BC First Nations Health Governance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Green Tech Exchange Forum
Green Tech Exchange Forum May 25, 2016 SFU Harbor Centre Presentation Chief Patrick Michell Kanaka Bar Indian Band “What we do to the lands, we do to ourselves.” The Indigenous People of Canada All diverse with distinct languages, culture and history. Canada • Celebrating 150 Years on July 1 2017 • 630 Bands • Metis and Inuit too British Columbia • Joined Canada in 1871 • 203 Bands The Nlaka’pamux Nation Archeology indicates an indigenous population living on the land for 7,000 years +. 1808: First Contact with French NWC with arrival of Simon Fraser. • First named Couteau Tribe. • Later renamed the Thompson Indian. 1857-58: Fought Americans to standstill in the Fraser Canyon War 1876: 69 villages amalgamated into 15 Indian Bands under the Indian Act 1878: Reserve Land allocations Kanaka Bar Indian Band • One of the original Nlaka’pamux communities. • Webpage: www.kanakabarband.ca • 66 members on reserve, 150 off • Codified: Election, Membership and Governance Codes in 2013. • Leadership: an indefinite term but face recall every 3rd Thursday. Land Use Plan (March 2015). Community Economic Development Plan (March 2016). Bi-annual implementation plans. Holistic: what one does affects another Kanaka Bar Indian Band Organization Chart As at May 2, 2016 Kanaka Bar & British Columbia Clean Energy Sectors Large Hydro Geothermal Tidal Wave N/A Applicable some day? N/A N/A Biomass Solar Run of River Wind Considered: not yet? 1.5 Projects 1.5 Projects Concept Stage How are we doing this? BC Hydro (the buyer of electrons) Self-sufficiency (off grid) Net Metering: projects under 100Kw Generating electrons for office, can connect to grid. -

To Read an Excerpt from Claiming the Land
CONTENTS S List of Illustrations / ix Preface / xi INTRODUCTION Fraser River Fever on the Pacific Slope of North America / 1 CHAPTER 1 Prophetic Patterns: The Search for a New El Dorado / 13 CHAPTER 2 The Fur Trade World / 36 CHAPTER 3 The Californian World / 62 CHAPTER 4 The British World / 107 CHAPTER 5 Fortunes Foretold: The Fraser River War / 144 CHAPTER 6 Mapping the New El Dorado / 187 CHAPTER 7 Inventing Canada from West to East / 213 CONCLUSION “The River Bears South” / 238 Acknowledgements / 247 Appendices / 249 Notes / 267 Bibliography / 351 About the Author / 393 Index / 395 PREFACE S As a fifth-generation British Columbian, I have always been fascinated by the stories of my ancestors who chased “the golden butterfly” to California in 1849. Then in 1858 — with news of rich gold discoveries on the Fraser River — they scrambled to be among the first arrivals in British Columbia, the New El Dorado of the north. To our family this was “British California,” part of a natural north-south world found west of the Rocky Mountains, with Vancouver Island the Gibraltar-like fortress of the North Pacific. Today, the descendants of our gold rush ancestors can be found throughout this larger Pacific Slope region of which this history is such a part. My early curiosity was significantly moved by these family tales of adventure, my great-great-great Uncle William having acted as fore- man on many of the well-known roadways of the colonial period: the Dewdney and Big Bend gold rush trails, and the most arduous section of the Cariboo Wagon Road that traversed and tunnelled through the infamous Black Canyon (confronted by Simon Fraser just a little over 50 years earlier). -

The Archaeology of 1858 in the Fraser Canyon
The Archaeology of 1858 in the Fraser Canyon Brian Pegg* Introduction ritish Columbia was created as a political entity because of the events of 1858, when the entry of large numbers of prospectors during the Fraser River gold rush led to a short but vicious war Bwith the Nlaka’pamux inhabitants of the Fraser Canyon. Due to this large influx of outsiders, most of whom were American, the British Parliament acted to establish the mainland colony of British Columbia on 2 August 1858.1 The cultural landscape of the Fraser Canyon underwent extremely significant changes between 1858 and the end of the nineteenth century. Construction of the Cariboo Wagon Road and the Canadian Pacific Railway, the establishment of non-Indigenous communities at Boston Bar and North Bend, and the creation of the reserve system took place in the Fraser Canyon where, prior to 1858, Nlaka’pamux people held largely undisputed military, economic, legal, and political power. Before 1858, the most significant relationship Nlaka’pamux people had with outsiders was with the Hudson’s Bay Company (HBC), which had forts at Kamloops, Langley, Hope, and Yale.2 Figure 1 shows critical locations for the events of 1858 and immediately afterwards. In 1858, most of the miners were American, with many having a military or paramilitary background, and they quickly entered into hostilities with the Nlaka’pamux. The Fraser Canyon War initially conformed to the pattern of many other “Indian Wars” within the expanding United States (including those in California, from whence many of the Fraser Canyon miners hailed), with miners approaching Indigenous inhabitants * The many individuals who have contributed to this work are too numerous to list. -

Farrell & Waatainen, 2020 Canadian Social Studies, Volume 51
Farrell & Waatainen, 2020 Canadian Social Studies, Volume 51, Issue No. 2 Face-to-Face with Place: Place-Based Education in the Fraser Canyon Teresa Farrell Instructor, Faculty of Education Vancouver Island University [email protected] Paula Waatainen Instructor, Faculty of Education Vancouver Island University [email protected] This work was supported by funding received from a Social Sciences and Humanities Research Council (SSHRC) Exchange Grant, a Vancouver Island University Innovate Grant, and funds from the Faculty of Education, Vancouver Island University. Two instructors from the Faculty of Education at Vancouver Island University organized a three-day field experience with 35 pre-service teachers along the Fraser Canyon corridor, home of the Nlaka’pamux and Stó:lō Nations. We asked: How will an educational field experience in this place impact and inform pre-service teachers and researchers’ understanding of place- based education (PBE) in their practice? We explore the shift towards Indigenous perspectives that subtly wove its way through the work and how it framed new ways of thinking about place for our participants and new ways of considering decolonizing education for the instructor researchers. We conclude by arguing that PBE is necessitated by active, living relationship in place and provides opportunities for critical pedagogy grounded in Indigeneity. We also suggest that both Indigenous and non-Indigenous educators have a role to play in this work. “Is it not time to face place – to confront it, take off its veil and see its full face.” (Johnson and Murton, 2007, p. 127). On September 12, 2019, two instructor researchers traveled with 35 pre-service teachers to a place that lived in our minds and hearts: the Fraser Canyon corridor1, in what is now British Columbia, Canada. -
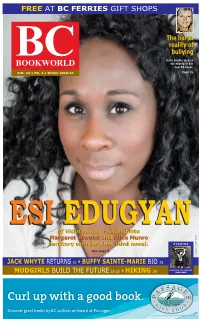
Esi Edugyan's
FREE AT BC FERRIES GIFT SHOPS TheThe harshharsh realityreality ofof BC bullying bullying Holly Dobbie tackles BOOKWORLD the misery in her new YA novel. VOL. 32 • NO. 4 • Winter 2018-19 PAGE 35 ESIESI EDUGYANEDUGYAN ofof VictoriaVictoria hashas rocketedrocketed intointo MargaretMargaret AtwoodAtwood andand AliceAlice MunroMunro PHOTO territoryterritory withwith justjust herher thirdthird novel.novel. STAMINA POPPITT See page 9 TAMARA JACK WHYTE RETURNS 10 • BUFFY SAINTE-MARIE BIO 25 PUBLICATION MAIL AGREEMENT BUILD THE FUTURE 22-23 • 26 MUDGIRLS HIKING #40010086 Curl up with a good book. Discover great books by BC authors on board at Passages. Orca Book Publishers strives to produce books that illuminate the experiences of all people. Our goal is to provide reading material that represents the diversity of human experience to readers of all ages. We aim to help young readers see themselves refl ected in the books they read. We are mindful of this in our selection of books and the authors that we work with. Providing young people with exposure to diversity through reading creates a more compassionate world. The World Around Us series 9781459820913 • $19.95 HC 9781459816176 • $19.95 HC 9781459820944 • $19.95 HC 9781459817845 • $19.95 HC “ambitious and heartfelt.” —kirkus reviews The World Around Us Series.com The World Around Us 2 BC BOOKWORLD WINTER 2018-2019 AROUNDBC TOPSELLERS* BCHelen Wilkes The Aging of Aquarius: Igniting Passion and Purpose as an Elder (New Society $17.99) Christine Stewart Treaty 6 Deixis (Talonbooks $18.95) Joshua -

1 SCT File No.: SPECIFIC CLAIMS TRIBUNAL BETWEEN: KANAKA
SCT File No.: SPECIFIC CLAIMS TRIBUNAL BETWEEN: KANAKA BAR INDIAN BAND Claimant v. HER MAJESTY THE QUEEN IN THE RIGHT OF CANADA As represented by the Minister of Indian Affairs and Northern Development Respondent DECLARATION OF CLAIM Pursuant to Rule 41 of the Specific Claims Tribunal Rules of Practice and Procedure This Declaration of Claim is filed under the provision of the Specific Claims Tribunal Act and the Specific Claims Tribunal Rules of Practice and Procedure. October 19, 2018 _________________________ (Registry Officer) TO: HER MAJESTY THE QUEEN IN THE RIGHT OF CANADA Assistant Deputy Attorney General, Litigation, Justice Canada Bank of Canada Building 234 Wellington Street East Tower Ottawa, Ontario K1A 0H8 Fax number: (613) 954-1920 1 I. Claimant 1. The Claimant, Kanaka Bar Indian Band (the “Band”) confirms that it is a First Nation within the meaning of s. 2 of the Specific Claim Tribunal Act (the “Act”) by being a “band” within the meaning of the Indian Act, R.S.C. 1985, c. I-5, as amended in the Province of British Columbia. II. Conditions Precedent (R. 41(c)) 2. The following conditions precedent as set out in s. 16(1) of the Act, have been fulfilled: 16. (1) A First Nation may file a claim with the Tribunal only if the claim has been previously filed with the Minster and (a) the Minister has notified the First Nation in writing of his or her decision not to negotiate the claim, in whole or in part; 3. On or about May 4, 2011, the Band filed a specific claim in respect to the illegal pre-emption in 1861 and subsequent alienation of a portion of the Band’s settlement at T’aqt’agtn (the “Claim”), now designated Lot 4, G.1, Kamloops Division of Yale Land District (“Lot 4”) with the Specific Claims Branch of the Department of Indian Affairs and Northern Development Canada. -

Art, Artist, and Witness(Ing) in Canada's Truth and Reconciliation
Dance with us as you can…: Art, Artist, and Witness(ing) in Canada’s Truth and Reconciliation Journey by Jonathan Robert Dewar A thesis submitted to the Faculty of Graduate and Postdoctoral Affairs in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Indigenous and Canadian Studies Carleton University Ottawa, Ontario © 2017, Jonathan Robert Dewar Abstract This dissertation explores, through in-depth interviews, the perspectives of artists and curators with regard to the question of the roles of art and artist – and the themes of community, responsibility, and practice – in truth, healing, and reconciliation during the early through late stages of the 2008-2015 mandate of the Truth and Reconciliation Commission of Canada (TRC), as its National Events, statement taking, and other programming began to play out across the country. The author presents the findings from these interviews alongside observations drawn from the unique positioning afforded to him through his professional work in healing and reconciliation-focused education and research roles at the Aboriginal Healing Foundation (2007-2012) and the Shingwauk Residential Schools Centre (2012-2016) about the ways art and artists were invoked and involved in the work of the TRC, alongside it, and/or in response to it. A chapter exploring Indigenous writing and reconciliation, with reference to the work of Basil Johnston, Jeannette Armstrong, Tomson Highway, Maria Campbell, Richard Wagamese, and many others, leads into three additional case studies. The first explores the challenges of exhibiting the legacies of Residential Schools, focusing on Jeff Thomas’ seminal curatorial work on the archival photograph-based exhibition Where Are the Children? Healing the Legacy of Residential Schools and Heather Igloliorte’s curatorial work on the exhibition ‘We were so far away…’: The Inuit Experience of Residential Schools, itself a response to feedback on Where Are the Children? Both examinations draw extensively from the author’s interviews with the curators. -

From Xwelítem Ways Towards Practices of Ethical Being in Stó:Lō Téméxw: a Narrative Approach to Transforming Intergenerational White Settler Subjectivities
From Xwelítem Ways Towards Practices of Ethical Being in Stó:lō Téméxw: A Narrative Approach to Transforming Intergenerational White Settler Subjectivities by Robyn Heaslip Master of Resource Management, Simon Fraser University, 2008 Bachelor of Science, University of Victoria, 2003 A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY in the Department of Indigenous Governance © Robyn Heaslip, 2017 University of Victoria All rights reserved. This dissertation may not be reproduced in whole or in part, by photocopy or other means, without the permission of the author. ii Supervisory Committee From Xwelítem Ways Towards Practices of Ethical Being in Stó:lō Téméxw: A Narrative Approach to Transforming Intergenerational White Settler Subjectivities by Robyn Heaslip Master of Resource Management, Simon Fraser University, 2008 Bachelor of Science, University of Victoria, 2003 Supervisory Committee Dr. Taiaiake Alfred, Indigenous Governance Program Supervisor Dr. Jeff Corntassel, Indigenous Governance Program Departmental Member Dr. Wenona Hall, Indigenous Studies, History, and Criminology Additional Member Dr. James Tully, Political Science, Law, Philosophy and Indigenous Governance Outside Member iii Abstract Supervisory Committee Dr. Taiaiake Alfred, Indigenous Governance Program Supervisor Dr. Jeff Corntassel, Indigenous Governance Program Departmental Member Dr. Wenona Hall, Indigenous Studies, History and Criminology Additional Member Dr. James Tully, Political Science, Law, Philosophy and Indigenous Governance Outside Member What must we transform in ourselves as white settlers to become open to the possibility of ethical, respectful, authentic relationships with Indigenous peoples and Indigenous lands? Situating this research in Stó:lō Téméxw (Stó:lō lands/world) and in relationships with Stó:lō people, this question has become an effort to understand what it means to be xwelítem and how white settlers might transform xwelítem ways of being towards more ethical ways of being. -
The Development of British Columbia
06_horizons2e_3rd.qxp 3/31/09 4:17 PM Page 204 The Development of 6 British Columbia Chapter Outcomes In this chapter, you will study the development of the province of British Columbia during the 19th century. By the end of the chapter, you will • assess the impact of the Cariboo Gold Rush on the development of British Columbia • identify factors that led to the expansion of Canada to include British Columbia, including issues involving the Oregon Territory • describe the shift in British Columbia’s trade patterns from north–south and overseas to east–west within Canada • evaluate the influence of immigration on the society of British Columbia, and relate the status of ethnic minorities to societal attitudes of the time • discuss the contributions of immigrants to Canada’s development • describe the components of the British Columbia provincial government 204 06_horizons2e_3rd.qxp 3/31/09 4:17 PM Page 205 Significance Patterns and Change Judgements CRITICAL Evidence INQUIRY Cause and Consequence Perspectives What led British Columbia to become a Canadian province? The Pacific Northwest was the last part of North America to be explored and settled by Europeans. What path did British Columbia follow compared with the other colonies in British North America? Who or what had the most influence on its development—individuals, groups, or environmental factors? Key Terms Oregon Territory Aboriginal title gold rush annexation Imagine being in the place of James Douglas, who in 1848 was appointed governor of the colony of Vancouver Island. Read his quote below, and discuss what his job might have included. How might he have related to the different people in his colony—the Chinese, for example, or the Songish, shown above? What challenges would he have faced? ...to create a great social organization, with all its civil, judicial, and military establishments, in a wilderness of forests and mountains, is a Herculean task. -

Colonialism, Capitalism, and the Rise of State Schooling in British Columbia, 1849-1900 Trent University
COLONIALISM, CAPITALISM, AND THE RISE OF STATE SCHOOLING IN BRITISH COLUMBIA, 1849-1900 A Thesis Submitted to the Committee on Graduate Studies in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in the Faculty of Arts and Science TRENT UNIVERSITY Peterborough, Ontario, Canada, Anishinaabe Territory © Copyright by Sean Carleton 2016 Canadian Studies Ph.D Graduate Program May 2016 ABSTRACT Colonialism, Capitalism, and the Rise of State Schooling in British Columbia, 1849-1900 Sean Carleton This dissertation examines the historical relationship between settler colonialism, capitalism, and the rise of state schooling in what is now known as British Columbia between 1849 and 1900. It aims to “unsettle” conventional views of Canadian schooling history by bringing accounts of Indigenous and non-Indigenous education into one analytical frame, and it shows how the state used different forms of schooling for both Indigenous and non-Indigenous children—company, common, public, mission, day, boarding, and industrial schools—to assist colonial-capitalist social formation in the Pacific Northwest. In combining interdisciplinary insights from Indigenous studies, historical materialism, political economy, and critical pedagogy, the dissertation highlights the ways in which state-supported schooling facilitated capitalist accumulation by colonial dispossession. The central argument of the dissertation is that between 1849 and 1900, colonial, provincial, and federal governments strategically took on greater responsibility for schooling as a way of legitimizing the state and supporting the emergence of a capitalist settler society. KEYWORDS: Settler Colonialism; Capitalism; Education; Indigenous Peoples; Violence; Indian Residential Schools; History; Political Economy; British Columbia; Canada. ii ACKNOWLEDGEMENTS I gratefully acknowledge the funding I received from the Social Sciences and Humanities Research Council of Canada (SSHRC) to complete this dissertation. -

Caa 2013 Paper Abstracts
CAA 2013 PAPER ABSTRACTS Bill Angelbeck, PhD University of British Columbia James Aimers Investigating the Array of Sites in the Kwoiek SUNY Geneseo Creek Valley: An Overview and Some Theorizing Ancient Mesoamerican Sexualities Implications for Mid-Fraser Archaeology The archaeological study of sex and sexuality Kwoiek Creek is the traditional territory of has emerged relatively recently out of feminist the Kanaka Bar Nlaka'pamux peoples, located and gender studies. In this paper I survey the midway between Boston Bar and Lytton on the current state of sexuality studies in archaeology west side of the Fraser River. The valley had generally and in Mesoamerica specifically. How largely been unexplored archaeologically, with have these studies helped us to understand the only a surficial studies of a few sites along its lives of people in the Mesoamerican past? I will confluence with the Fraser, while no sites had highlight some elements of sexuality studies that then documented in the valley itself. Here, I will have changed the way we see the lives of ancient present results from over four seasons of Mesoamericans, and areas where work remains investigations, initiated by and conducted with challenging and incomplete. The paper will end the Kanaka Bar First Nation. In so doing, we with a consideration of evidence for non- have recorded over thirty-three archaeological heteronormative behaviors and identities in sites, including a range of sites: large winter ancient Mesoamerica. This is a topic which is villages, mat lodge camps, isolated housepits, ignored by many archaeologists, but is essential hamlets, rock shelter camps, roasting pits, if we are to people the Mesoamerican past with pictograph panels, and a series of culturally something other than versions of ourselves. -
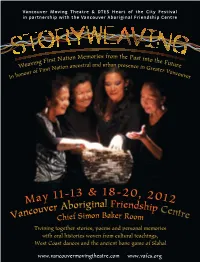
Storyweaving Program
Vancouver Moving Theatre & DTES Heart of the City Festival in partnership with the Vancouver Aboriginal Friendship Centre Memories from the irst Nation Past into th aving F e Futu We ation ancestral and urban presence in G re f First N reater V nour o anco In ho uver 18 ay 11-13 & -20, 2012 M Aboriginal Friendsh couver ip Cent Van Chief Simon Baker Room re Twining together stories, poems and personal memories with oral histories woven from cultural teachings, West Coast dances and the ancient bone game of Slahal www.vancouvermovingtheatre.com www.vafcs.org Storyweaving 1 Over half the population of the Lower Mainland has been here Vancouver Moving Theatre & Downtown Eastside Heart of the City Festival In partnership with Vancouver Aboriginal Friendship Centre, invite you to witness less than twenty years. Storyweaving They need to hear our stories. Weaving First Nation Memories from the Past into the Future His Honour Steven Point Inspired by Stories and Memories from Greater Vancouver’s Urban Aboriginal Community Lieutenant Governor of British Columbia Vancouver Aboriginal Friendship Centre (Stó:lō) Nation Chief Simon Baker Room, 1607 East Hastings Street, Vancouver, BC May 11-13 & May 18-20, 2012 Fridays and Saturdays 7:30pm, Sunday Matinees 2pm POST SHOW DISCUSSIONS Sunday May 13 and Sunday May 20 Angela White, Indian Residential School Survivors Society Renae Morriseau, Director Spiritual and emotional support during the event is provided by the Indian Residential School Survivors Society. The event is approximately two hours long. There is no intermission. Washrooms are down the hall to the west.