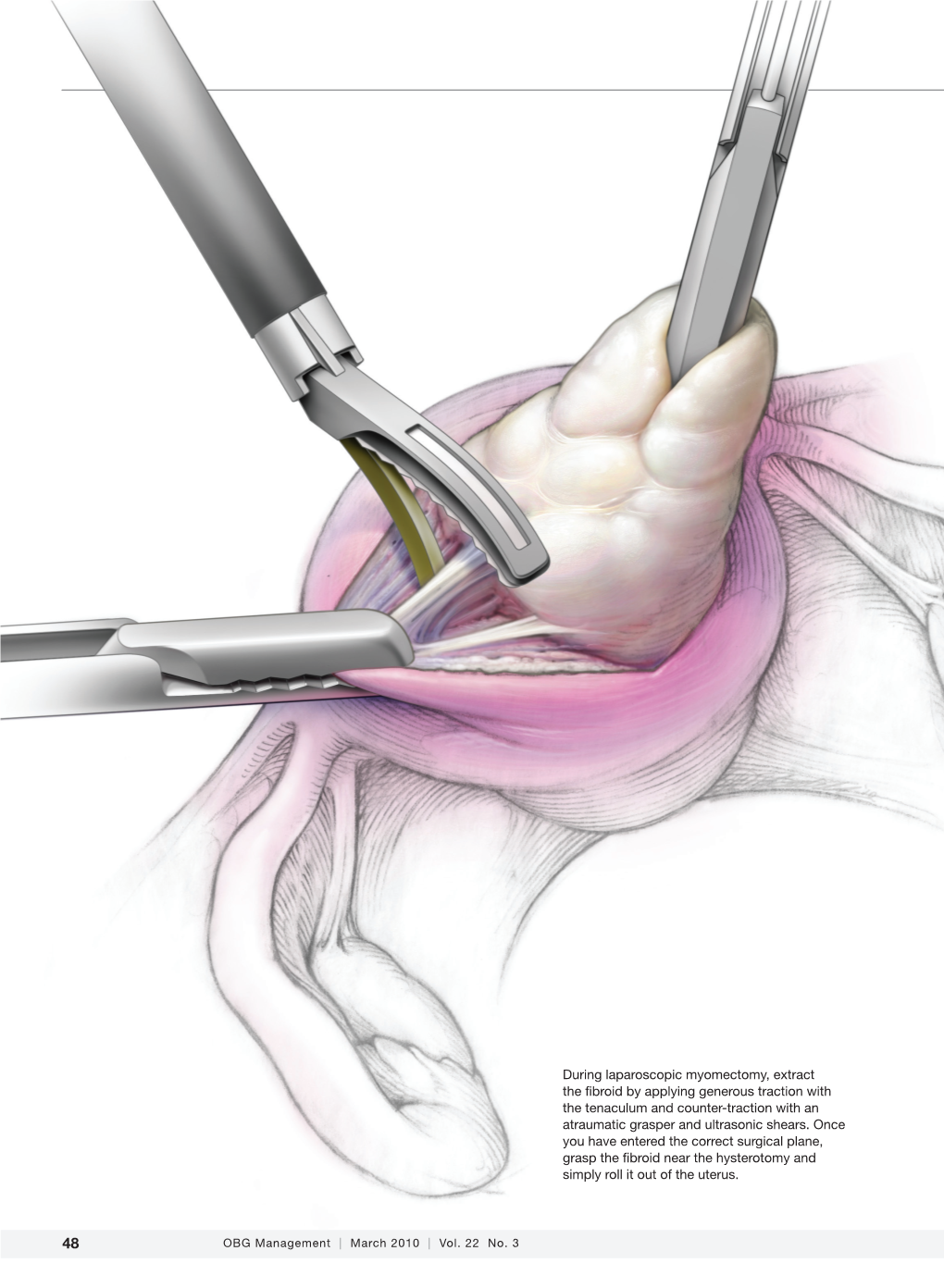
Einarsson-Myomectomy-Article.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CST-On-Demand-Binder.Pdf
Zander Perioperative Education Zander CST Exam Preparation Course Zander Perioperative Education Certification Preparation for CNOR, CAPA-CPAN, CST and CBSPD Wendy Zander MSN/Ed, RN, CNOR [email protected] Test Taking Strategies Objectives: 1. Apply Test Taking Strategies for the CST exam 2. Create a Personal Study Plan 3. Eligibility • Registering for the exam • Exam Format • Time Management • Test Taking Strategies Eligibility • Current or previously Certified Surgical Technologist (CST) ▫ Evidence of CST Certification • Graduate of a surgical technology program accredited by CAAHEP ▫ Evidence of proof of graduation • Graduate of a surgical technology accredited by ABHES ▫ Evidence of proof of graduation www.periop-ed.com 1 Zander Perioperative Education Military Eligible • A graduate of a military training program in surgical technology is always eligible whether it was before, during or after having CAAHEP accreditation. ▫ a copy of your DD214 (must state location of the base where program was completed), ▫ a copy of your graduation certificate from the surgical technology training program ▫ a smart transcript Accelerated Alternate Delivery (AAD) Pathway • Have on-the-job training in surgical technology • Are a graduate from a surgical technology program that did not hold CAAHEP accreditation during your enrollment CST Testing Fees First Time Test Takers Exam Fee (AST Members) Exam Fee (Non Members) $190 $290 Current or Previous Certified Surgical Technologist Renewing First Time Test Takers Certification by Examination Exam Fee -

AAGL Practice Report: Practice Guidelines for Management of Intrauterine Synechiae
Special Article AAGL Practice Report: Practice Guidelines for Management of Intrauterine Synechiae AAGL ADVANCING MINIMALLY INVASIVE GYNECOLOGY WORLDWIDE Background The search was not restricted to English language literature; committee members fluent in languages other than English re- Intrauterine adhesions (IUAs) have been recognized as viewed relevant articles and provided the committee with rel- a cause of secondary amenorrhea since the end of the 19th ative information translated into English. Because of the century [1], and in the mid-20th century, Asherman further paucity of data in this area, all published works were included described the eponymous condition occurring after preg- for the electronic database searches, and relevant articles not nancy [2]. The terms ‘‘Asherman syndrome’’ and IUAs are available in electronic sources (e.g., published before the be- often used interchangeably, although the syndrome requires ginning of electronic database commencement) were cross- the constellation of signs and symptoms (in this case, pain, referenced from hand-searched bibliographies and included menstrual disturbance, and subfertility in any combination) in the literature review. When necessary, authors were con- and the presence of IUAs [2]. The presence of IUAs in the tacted directly for clarification of points published. absence of symptoms may be best referred to as asymptom- atic IUAs or synechiae. Diagnosis Identification and Assessment of Evidence In women with suspected IUAs, physical examination usually fails to reveal abnormalities [3,4]. Blind transcervical This AAGL Practice Guideline was produced after elec- sounding of the uterus may reveal cervical obstruction at or tronic resources including Medline, PubMed, CINAHL, the near the level of the internal os [3]. -
Minimal Endoscope-Assisted Thyroidectomy Through a Retroauricular Approach: an Evolving Solo Surgery Technique
ORIGINAL ARTICLE Minimal Endoscope-assisted Thyroidectomy Through a Retroauricular Approach: An Evolving Solo Surgery Technique Myung Jin Ban, MD,*w Jae Won Chang, MD,z Won Shik Kim, MD,y Hyung Kwon Byeon, MD, PhD,y Yoon Woo Koh, MD, PhD,y and Jae Hong Park, MD, PhD* (RA), or transoral approach.1–5 Endoscopic thyroidectomy Abstract: This study aimed to evaluate the feasibility and efficacy of through an RA approach is an especially excellent choice minimal endoscope-assisted thyroidectomy (MEAT) through a for head and neck surgeons because of their familiarity with retroauricular (RA) approach. Most of the thyroidectomy oper- the direction of the approach, the short distance to the ative time was accounted for by direct visualization through the thyroid gland, and a good cosmetic outcome without the RA window, minimizing interference between surgical instruments. 6 Endoscope use was minimized and limited to critical surgical need for additional incisions. aspects, including preservation of the recurrent laryngeal nerve and Despite the advantages of the RA approach, funda- parathyroid glands. The recurrent laryngeal nerve was neuro- mental limitations of endoscopic surgery still exist, includ- monitored throughout the procedure. MEAT through an RA ing a narrow operative field that restricts the free movement approach was performed in 8 patients with papillary thyroid car- of instruments. Gas insufflation, an additional incision for cinoma (mean tumor size, 1.2 ± 0.5 cm). The mean patient age was the endoscope port, robotic arm assistance, and a flexible 41.1 ± 7.5 years. The endoscopic operating time was endoscope holder for solo surgery have all been used to 19 ± 3.4 minutes, and no postoperative hematoma, seroma, or overcome this limitation.3,7,8 vocal cord paralysis was observed. -

Comparison of Curettage and Hysteroscopy Plus Curettage After Uterine Arterial Embolization in the Treatment of Cesarean Scar Pregnancy
Comparison of Curettage and Hysteroscopy Plus Curettage After Uterine Arterial Embolization in the Treatment of Cesarean Scar Pregnancy Lili Cao Women's Hospital, Zhejiang University School of Medicine Zhida Qian Women's Hospital, Zhejiang University School of Medicine Lili Huang ( [email protected] ) Women's Hospital, Zhejiang University School of Medicine https://orcid.org/0000-0002-5919-3172 Research article Keywords: Cesarean scar pregnancy, Hysteroscopy, Curettage, Uterine artery embolization Posted Date: July 2nd, 2020 DOI: https://doi.org/10.21203/rs.3.rs-39244/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/11 Abstract Background: Caesarean scar pregnancy (CSP) stands for the advanced stage severe complication secondary to cesarean section, and its incidence shows an increasing trend recently. However, no consensus has been reached about the optimal CSP treatment. Methods: The childbearing CSP patients with a cesarean section history were evaluated by ultrasonography, with a gestational age of less than 10 weeks. 34 patients receiving dilation and curettage (D&C) and uterine artery embolization (UAE) were enrolled into the D&C group, while 46 undergoing hysteroscopy (H/S) and D&C after UAE were enrolled into the H/S+D&C group. Results: Differences in success rate and decrease in the β-hCG level in serum on the second day of surgery were not signicant between D&C and H/S+D&C groups (P>0.05). Also, differences in side effect rate, intraoperative blood loss amount, postoperative bleeding time, and total length of stay were not signicant between both groups (P>0.05). -

(8Th Edition) Procedure Code ACHI (8
Appendix 1. Procedure and Diagnostic Codes Used to Identify Prior Procedures Procedure ACHI (8th ACHI (8th edition) procedure names ICD-10- ICD-10-AM edition) AM diagnosis name procedure diagnosis code code Gynecological laparoscopy 35638-00 Laparoscopic wedge resection of ovary 35638-01 Laparoscopic partial oophorectomy 35638-02 Laparoscopic oophorectomy, unilateral 35638-03 Laparoscopic oophorectomy,bilateral 35638-04 Laparoscopic ovarian cystectomy, unilateral 35638-05 Laparoscopic ovarian cystectomy, bilateral 35638-06 Laparoscopic salpingotomy 35638-07 Laparoscopic partial salpingectomy, unilateral 35638-08 Laparoscopic partial salpingectomy, bilateral 35638-09 Laparoscopic salpingectomy, unilateral 35638-10 Laparoscopic salpingectomy, bilateral 35638-11 Laparoscopic salpingo-oophorectomy, unilateral 35638-12 Laparoscopic salpingo-oophorectomy, bilateral 35638-14 Laparoscopic uterosacral nerve ablation 35637-02 Laparoscopic diathermy of lesion of pelvic cavity 35637-04 Laparoscopic ventrosuspension 35637-07 Laparoscopic rupture of ovarian cyst or abscess 35637-08 Laparoscopic ovarian drilling 35637-10 Laparoscopic excision of lesion of pelvic cavity 35729-00 Laparoscopic transposition of ovary 90430-00 Laparoscopic repair of ovary 90433-00 Other laparoscopic repair of fallopian tube 35694-00 Laparoscopic salpingoplasty 35694-01 Laparoscopic anastomosis of fallopian tube 35694-02 Laparoscopic salpingolysis 35694-03 Laparoscopic salpingostomy 35694-06 Laparoscopic salpingotomy 35649-01* Myomectomy of uterus via laparoscopy Hysteroscopy, including operative hysteroscopy 35630-00 Diagnostic hysteroscopy 35649-00 Hysterotomy 35633-00 Division of uterine adhesions 35634-00 Division of uterine septum via hysteroscopy 35649-02 Division of uterine septum via hysterotomy 35633-01 Polypectomy of uterus via hysteroscopy 35623-00 Myomectomy of uterus via hysteroscopy Baldwin HJ, Patterson JA, Nippita TA, Torvaldsen S, Ibiebele I, Simpson JM, et al. Antecedents of abnormally invasive placenta in primiparous women: the risk from gynecologic procedures. -

Editorial Robert L
Editorial Robert L. Barbieri, MD Editor in Chief A stitch in time: The B-Lynch, Hayman, and Pereira uterine compression sutures All three of these uterine compression sutures are effective at treating postpartum hemorrhage caused by uterine atony—remember to use them CASE You are performing a cesarean carboprost tromethamine (Hemabate), others. Every obstetrician should be delivery for a 30-year-old G1P0 woman and methergine do not result in resolu- proficient with the placement of at who presented in labor with a breech tion of the hemorrhage. Your assistant least one uterine compression suture fetus at term. Earlier in the pregnancy suggests a uterine compression suture for the treatment of PPH caused by an external version was unsuccessful to treat the PPH. uterine atony. in achieving a cephalic presentation. What uterine compression suture The breech delivery of the newborn would you choose? Consider the hysterotomy is uncomplicated but, immediately When it’s open. When PPH caused following delivery of the placenta, he management of PPH can by uterine atony occurs at cesarean you note excessive uterine bleeding be conveniently described delivery and the hysterotomy inci- and diagnose a postpartum hemor- T using one algorithm for cases sion is open, the B-Lynch suture rhage (PPH) due to uterine atony. that follow a vaginal delivery, and ( FIGURE 1, page 8) is a common se- Manual massage of the uterus and another algorithm for PPH that lection by obstetricians. administration of oxytocin, misoprostol, occurs during cesarean delivery (see When it’s closed. When the hys- “Managing PPH following vaginal terotomy is already closed when and cesarean delivery” on page 10). -

Rapid HTA Report Ultrasonic Energy Devices for Surgery July 2014
Rapid HTA report 1 Ultrasonic energy devices for surgery July 2014 1 This report should be cited as: Migliore A, Corio M, Perrini MR, Rivoiro C, Jefferson T. Ultrasonic energy devices for surgery: rapid HTA report. Agenas, Agenzia nazionale per i servizi sanitari regionali. Rome, July 2014. Contributions Authors Antonio Migliore, Mirella Corio, Maria Rosaria Perrini, Chiara Rivoiro, and Tom Jefferson Agenas, Agenzia nazionale per i servizi sanitari regionali, Area Funzionale Innovazione, Sperimentazione e Sviluppo, via Puglie 23, 00187 Rome (Italy) Corresponding author Antonio Migliore, MSc ([email protected]) Clinical experts Mario Alessiani, MD FACS Division of General Surgery, Varzi Hospital, University of Pavia (Italy) Marco Filauro, MD Division of General and Hepatobiliopancreatic Surgery, Galliera Hospital, Genova (Italy) Invited reviewers Chuong Ho, MD MSc Canadian Agency for Drugs and Technologies in Health (CADTH), Ottawa (Canada) Björn Fahlgren, MSc 2 Comité d’évaluation des technologies de santé (CEDIT), Paris (France) Acknowledgements Authors would like to thank Marina Cerbo (Agenas) and Simona Paone (Agenas), for the valuable help in reviewing the research protocol and the first draft of the report, Patrizia Brigoni (Agenas) for performing the systematic literature searches, Fabio Bernardini (Agenas) for his relevant support in retrieving the publications, and Laura Velardi (Agenas) for supporting consultation and analysis of databases. Declaration on the conflict of interest and privacy Authors, Clinical expert and External Reviewers declare that they do not receive benefits or harms from the publication of this report. None of the authors have or have held shares, consultancies or personal relationships with any of the producers of the devices assessed in this document. -

Physicians As Assistants at Surgery: 2016 Update
Physicians as Assistants at Surgery: 2016 Update Participating Organizations: American College of Surgeons American Academy of Ophthalmology American Academy of Orthopaedic Surgeons American Academy of Otolaryngology – Head and Neck Surgery American Association of Neurological Surgeons American Pediatric Surgical Association American Society of Colon and Rectal Surgeons American Society of Plastic Surgeons American Society of Transplant Surgeons American Urological Association Congress of Neurological Surgeons Society for Surgical Oncology Society for Vascular Surgery Society of American Gastrointestinal Endoscopic Surgeons The American College of Obstetricians and Gynecologists The Society of Thoracic Surgeons Physicians as Assistants at Surgery: 2016 Update INTRODUCTION This is the seventh edition of Physicians as Assistants at Surgery, a study first undertaken in 1994 by the American College of Surgeons and other surgical specialty organizations. The study reviews all procedures listed in the “Surgery” section of the 2016 American Medical Association’s Current Procedural Terminology (CPT TM). Each organization was asked to review new codes since 2013 that are applicable to their specialty and determine whether the operation requires the use of a physician as an assistant at surgery: (1) almost always; (2) almost never; or (3) some of the time. The results of this study are presented in the accompanying report, which is in a table format. This table presents information about the need for a physician as an assistant at surgery. Also, please note that an indication that a physician would “almost never” be needed to assist at surgery for some procedures does NOT imply that a physician is never needed. The decision to request that a physician assist at surgery remains the responsibility of the primary surgeon and, when necessary, should be a payable service. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Case Report Management of Total Transection of Nasoendotracheal Tube During Lefort I Osteotomy
Hindawi Case Reports in Anesthesiology Volume 2020, Article ID 2097240, 4 pages https://doi.org/10.1155/2020/2097240 Case Report Management of Total Transection of Nasoendotracheal Tube during LeFort I Osteotomy Miles Somers ,1 Peter Tsakiris,1 Peter Isert,2 and Samuel Kim 1 1Department of Oral and Maxillofacial Surgery, Prince of Wales Hospital, Randwick, NSW, Australia 2VMO Anaesthetist, Prince of Wales Private Hospital, Randwick, NSW, Australia Correspondence should be addressed to Miles Somers; [email protected] Received 10 March 2020; Revised 8 August 2020; Accepted 26 October 2020; Published 17 November 2020 Academic Editor: Pavel Michalek Copyright © 2020 Miles Somers et al. *is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Transection of the nasoendotracheal tube during orthognathic surgery is a rare, but life-threatening complication. We present a case of complete nasoendotracheal tube transection during a LeFort 1 osteotomy and discuss appropriate preventative and management techniques. 1. Introduction 2. Case Report Complete transection of the nasoendotracheal tube (NET) A 28-year-old male underwent a 2-piece maxillary osteot- during surgery is rare [1]. However, it poses a potentially life- omy plus right ramus graft for genioplasty. *e aim of the threatening complication that must be managed effectively. surgery was orthognathic correction of a dentoskeletal class *ere are several reported cases in the literature reporting III malocclusion related to hypoplasia of the maxilla sec- both complete [2, 3] and partial transection [4–7]. Maxil- ondary to cleft lip and palate. -

Transabdominal Cerclage: Different Indications, Optimal Outcome
ISSN: 2474-1353 Sabr and Yousef. Int J Womens Health Wellness 2018, 4:067 DOI: 10.23937/2474-1353/1510067 Volume 4 | Issue 1 International Journal of Open Access Women’s Health and Wellness CASE REPORT Transabdominal Cerclage: Different Indications, Optimal Outcome. Two Case Reports Yasser Sabr* and Sara W Yousef Check for Department of Obstetrics and Gynecology, Collage of Medicine, King Saud University, Riyadh, Saudi Arabia updates *Corresponding author: Yasser Sabr, Department of Obstetrics and Gynecology, Collage of Medicine, King Saud University, Riyadh, Saudi Arabia, E-mail: [email protected] Abstract Case 1 Transabdominal placement of a cerclage at the cervicoisth- 25-years-old woman gravida 2 para 0 abortus 1 mic junction appears to be a safe and effective procedure known case of congenital hypoplastic upper vagina, for for reducing the incidence of spontaneous pregnancy loss that she underwent multiple vaginal surgeries including in selected patients with cervical insufficiency, we reported a case series of two woman with different indications for ab- vaginal septum resection, vaginoplasty (vaginostomy). dominal cerclage. Case 1 is a 25-years-old woman gravida After the procedures, Patient was unable to get preg- 2 para 0 abortus 1 known case of hypoplastic upper vagina nant for 1 year, so she came back and hysteroscopy who had 2 vaginal repair (vaginostomy) and had abdominal with examination under anesthesia was done, which cerclage for short cervix and delivered by caesarean sec- revealed stenosed upper vagina and very short cervix tion at 38 weeks a healthy baby boy. Case 2 is a 34-years- old woman gravida 5 para 0 abortus 4 known case of dia- with normal uterine cavity. -

Thoracoscopic Spine Surgery for Decompression and Stabilization of the Anterolateral Thoracolumbar Spine
Neurosurg Focus 19 (6):E4, 2005 Thoracoscopic spine surgery for decompression and stabilization of the anterolateral thoracolumbar spine AMIN AMINI, M.D., M.SC., RUDOLF BEISSE, M.D., AND MEIC H. SCHMIDT, M.D. Department of Neurosurgery, University of Utah, Salt Lake City, Utah; and Department of Trauma Surgery, Berufsgenossenschaftliche Unfallklinik Murnau, Germany The anterior thoracolumbar spine can be exposed via a variety of approaches. Historically, open anterolateral or pos- terolateral approaches have been used to gain access to the anterior thoracolumbar spinal column. Although the expo- sure is excellent, open approaches are associated with significant pain and respiratory problems, substantial blood loss, poor cosmesis, and prolonged hospitalization. With the increasing use of the endoscope in surgical procedures and recent advances in video-assisted thoracoscopic surgery, minimally invasive thoracoscopic spine surgery has been developed to decrease the morbidity associated with open thoracotomy. The purpose of this article is to illustrate the surgical technique of a minimally invasive thoracoscopic approach to the anterolateral thoracolumbar spine and to dis- cuss its potential indications and contraindications in patients with diseases involving the anterior thoracic and lumbar regions. KEY WORDS • endoscopic spinal surgery • thoracoscopy • thoracic spine • lumbar spine • thoracoscopic spinal instrumentation Since the introduction of thoracoscopic surgery by Jaco- Minimal access surgical techniques can potentially de- baeus15 in 1910, the technique has undergone enormous crease spinal access morbidity and speed recovery and advances. With the development of high-quality video im- healing.4,7,16,17 At the University of Utah Medical Center, we aging, small endoscopes, and modified new instruments, have performed 30 thoracoscopic spine surgeries for tho- video-assisted thoracic surgery has become the minimally racolumbar trauma, tumors, and infection.