Nutrition Analysis Post Gu ‘12
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Somalia Complex Emergency Fact Sheet #1- 04-26-2013
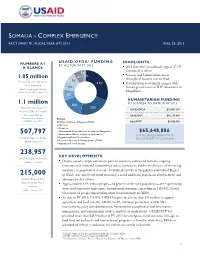
SOMALIA - COMPLEX EMERGENCY FACT SHEET #1, FISCAL YEAR (FY) 2013 APRIL 26, 2013 USAID/OFDA 1 F U N D I N G NUMBERS AT HIGHLIGHTS BY SECTOR IN FY 2013 A GLANCE 2013 Somalia Consolidated Appeal (CAP) requests $1.3 billion 2% Security and humanitarian access 6% 1% 1.05 million throughout Somalia remain fluid 7% People Experiencing Acute 31% Humanitarian community engages with Food Insecurity 7% Somali government on IDP relocations in U.N. Food Security and Nutrition Analysis Unit (FSNAU) – April 2013 Mogadishu 8% HUMANITARIAN FUNDING 1.1 million TO SOMALIA TO DATE IN FY 2013 15% Total Internally Displaced 23% USAID/OFDA $15,069,387 Persons (IDPs) in Somalia Office of the U.N. High USAID/FFP2 $45,579,499 Commissioner for Refugees Health 3 (UNHCR) – April 2013 Water, Sanitation, & Hygiene (WASH) State/PRM $5,000,000 Nutrition Protection Humanitarian Coordination & Information Management $65,648,886 507,797 Humanitarian Studies, Analysis, or Applications TOTAL USAID AND STATE Somali Refugees in Kenya Logistics and Relief Commodities ASSISTANCE TO SOMALIA Economic Recovery & Market Systems (ERMS) UNHCR – April 2013 Agriculture & Food Security 238,957 KEY DEVELOPMENTS Somali Refugees in Ethiopia UNHCR – April 2013 Despite security improvements in parts of southern and central Somalia, ongoing insecurity and restricted humanitarian access continue to hinder the delivery of life-saving assistance to populations in need. Al-Shabaab activity in Mogadishu and Bakool Region 215,000 in March and April heightened insecurity, caused additional population displacement, and Acutely Malnourished obstructed relief efforts. Children under Five in Approximately 1.05 million people—14 percent of the total population—are experiencing Somalia FSNAU – February 2013 acute food insecurity and require humanitarian assistance, according to FSNAU. -

Somalia Emergency Weekly Health Update Aims to Provide an Overview of the Health Activities Conducted by WHO and Health Partners in Somalia
SSoommaalliiaa EEmmeerrggeennccyy WWeeeekkllyy HHeeaalltthh UUppddaattee The Somalia emergency weekly health update aims to provide an overview of the health activities conducted by WHO and health partners in Somalia. It compiles health information including nine health events (epidemiological surveillance) reported in Somalia, information on ongoing conflicts in some regions of Somalia and health responses from partners. For further information please contact: Pieter Desloovere - Communications Officer - [email protected] - T: +254 733 410 984 BULLETIN HIGHLIGHTS Reporting dates 1-14 April 2012 (reflecting Epidemiological week 13 and 14) • On 4 April, a female suicide bomber killed at least six people at National Theater in Mogadishu. According to three major hospitals in Mogadishu, the caseload accounted for 80 casualties, including eight death. • On 9 April, more than 40 casualties were brought to Baidoa hospital after a bomb exploded at the market place of Baidoa. • Child Health Days have kicked off, on 10 April in Gedo region as well as Banadir region. Two rounds will be organized in Banadir region, with round one from 14-18 April 2012 and round two from 21-25 April 2012. Proportion of timely reporting sentinel sites by zone % 100 90 80 70 67 facilitiess 65 60 59 63 61 R. 57 57 50 52 54 of 50 40 42 36 30 20 23 Proporton 10 0 1234567891011121314 Weeks South & Central Puntland Somaliland Of the 222 sentinel sites reporting weekly from the three zones of Somalia, for week 13, 98% (53) in Puntland, 98% (44) in Somaliland, but only 36% (44) sentinel sites reported on time from South and Central Somalia or 64% (141) of all sentinel sites. -

S.No Region Districts 1 Awdal Region Baki
S.No Region Districts 1 Awdal Region Baki District 2 Awdal Region Borama District 3 Awdal Region Lughaya District 4 Awdal Region Zeila District 5 Bakool Region El Barde District 6 Bakool Region Hudur District 7 Bakool Region Rabdhure District 8 Bakool Region Tiyeglow District 9 Bakool Region Wajid District 10 Banaadir Region Abdiaziz District 11 Banaadir Region Bondhere District 12 Banaadir Region Daynile District 13 Banaadir Region Dharkenley District 14 Banaadir Region Hamar Jajab District 15 Banaadir Region Hamar Weyne District 16 Banaadir Region Hodan District 17 Banaadir Region Hawle Wadag District 18 Banaadir Region Huriwa District 19 Banaadir Region Karan District 20 Banaadir Region Shibis District 21 Banaadir Region Shangani District 22 Banaadir Region Waberi District 23 Banaadir Region Wadajir District 24 Banaadir Region Wardhigley District 25 Banaadir Region Yaqshid District 26 Bari Region Bayla District 27 Bari Region Bosaso District 28 Bari Region Alula District 29 Bari Region Iskushuban District 30 Bari Region Qandala District 31 Bari Region Ufayn District 32 Bari Region Qardho District 33 Bay Region Baidoa District 34 Bay Region Burhakaba District 35 Bay Region Dinsoor District 36 Bay Region Qasahdhere District 37 Galguduud Region Abudwaq District 38 Galguduud Region Adado District 39 Galguduud Region Dhusa Mareb District 40 Galguduud Region El Buur District 41 Galguduud Region El Dher District 42 Gedo Region Bardera District 43 Gedo Region Beled Hawo District www.downloadexcelfiles.com 44 Gedo Region El Wak District 45 Gedo -

Reserve 2016 Direct Beneficiaries : Men Women Boys Girls Total 7
Requesting Organization : Save the Children Allocation Type : Reserve 2016 Primary Cluster Sub Cluster Percentage Water, Sanitation and Hygiene 50.00 Education 50.00 100 Project Title : Provide life-saving basic WASH services for the drought affected populations in Bari and Hiran regions via schools Allocation Type Category : OPS Details Project Code : Fund Project Code : SOM-16/3485/R/WASH-Ed/INGO/4455 Cluster : Project Budget in US$ : 450,000.44 Planned project duration : 6 months Priority: Planned Start Date : 01/02/2017 Planned End Date : 31/07/2017 Actual Start Date: 01/02/2017 Actual End Date: 31/07/2017 Project Summary : Save the Children is intending to reduce the vulnerability of the drought affected communities and ensure the retention of children at schools in rural villages in Bari and Hiran regions through provision of life-saving basic WASH services via the schools. The proposed intervention will link with SC’s ongoing emergency response interventions of WASH, Education, Heath, Nutrition and Food Security, Livelihoods, all defined to provide a combination of lifesaving and resilience building support to drought affected communities in Puntland and Hiran. The proposed project activities will include provision of water supply through voucher system via schools to drought affected communities and school children to meet the drinking, cooking and personal hygiene needs, rehabilitation of strategic water sources at the community, provision of operation and maintenance tools, rehabilitation of WASH facilities in the target schools, trainings and dissemination of hygiene best practice through IECs. In addition, Save the Children will provide 4000 households from the drought affected populations with 2 water storage containers of 20 litters per household and PuR sachets for water treatment at the household level. -
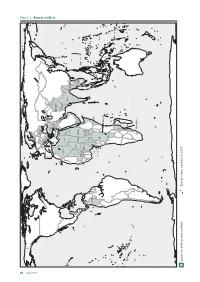
Map 1.1. Armed Con Icts
20 Map 1 . 1. Armed conicts Ukraine Turkey Syria Palestine Afghanistan Iraq Israel Algeria Pakistan Libya Egypt India Myanmar Mali Niger Chad Sudan Thailand Yemen Burkina Philippines Faso Nigeria South CAR Sudan Colombia Benin Somalia Cameroon DRC Burundi (Kasai) Mozambique Countries with armed conicts End of armed conict in 2019 Alert 2020 1. Armed conflicts • 34 armed conflicts were reported in 2019, 32 of them remained active at the end of the year. Most of the conflicts occurred in Africa (16), followed by Asia (nine), the Middle East (six), Europe (two) and America (one). • Repression by the Burundian government and the youth wing of the ruling party CNDD-FDD, the Imbonerakure, intensified prior to the 2020 elections. • The widespread reduction of violence and the beginning of the demobilisation of armed groups led to the end of the armed conflict in the Congolese region of Kasai. • There was an escalation of violence by the ADF in eastern DRC as a result of a military operation conducted by the Congolese Armed Forces in the last quarter of the year. • Various analysts highlighted that ISIS would be seeking a greater role in the conflict in the Lake Chad region, which mainly affects northeast Nigeria and the neighbouring regions of Chad, Cameroon and Niger, due to the increase in the group’s actions. • Violence in the Cabo Delgado province in northern Mozambique increased due to the presence of armed groups calling themselves jihadists. • South Sudan, with 2.21 million refugees, ranked as the largest refugee crisis in Africa and the third largest in the world, behind Syria and Afghanistan. -

General Meeting
General Meeting UNOPS – Nairobi February 23, 2015 Agenda • Review of Action Points • Post-Deyr Seasonal Assessment - FSNAU • Food Security Response Update • Risk Management Unit Presentation • “Mobile Money Payments for CFW” Report – FAO • Risk Management through Remote Sensing – SWALIM • Cash & Markets Task Force Update • AOB Review of Action Points Change in structure - Review of APs during FSC meeting - Review of minutes when circulated Action Points: • Members were requested to inform the FSC if they had any reservations with the cluster sharing all information regarding the 4W matrix when submitting reports. This followed the FSC survey to its partners regarding whether to share or not share the identity of the partners that were implementing FSC programs. Information for Better Livelihoods KEY FINDINGS FROM THE 2014/15 POST Deyr SEASONAL FOOD SECURITY AND NUTRITION ASSESSMENT IN SOMALIA Food Security Cluster Meeting 23 February 2015, Nairobi FSNAU Post Deyr 2014/15 Seasonal Assessment Scope and timeline: Food security and nutrition assessment of rural, urban and displaced populations across Somalia between October-December (for field work) Process: (1)FSNAU-led assessment with the participation of Technical staff of other UN agencies, partners and government institutions (2) Regional and All-Team analysis workshops in Garowe & Hargeisa with government and partners (3) Technical vetting in Mogadishu (Nutrition) and Nairobi with government and partners (5) Presentation to Government authorities (Mogadishu, Garowe and Hargeisa) (6) Presentation to other stakeholders in Nairobi and technical release (7) Public dissemination (technical release, food security and nutrition outlook; comprehensive technical reports) Civil Insecurity- Most Likely Scenario (Jan-Jun 2015) Security risks: High or Medium security risk in most of the South-Central Somalia. -
Belet Weyne District Survey
NUTRITION SURVEY REPORT BELEDWEYNE DISTRICT HIRAAN REGION SOMALIA UNICEF SOUTH/CENTRAL ZONE OF SOMALIA BAIDOA OFFICE APRIL 2000 Beledweyne District Nutrition Survey, April 2000 1. INTRODUCTION This nutrition survey is the seventh in a series of surveys that UNICEF has conducted in Central and Southern Somalia since September 1999 and the third within the framework of the joint UNICEF/FSAU survey agreement. UNICEF planned the survey, conducted the fieldwork, trained enumerators, monitored survey activities, and carried out data analysis and interpretation. UNICEF is grateful to Somalia Red Crescent Society who facilitated the work in Beledweyne. 1.2. SURVEY JUSTIFICATION UNICEF has supported a supplementary feeding programme in Beledweyne town during the past three years through International Medical Corps (IMC) yet there continues to be evidence of increasing malnutrition rate amongst the population in Beledweyne District although the level of malnutrition is not well documented. There have been alarming reports of food insecurity and displacement mainly in the pastoral and agro-pastoral areas resulting in a decision to conduct a nutrition survey in Beledweyne District, including the displaced population and residents. 1.3 SURVEY OBJECTIVES - To determine the level of malnutrition and Oedema in Beledweyne District by screening the Weight for Height measurement of children between 6– 59 months or 65-110cm. - To measure the determinant factors causing/contributing to existence of malnutrition by recording the occurrence of diarrhoea and ARI diseases in the two weeks prior to the survey. - To measure measles vaccination and Vitamin A supplementation coverage in Beledweyne District and monitor performance in the past 6 months. - To measure the extent of household movements during the changes in Beledweyne District, which has impacted on aid service deliveries. -
SOMALIA Post-Deyr 2012 Food Security and Nutrition Outlook January to June 2013
SOMALIA Post-Deyr 2012 Food Security and Nutrition Outlook January to June 2013 Despite improvements, more than one million likely to remain in Crisis through June 2013 KEY MESSAGES Figure 1. Current rural food security outcomes, January 2013 • As a result of positive impact of the good Deyr rains on livestock and crop performance and continued humanitarian assistance, the number of people in Crisis and Emergency (IPC Phases 3 and 4) has halved to 1.05 million since August. Even so, malnutrition rates in Somalia remain among the highest in the world, according to surveys conducted from October to December 2012. Humanitarian assistance to protect livelihoods, reduce acute malnutrition, and help the most food insecure populations meet their food needs is still necessary. • With the onset of the January to March Jilaal dry season, livestock productivity will decrease, but no major changes in food security classification are expected between now and June. However, livelihoods in Somalia remain at risk to a wide variety of hazards such as limited water access. • Early forecasts are that the April to June Gu rains will be normal to below normal in terms of total rainfall. However, if total seasonal rainfall is well below average or very poorly distributed unlike in the early forecast, the food insecure population is likely to increase. The primary areas affected would likely be maize-growing, agropastoral areas of the South. Source: FSNAU, FEWS NET Somalia, and partners Graphic: FSNAU This map represents acute food insecurity outcomes relevant for emergency decision-making. It does not necessarily reflect chronic food insecurity. -
Joint Multi-Cluster Needs Assessment (JMCNA) Round III
SOMALIA Joint Multi-Cluster Needs Assessment (JMCNA) Round III November 2019 Informing more effective REACH humanitarian action Somalia Joint Multi-Cluster Needs Assessment, November 2019 Assessment conducted in the framework of: Somalia Assessment Working Group Somalia Information Management Working Group Funded by: With the support of: Data collection partners: Action Contre la Faim (ACF), American Refugee Committee (ARC), Concern Worldwide (CWW), Danish Refugee Council (DRC), HIMILO Foundation (HIMFO), International Organisation for Migration (IOM), Islamic Relief, MCA Network, Mercy Corps, Norwegian Church Aid (NCA), Norwegian Refugee Council (NRC), Oxfam, Polish Humanitarian Action (PAH), Skills Active Forward (SAF-UK), Save the Children (SCI), Somali Community Concern (SCC), Shabelle Community Development Organisation (SHACDO), Secours Islamique France (SIF), Somali Aid, SOS Children’s Village International, United Nations High Commissioner for Refugees (UNHCR), Women and Child Care Organisation (WOCCA), World Vision, and Wamo Relief, Rehabilitation Services (WRRS), and the Somali Ministry of Humanitarian Affairs and Disaster Management. 1 Somalia Joint Multi-Cluster Needs Assessment, November 2019 Enumerator and respondent, during JMCNA data collection, © REACH About REACH REACH facilitates the development of information tools and products that enhance the capacity of aid actors to make evidence-based decisions in emergency, recovery and development contexts. The methodologies used by REACH include primary data collection and in-depth analysis, and all activities are conducted through inter-agency aid coordination mechanisms. REACH is a joint initiative of IMPACT Initiatives, ACTED and the United Nations Institute for Training and Research - Operational Satellite Applications Programme (UNITAR-UNOSAT). For more information please visit our website: www.reach-initiative.org. You can contact us directly at: [email protected] and follow us on Twitter @REACH_info. -

Final Performance Evaluation of the Transition Initiatives for Stabilization Project Idiq Aid-623-I-14-00009 Task Order Aid-623-T0-15-00014
SOMALIA PROGRAM SUPPORT SERVICES FINAL PERFORMANCE EVALUATION OF THE TRANSITION INITIATIVES FOR STABILIZATION PROJECT IDIQ AID-623-I-14-00009 TASK ORDER AID-623-T0-15-00014 June 4, 2016 This publication was produced at the request of the United States Agency for International Development. It was prepared by International Business & Technical Consultants, Inc. under IDIQ AID-623-I-14-00009, Task Order /AID- 623-TO-15-00014 1 SOMALIA PROGRAM SUPPORT SERVICES FINAL PERFORMANCE EVALUATION OF THE TRANSITION INITIATIVES FOR STABILIZATION PROJECT IDIQ AID-623-I-14-00009, TASK ORDER /AID-623-TO-15-00014 June 4, 2016 Authors: Roger Pipe, Jama Egal, Jane Meme, Lucas Malla, Zamzam Billow and Aden Abdi. International Business & Technical Consultants, Inc. (IBTCI) Additional input was provided by Mamuka Shatirishvili, Jeffrey Swedberg, and Gayla Cook of IBTCI, and consultant David Sip. In the US: IBTCI Home Office 8618 Westwood Center Drive Suite 400 Vienna, VA 22182 USA +1.703.749.0100 In Kenya : Park Office Suites, #9, Ground Floor Parklands, Nairobi +254.786.866.793 IDIQ AID-623-I-14-00009 DISCLAIMER The authors’ views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. COVER PHOTO: Women celebrate during a Community Dialogue Event in Hodan, Mogadishu. Photo: Alinur Hassan, IOM. i CONTENTS CONTENTS ................................................................................................................................................................................ -
Community-Based and Customary Taxation in South-Central Somalia: Possibilities for Hybrid Governance and DIALOGUE Programming !
! ! ! Community-based and customary taxation in south-central Somalia: Possibilities for hybrid governance and DIALOGUE programming ! Report!commissioned!by!the!Danish!Refugee!Council,!Somalia! ! Written!by!Kailee!Jordan!! TABLE OF CONTENTS ! ! Executive!Summary……………………………………………………………………………………………………………...…..3! ! I.!Introduction…………………………………………………………………………………………………………………………7! ! II.!Research!context! ! Taxation,!state!building!and!good!governance………………………………………………………………………..……8! Taxation!and!state!building!in!southFcentral!Somalia………………………………………………………...…………9! CDRD!and!DIALOGUE………………………………………………………………………………………………………………10! Methodology………………………………………………………………………………………………………………….…………11! Limitations……………………………………………………………………………………………………………….………………12! Case!study!selection:!Hiran!and!Jubaland……………………………………………………………………………….….13! ! III.!Key!Findings! 1.! Actors,!services,!and!networks:!mapping!existing!mechanisms……………………………………….15! 1.1!Key!actors!……………………………………………………..................................................…………………….15! 1.2!Service!provision!and!local!collective!action………………………………………..……………………19! 1.3!Collaborations!across!actors!and!service!provisions………………………………………….………21! ! 2.! Payments!and!revenue!collection…………………………………………………………………………..….…...22! 2.1!Customary!taxation!and!payments!to!nonFstate!actors………………………………………………27! !!! 2.1.1!Clan!payments…………………………………………………………………………………..………27! !!! 2.1.2!Payments!to!religious!entities…………………………………………………………...……….28! 2.1.3!Social!contributions!and!civil!society!payments!………………………………………...29! 2.1.4!Payments!to!private!service!actors………………………………………..…………………...30! -

Danish Immigration Service
Danish Immigration Service _______________________________________________ Report on the Nordic fact-finding mission to Nairobi, Kenya, and the Middle Shabelle region of Somalia 21 February – 6 March 1998 Copenhagen, September 1999 Report on Nordic fact-finding mission to Nairobi (Kenya) and the Middle Shabelle region of Somalia Contents EXECUTIVE SUMMARY................................................................................................................4 BACKGROUND TO THE MISSION..............................................................................................5 POLITICAL AND SECURITY SITUATION, ETC. IN CENTRAL AND SOUTHERN SOMALIA...........................................................................................................................................6 CLAN-BASED SECURITY.....................................................................................................................6 A SOCIETY ROOTED IN CONFLICT.......................................................................................................6 RECURRENT HUMANITARIAN CRISES .................................................................................................8 1. DIVISION OF CENTRAL AND SOUTHERN SOMALIA INTO ZONES IN GENERAL …………………………………………………………………………………………………10 2. RISK OF PERSECUTION ON CLAN, ETHNIC OR POLITICAL GROUNDS .............13 2.1. GENERAL POINTS.................................................................................................................13 2.2. VULNERABLE POPULATION GROUPS ....................................................................................13