, Nepal Correspondence should be addressed to Vikal Chandra Shakya; [email protected] Received 20 March 2018; Revised 3 July 2018; Accepted 15 July 2018; Published 1 August 2018 Academic Editor: Diego Cuccurullo Copyright © 2018 Vikal Chandra Shakya et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Introduction. Tough, in developed countries, laparoscopy is now a gold standard for splenectomy, we are lacking in this aspect in the eastern world. Splenectomy has mostly been performed by open surgery in our region. Tis is our efort to introduce laparoscopic splenectomy in our country. Methods. Tis is a retrospective cohort study done in patients presenting to hematology and surgery department of our hospital who underwent laparoscopic splenectomy for hematological diseases from January 2013 to December 2016. Results. Tere were 50 patients (38 females, 12 males). Te diagnoses were idiopathic thrombocytopenic purpura in 31, (steroid/azathioprine-resistant, steroid dependent), hereditary spherocytosis in 9, alpha-thalassemia in 3, beta-thalassemia in 2, autoimmune hemolytic anemia in 4, and isolated splenic tuberculosis in 1. -

Chirurgische Instrumente Surgical Instruments
CHIRURGISCHE INSTRUMENTE SURGICAL INSTRUMENTS SURGICAL INSTRUMENTS Percussion Hammers & Aesthesiometers 01-103 01-102 DEJERINE 01-104 DEJERINE With Needle TAYLOR Size: 200 mm Size: 210 mm Size: 195 mm 01-101 ½ ½ ½ TROEMNER Size: 245 mm ½ 01-109 01-106 01-107 WARTENBERG BUCK RABINER Pinwheal For 01-105 With Needle With Needle 01-108 Neurological BERLINER And Brush And Brush ALY Examination Size: 200 mm Size: 180 mm Size: 255 mm Size: 190 mm Size: 185 mm ½ ½ ½ ½ ½ Page 1 2 Stethoscopes 01-112 01-110 01-111 BOWLES PINARD (Aluminum) aus Holz (Wooden) Stethoscope Size: 155 mm Size: 145 mm With Diaphragm ½ ½ 01-113 01-114 ANESTOPHON FORD-BOWLES Duel Chest Piece 01-115 With Two Outlets BOWLES Page 2 3 Head Mirrors & Head Bands 01-116 01-117 ZIEGLER mm ZIEGLER mm Head mirror only Head mirror only with rubber coating with metal coating 01-118 01-120 ZIEGLER MURPHY Head band of plastic black Head band of celluloid, white 01-119 ZIEGLER Head band of plastic white 01-121 01-122 Head band of plastic, Head mirror with black white, soft pattern plastic head band. Page 3 4 Head Light 01-123 CLAR Head light, 6 volt, with adjustable joint, white celluloid head band, cord with plugs for transformer 01-124 White celluloid head band, only, for 01-125 Spare mirror only, for 01-126 spare bulb 01-127 CLAR Head light, 6 volt, with adjustable joint, white celluloid head band, with foam rubber pad and cord with plugs for transformer 01-128 White celluloid head band, only, for head light 01-129 mirror only, for head light 01-130 spare foam rubber pad, for head band -

Penoscrotal Three-Piece Inflatable Penile Prosthesis Placement: Surgical Technique
Editorial Page 1 of 6 Penoscrotal three-piece inflatable penile prosthesis placement: surgical technique Matthew J. Watson, Anand Shridharani Department of Urology, University of Tennessee-Chattanooga, Chattanooga, TN, USA Correspondence to: Anand Shridharani. Department of Urology, University of Tennessee-Chattanooga, Chattanooga, TN, USA. Email: [email protected]. Received: 06 April 2019; Accepted: 11 November 2019; Published: 05 July 2020. doi: 10.21037/jovs.2019.11.09 View this article at: http://dx.doi.org/10.21037/jovs.2019.11.09 Introduction Table 1 Penoscrotal IPP attributes Advantages of penoscrotal IPP placement The development of the inflatable penile prosthesis (IPP) in 1973 changed the landscape of erectile dysfunction Optimal corporal exposure (ED) management. It is the first and only treatment to Minimal risk of dorsal nerve injury prove efficacious in all males while simulating an erect Optimal approach in severely obese and flaccid state. Subsequent developments in the device, Anchoring of pump directly in scrotum such as new cylinder designs to prevent aneurysm, antibiotic coatings to reduce infection and lockout Optimal approach in patients with severe corporal fibrosis valves to prevent autoinflation, have caused the device Minimal scar to be widely accepted and utilized. Now IPPs more Can perform concomitant scrotoplasy, AUS placement, Mini- closely approximate natural flaccidity, natural erection Jupette (sling) through same incision and are much more reliable. The penoscrotal approach Disadvantages of penoscrotal IPP placement to IPP placement is most common approach utilized Blind placement of reservoir and performed in over 80% of the IPPs placed (1). Although the penoscrotal approach does not allow direct Increased scrotal swelling visualization of the reservoir placement, it likely derives IPP, inflatable penile prosthesis. -
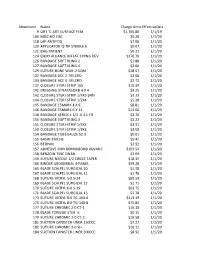
Mnemonic Name Charge Amounteffectivedate 9 ORT TJ ART
Mnemonic Name Charge AmountEffectiveDate 9 ORT TJ ART SURFACE FEM $1,765.80 1/1/19 100 MISC NO CHG $0.20 1/1/20 118 LAP ANTIFOG $7.06 1/1/20 120 APPLICATOR Q-TIP STERILE 6 $0.07 1/1/20 121 BAG PATIENT $0.21 1/1/20 124 ENDO ALLIANCE INFLAT SYRNG DEV $176.70 1/1/20 126 BANDAGE SOFT KLING 2 $1.88 1/1/20 127 BANDAGE SOFT KLING 4 $2.60 1/1/20 129 SUTURE BONE WAX 2.5QM $28.57 1/1/20 132 BANDAGE ACE 2 VELCRO $2.06 1/1/20 133 BANDAGE ACE 3 VELCRO $2.72 1/1/20 137 CLOSURE STERI-STRIP 1X5 $10.39 1/1/20 141 DRESSING STRATASORB 4 X 4 $9.25 1/1/20 142 CLOSURE STERI-STRIP 1/4X3 BRN $3.33 1/1/20 144 CLOSURE STERI-STRIP 1/2X4 $5.28 1/1/20 145 BANDAGE ESMARK 4 X 9 $8.81 1/1/20 146 BANDAGE ESMARK 6 X 12 $13.00 1/1/20 148 BANDAGE KERLIX 4 1/2 X 4.1 YD $3.70 1/1/20 150 BANDAGE SOFT KLING 3 $2.23 1/1/20 151 CLOSURE STERI-STRIP 1/4X3 $3.31 1/1/20 153 CLOSURE STERI-STRIP 1/8X3 $3.00 1/1/20 154 BANDAGE TUBEGAUZE SZ 3 $0.01 1/1/20 155 BASIN EMESIS $0.41 1/1/20 156 BEDPAN $2.92 1/1/20 157 ADHESIVE SKIN DERMABOND ADVANC $103.54 1/1/20 158 BENZOIN TINC SWAB $2.09 1/1/20 159 SUTURE NEEDLE 1/2 CIRCLE TAPER $18.35 1/1/20 160 BINDER ABDOMINAL 4-PANEL $59.28 1/1/20 165 BLADE SCALPEL SURGICAL 10 $1.78 1/1/20 167 BLADE SCALPEL SURGICAL 11 $1.78 1/1/20 168 SUTURE VICRYL 5-0 S-24 $69.59 1/1/20 169 BLADE SCALPEL SURGICAL 12 $1.71 1/1/20 170 SUTURE VICRYL 6-0 S-29 $63.75 1/1/20 171 BLADE SCALPEL SURGICAL 15 $1.78 1/1/20 173 SUTURE VICRYL 8-0 TG-160-6 $113.19 1/1/20 175 SUTURE VICRYL 8-0 TG-140-8 $75.84 1/1/20 177 SUTURE CHROMIC 2-0 CT-1 $16.10 1/1/20 178 BLADE TONGUE STER. -

Comparison of Ultrasonic Device Versus Bipolar Diathermy Tonsillectomy in Children Mukesh Kumar Sah,1 Yogesh Neupane,2 Rajendra Prasad Sharma Guragain,2
J Nepal Health Res Counc 2019 Jan-Mar;17(42): 71-5 Original Article DOI https://doi.org/10.33314/jnhrc.1751 Comparison of Ultrasonic Device Versus Bipolar Diathermy Tonsillectomy in Children Mukesh Kumar Sah,1 Yogesh Neupane,2 Rajendra Prasad Sharma Guragain,2 1Department of ENT- Head and Neck surgery, National medical college, Birgunj, Nepal, 2Department of ENT- Head and Neck surgery, Institute of medicine, Kathmandu, Nepal. ABSTRACT Background: Intraoperative bleeding and postoperative pain are two commonest concerns for both patient and surgeon in tonsillectomy. This study was aimed to compare intraoperative blood loss and early postoperative pain between ultrasonic device and bipolar diathermy tonsillectomy in children. Methods: Prospective, interventional, single blinded, comparative study was carried out from September 2016 to September 2017 including children up to age 15 years who underwent tonsillectomy either by bipolar diathermy or ultrasonic device. Intraoperative blood loss was recorded using standard sized gauge technique. Post-tonsillectomy pain on first five postoperative days (early postoperative pain) was assessed using Visual analog scale for children older than 5 years and FLACC score for children up to 5 years respectively.Means were compared. Results: 38 children (76 tonsils) were included in the study out of which 31 were boys (62 tonsils) and 7 were girls (14 tonsils). The mean intraoperative blood loss in ultrasonic dissection group was 13.94 ml and 13.91 ml in bipolar diathermy group. This difference was not statistically significant (p=0.974). Post-operative pain on 1st, 2nd, 3rd and 4th days were significantly less (p<0.05) in ultrasonic device group compared to bipolar diathermy group.