Antimicrobial Stewardship: Getting the Most out of Culture and Susceptibility Tests Insights from a Microbiologist
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sebastien Lefebvre
A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sebastien Lefebvre To cite this version: Tessa Trouchon, Sebastien Lefebvre. A Review of Enrofloxacin for Veterinary Use. Open Journal of Veterinary Medicine, 2016, 6 (2), pp.40-58. 10.4236/ojvm.2016.62006. hal-01503397 HAL Id: hal-01503397 https://hal.archives-ouvertes.fr/hal-01503397 Submitted on 7 Apr 2017 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution - NoDerivatives| 4.0 International License Open Journal of Veterinary Medicine, 2016, 6, 40-58 Published Online February 2016 in SciRes. http://www.scirp.org/journal/ojvm http://dx.doi.org/10.4236/ojvm.2016.62006 A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sébastien Lefebvre USC 1233 INRA-Vetagro Sup, Veterinary School of Lyon, Marcy l’Etoile, France Received 12 January 2016; accepted 21 February 2016; published 26 February 2016 Copyright © 2016 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract This review outlines the current knowledge on the use of enrofloxacin in veterinary medicine from biochemical mechanisms to the use in the field conditions and even resistance and ecotoxic- ity. -

Antibiotic Use Guidelines for Companion Animal Practice (2Nd Edition) Iii
ii Antibiotic Use Guidelines for Companion Animal Practice (2nd edition) iii Antibiotic Use Guidelines for Companion Animal Practice, 2nd edition Publisher: Companion Animal Group, Danish Veterinary Association, Peter Bangs Vej 30, 2000 Frederiksberg Authors of the guidelines: Lisbeth Rem Jessen (University of Copenhagen) Peter Damborg (University of Copenhagen) Anette Spohr (Evidensia Faxe Animal Hospital) Sandra Goericke-Pesch (University of Veterinary Medicine, Hannover) Rebecca Langhorn (University of Copenhagen) Geoffrey Houser (University of Copenhagen) Jakob Willesen (University of Copenhagen) Mette Schjærff (University of Copenhagen) Thomas Eriksen (University of Copenhagen) Tina Møller Sørensen (University of Copenhagen) Vibeke Frøkjær Jensen (DTU-VET) Flemming Obling (Greve) Luca Guardabassi (University of Copenhagen) Reproduction of extracts from these guidelines is only permitted in accordance with the agreement between the Ministry of Education and Copy-Dan. Danish copyright law restricts all other use without written permission of the publisher. Exception is granted for short excerpts for review purposes. iv Foreword The first edition of the Antibiotic Use Guidelines for Companion Animal Practice was published in autumn of 2012. The aim of the guidelines was to prevent increased antibiotic resistance. A questionnaire circulated to Danish veterinarians in 2015 (Jessen et al., DVT 10, 2016) indicated that the guidelines were well received, and particularly that active users had followed the recommendations. Despite a positive reception and the results of this survey, the actual quantity of antibiotics used is probably a better indicator of the effect of the first guidelines. Chapter two of these updated guidelines therefore details the pattern of developments in antibiotic use, as reported in DANMAP 2016 (www.danmap.org). -

WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -

Nitroaromatic Antibiotics As Nitrogen Oxide Sources
Review biomolecules Nitroaromatic Antibiotics as Nitrogen Oxide Sources Review Allison M. Rice, Yueming Long and S. Bruce King * Nitroaromatic Antibiotics as Nitrogen Oxide Sources Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; Allison M. Rice , Yueming [email protected] and S. Bruce (A.M.R.); King [email protected] * (Y.L.) * Correspondence: [email protected]; Tel.: +1-336-702-1954 Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; [email protected]: Nitroaromatic (A.M.R.); [email protected] antibiotics (Y.L.) show activity against anaerobic bacteria and parasites, finding * Correspondence: [email protected]; Tel.: +1-336-702-1954 use in the treatment of Heliobacter pylori infections, tuberculosis, trichomoniasis, human African trypanosomiasis, Chagas disease and leishmaniasis. Despite this activity and a clear need for the Abstract: Nitroaromatic antibiotics show activity against anaerobic bacteria and parasites, finding usedevelopment in the treatment of new of Heliobacter treatments pylori forinfections, these conditio tuberculosis,ns, the trichomoniasis, associated toxicity human Africanand lack of clear trypanosomiasis,mechanisms of action Chagas have disease limited and their leishmaniasis. therapeutic Despite development. this activity Nitroaro and a clearmatic need antibiotics for require thereductive development bioactivation of new treatments for activity for theseand this conditions, reductive the associatedmetabolism toxicity can convert -

Comparative Efficacy of Kanamycin, Enrofloxacin, Moxifloxacin and Cefoperazone for the Treatment of Pneumonia in Buffaloes
Journal of Animal Research: v.8 n.5, p. 807-811. October 2018 DOI: 10.30954/2277-940X.10.2018.10 Comparative Efficacy of Kanamycin, Enrofloxacin, Moxifloxacin and Cefoperazone for the Treatment of Pneumonia in Buffaloes Praveen Kumar1*, V.K. Jain1, Tarun Kumar2, Parveen Goel1 and Neelesh Sindhu2 1Department of Veterinary Medicine, College of Veterinary Sciences, Lala Lajpat Rai University of Veterinary and Animal Sciences, Hisar, INDIA 2Veterinary Clinical Complex, Lala Lajpat Rai University of Veterinary and Animal Sciences, Hisar, INDIA *Corresponding author: P Kumar; Email: [email protected] Received: 05 March., 2018 Revised: 21 July, 2018 Accepted: 31 July, 2018 ABSTRACT A study was conducted to evaluate the comparative efficacy of kanamycin, enrofloxacin, moxifloxacin and cefoperazone to treat pneumonia in buffaloes. During study period, a total of 28 buffaloes brought to VCC, LUVAS, Hisar with the history of fever, anorexia, nasal discharge, coughing and dyspnoea. Clinical examination revealed abnormal lung sounds during auscultation. All the buffaloes diagnosed with pneumonia were randomly divided into four equal groups viz. group I, II, III and IV. Animals of group I were treated with kanamycin @ 7.0 mg/kg b.wt., i/m, b.i.d., group II with enrofloxacin @ 5 mg/kg b.wt., i/m, o.d., group III with moxifloxacin @ 5 mg/kg b.wt., i/m, o.d. and group IV with cefoperazone@ 20 mg/kg b.wt., i/m, o.d., along with supportive therapy for 5 days. Clinical recovery was determined on the basis of remittance of clinical signs. The highest and earliest recovery was found in group II animals. -

The Grohe Method and Quinolone Antibiotics
The Grohe method and quinolone antibiotics Antibiotics are medicines that are used to treat bacterial for modern fluoroquinolones. The Grohe process and the infections. They contain active ingredients belonging to var- synthesis of ciprofloxacin sparked Bayer AG’s extensive ious substance classes, with modern fluoroquinolones one research on fluoroquinolones and the global competition of the most important and an indispensable part of both that produced additional potent antibiotics. human and veterinary medicine. It is largely thanks to Klaus Grohe – the “father of Bayer quinolones” – that this entirely In chemical terms, the antibiotics referred to for simplicity synthetic class of antibiotics now plays such a vital role for as quinolones are derived from 1,4-dihydro-4-oxo-3-quin- medical practitioners. From 1965 to 1997, Grohe worked oline carboxylic acid (1) substituted in position 1. as a chemist, carrying out basic research at Bayer AG’s Fluoroquinolones possess a fluorine atom in position 6. In main research laboratory (WHL) in Leverkusen. During this addition, ciprofloxacin (2) has a cyclopropyl group in posi- period, in 1975, he developed the Grohe process – a new tion 1 and also a piperazine group in position 7 (Figure A). multi-stage synthesis method for quinolones. It was this This substituent pattern plays a key role in its excellent achievement that first enabled him to synthesize active an- antibacterial efficacy. tibacterial substances such as ciprofloxacin – the prototype O 5 O 4 3 6 COOH F COOH 7 2 N N N 8 1 H N R (1) (2) Figure A: Basic structure of quinolone (1) (R = various substituents) and ciprofloxacin (2) Quinolones owe their antibacterial efficacy to their inhibition This unique mode of action also makes fluoroquinolones of essential bacterial enzymes – DNA gyrase (topoisomer- highly effective against a large number of pathogenic ase II) and topoisomerase IV. -
![Bacterial Infection Imaging with [18F]Fluoropropyl-Trimethoprim](https://docslib.b-cdn.net/cover/1851/bacterial-infection-imaging-with-18f-fluoropropyl-trimethoprim-1771851.webp)
Bacterial Infection Imaging with [18F]Fluoropropyl-Trimethoprim
Bacterial infection imaging with [18F]fluoropropyl-trimethoprim Mark A. Sellmyera,1, Iljung Leea, Catherine Houa, Chi-Chang Wenga, Shihong Lia, Brian P. Liebermana, Chenbo Zenga, David A. Mankoffa, and Robert H. Macha,1 aDepartment of Radiology, University of Pennsylvania, Philadelphia, PA 19104 Edited by Joanna S. Fowler, Brookhaven National Laboratory, Upton, NY, and approved June 15, 2017 (received for review February 23, 2017) There is often overlap in the diagnostic features of common pathologic To address this clinical challenge, we sought to make a small- processes such as infection, sterile inflammation, and cancer both molecule PET probe to identify bacterial infection in vivo, which clinically and using conventional imaging techniques. Here, we report would not be confounded by chemical inflammation or cancer the development of a positron emission tomography probe for live (Fig. 1A). The probe is based on the synthetic antibiotic tri- bacterial infection based on the small-molecule antibiotic trimethoprim methoprim (TMP) that inhibits bacterial dihydrofolate reductase (TMP). [18F]fluoropropyl-trimethoprim, or [18F]FPTMP, shows a greater (dhfr), an enzyme in the DNA synthesis and folate pathway that is than 100-fold increased uptake in vitro in live bacteria (Staphylococcus conserved across most bacterial species including both Gram- aureus, Escherichia coli,andPseudomonas aeruginosa) relative to con- positive, Gram-negative, mycobacterial species such as Mycobac- 18 trols. In a rodent myositis model, [ F]FPTMP identified live bacterial terium tuberculosis and some parasites such as Toxoplasma gondii infection without demonstrating confounding increased signal in the (SI Appendix,Fig.S1) (6, 7). TMP has nanomolar affinity for dhfr same animal from other etiologies including chemical inflammation whereas it has micromolar affinity for human dihydrofolate re- (turpentine) and cancer (breast carcinoma). -

ARCH-Vet Anresis.Ch
Usage of Antibiotics and Occurrence of Antibiotic Resistance in Bacteria from Humans and Animals in Switzerland Joint report 2013 ARCH-Vet anresis.ch Publishing details © Federal Office of Public Health FOPH Published by: Federal Office of Public Health FOPH Publication date: November 2015 Editors: Federal Office of Public Health FOPH, Division Communicable Diseases. Elisabetta Peduzzi, Judith Klomp, Virginie Masserey Design and layout: diff. Marke & Kommunikation GmbH, Bern FOPH publication number: 2015-OEG-17 Source: SFBL, Distribution of Publications, CH-3003 Bern www.bundespublikationen.admin.ch Order number: 316.402.eng Internet: www.bag.admin.ch/star www.blv.admin.ch/gesundheit_tiere/04661/04666 Table of contents 1 Foreword 4 Vorwort 5 Avant-propos 6 Prefazione 7 2 Summary 10 Zusammenfassung 12 Synthèse 14 Sintesi 17 3 Introduction 20 3.1 Antibiotic resistance 20 3.2 About anresis.ch 20 3.3 About ARCH-Vet 21 3.4 Guidance for readers 21 4 Abbreviations 24 5 Antibacterial consumption in human medicine 26 5.1 Hospital care 26 5.2 Outpatient care 31 5.3 Discussion 32 6 Antibacterial sales in veterinary medicines 36 6.1 Total antibacterial sales for use in animals 36 6.2 Antibacterial sales – pets 37 6.3 Antibacterial sales – food producing animals 38 6.4 Discussion 40 7 Resistance in bacteria from human clinical isolates 42 7.1 Escherichia coli 42 7.2 Klebsiella pneumoniae 44 7.3 Pseudomonas aeruginosa 48 7.4 Acinetobacter spp. 49 7.5 Streptococcus pneumoniae 52 7.6 Enterococci 54 7.7 Staphylococcus aureus 55 Table of contents 1 8 Resistance in zoonotic bacteria 58 8.1 Salmonella spp. -

Effect of Meloxicam and Its Combination with Levofloxacin, Pazufloxacin, and Enrofloxacin on the Plasma Antioxidative Activity and the Body Weight of Rabbits
Veterinary World, EISSN: 2231-0916 RESEARCH ARTICLE Available at www.veterinaryworld.org/Vol.6/Dec-2013/1.pdf Open Access Effect of meloxicam and its combination with levofloxacin, pazufloxacin, and enrofloxacin on the plasma antioxidative activity and the body weight of rabbits Adil Mehraj Khan and Satyavan Rampal Department of Pharmacology and Toxicology, College of Veterinary Sciences, Guru Angad Dev Veterinary and Animal Sciences (GADVASU), Ludihana, Punjab, India Corresponding author: Adil Mehraj Khan, email: [email protected] Received: 25-09-2013, Revised: 12-10-2014, Accepted: 14-10-2013, Published online: 01-12-2013 doi: 10.14202/vetworld.2013.950-954 How to cite this article: Khan AM and Rampal S (2013) Effect of meloxicam and its combination with levofloxacin, pazufloxacin, and enrofloxacin on the plasma antioxidative activity and the body weight of rabbits, Veterinary World 6(12): 950-954. Abstract Aim: Evaluation of meloxicam, levofloxacin, pazufloxacin, and enrofloxacin for their effect on the plasma antioxidative activity (AOA) and the body weight in rabbits. Materials and Methods: Thirty two male Soviet Chinchilla rabbits were divided to eight groups of four rabbits each. Group A, serving as control, was administered 5 % dextrose. Group B, C, E and G were gavaged meloxicam, levofloxacin, pazufloxacin and enrofloxacin, respectively, in 5% dextrose. Levofloxacin and pazufloxacin were administered at the dose rate of 10 mg/kg body weight b.i.d 12h, whereas the meloxicam and enrofloxacin were administered at 0.2mg/kg body weight o.i.d and 20 mg/kg body weight, respectively. Groups D, F and H were co-gavaged meloxicam with levofloxacin, pazufloxacin, and enrofloxacin, respectively, at the above dose rates. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

Simultaneous Determination of the Residues of Fourteen Quinolones
Vol. 30, 2012, No. 1: 74–82 Czech J. Food Sci. Simultaneous Determination of the Residues of Fourteen Quinolones and Fluoroquinolones in Fish Samples using Liquid Chromatography with Photometric and Fluorescence Detection Florentina CAÑADA-CAÑADA, Anunciacion ESPINOSA-MAnsILLA, Ana JIMÉneZ GIRÓN and Arsenio MUÑOZ DE LA PeÑA Department of Analytical Chemistry, University of Extremadura, Badajoz, Spain Abstract Cañada-Cañada F., Espinosa-Mansilla A., Jiménez Girón A., Muñoz de la Peña A. (2012): Simul- taneous determination of the residues of fourteen quinolones and fluoroquinolones in fish samples using liquid chromatography with photometric and fluorescence detection. Czech J. Food Sci., 30: 74–82. A chromatographic method is described for assaying fourteen quinolones and fluoroquinolones (pipemidic acid, marbofloxacin, norfloxacin, ciprofloxacin, danofloxacin, lomefloxacin, enrofloxacin, sarafloxacin, difloxacin, oxolinic acid, nalidixic acid, flumequine, and pyromidic acid) in fish samples. The samples were extracted with m-phosphoric acid/acetonitrile mixture (75:25, v/v), purified, and preconcentrated on ENV + Isolute cartridges. The determina- tion was achieved by liquid chromatography using C18 analytical column. A mobile phase composed of mixtures of methanol-acetonitrile-10mM citrate buffer at pH 4.5, delivered under optimum gradient program, at a flow rate of 1.5 ml/min, allows accomplishing the chromatographic separation in 26 minutes. For the detection were used serial UV-visible diode-array at 280 nm and 254 nm and fluorescence detection at excitation wavelength/emission wavelength: 280/450, 280/495, and 280/405 nm. The detection and quantification limits were between 0.2–9.5 and 0.7–32 µg/kg, respectively. The procedure was applied to the analysis of spiked salmon samples at two different concentration levels (50 µg/k and 100 µg/kg). -
Summary Report (2)
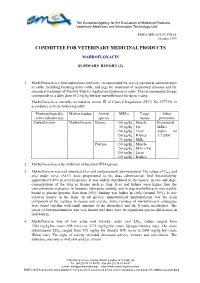
The European Agency for the Evaluation of Medicinal Products Veterinary Medicines and Information Technology Unit EMEA/MRL/693/99-FINAL October 1999 COMMITTEE FOR VETERINARY MEDICINAL PRODUCTS MARBOFLOXACIN SUMMARY REPORT (2) 1. Marbofloxacin is a fluoroquinolone antibiotic, recommended for oral or parenteral administration to cattle, including lactating dairy cattle, and pigs for treatment of respiratory diseases and for parenteral treatment of Mastitis Metritis Agalactiae syndrome in sows. The recommended dosage corresponds to a daily dose of 2 mg/kg bw/day marbofloxacin for up to 5 days. Marbofloxacin is currently included in Annex III of Council Regulation (EEC) No 2377/90, in accordance with the following table: Pharmacologically Marker residue Animal MRLs Target Other active substance(s) species tissues provisions Marbofloxacin Marbofloxacin Bovine 150 µg/kg Muscle Provisional 50 µg/kg Fat MRLs 150 µg/kg Liver expire on 150 µg/kg Kidney 1.7.2000 75 µg/kg Milk Porcine 150 µg/kg Muscle 50 µg/kg Skin + Fat 150 µg/kg Liver 150 µg/kg Kidney 2. Marbofloxacin acts by inhibition of bacterial DNA-gyrase. 3. Marbofloxacin was well absorbed after oral and parenteral administration. The values of Cmax and area under curve (AUC) were proportional to the dose administered. Oral bioavailability approached 100% in several species. It was widely distributed to the tissues. In rats and dogs, concentrations of the drug in tissues such as lung, liver and kidney were higher than the concentrations in plasma. In humans, laboratory animals and in pigs marbofloxacin was weakly bound to plasma proteins (less than 10%); binding was higher in cattle (around 30%).